
Sealant Usage
Dimensions of Dental Hygiene speaks with Steven M. Adair, DDS, MS, from the Medical College of Georgia in Augusta, about sealant use—from tooth evaluation to clinical placement.
What criteria for sealant placement are used when evaluating the need for dental sealants?
Caries risk assessment is the first step, which is based on factors such as previous caries experience and the patient’s diet, fluoride exposure, and oral hygiene habits. First, determine whether this is a patient at risk for dental caries, then focus on the individual teeth. Perform a risk assessment of individual teeth based on the morphology of the pits and fissures, their extent and depth, whether there’s already caries activity, and the pattern of dental decay in the mouth in general. Sealants are recommended for placement on teeth that have enamel caries, are questionable for decay, or are caries free but at risk for caries. Questionable teeth may have fissures that are stained but not particularly sticky and rather noticeable pits that are soft.
What is the outcome when a tooth with undetected active decay is sealed?
Research1-3 shows that if the sealant remains intact—and that’s a big “if” in a clinical situation—then the caries process stops because the microorganisms are cut off from their nutrient supply in the oral cavity. This type of procedure is termed a therapeutic sealant as opposed to a preventive sealant. Most clinicians avoid sealants when decay is present, especially when the caries has penetrated the dentin. When dentists are opening the pits and fissures slightly with a small bur or by air abrasion, they are using therapeutic sealants. Knowing that the caries process stops when the tooth is sealed is important because it alleviates the fear of sealing over caries and having it progress. However, the hygienist and the dentist must be diligent in checking and repairing the sealants at frequent intervals—at least every 6 months.
A sealant is not recommended if a proximal restoration or lesion is present. This would involve a restoration that obliterates the fissures. However, we do teach sealing over occlusal restorations to reduce microleakage and prolong the longevity of amalgam composite and glass ionomer-type occlusal restorations. Studies4,5 done here at the Medical College of Georgia that looked at sealing restorations—both composite resin and amalgam—found that sealants are effective in reducing microleakage and recurrent caries. This is done immediately after placement of the restoration.
Are sealants for children only?
No, sealants are for any caries susceptible individual with a tooth that has pit and fissure morphology that makes it caries susceptible.
Primary teeth have flat occlusal surfaces so they don’t require sealants as often, but if the individual and the tooth risk assessment suggest that a primary tooth is susceptible to pit and fissure caries, there is no reason not to seal unless the lifespan of the tooth is relatively short. If root resorption has progressed where the tooth will exfoliate in 6 months, sealing it is not beneficial.
Research4,5 shows that the progression of dental caries is slowing down in the population. Lesions that may have taken 3 or 4 years to show up in a newly erupted permanent molar are now taking longer to appear due to increased fluoride exposure. Almost everyone uses fluoride toothpaste and many processed foods and beverages contain some level of fluoride as well. Previous opinion dictated that if a permanent molar was in the mouth more than 3 years and did not decay, then it was not likely to decay. Therefore, even if it looked susceptible, there was no reason to put on a sealant. Now we are sealing susceptible looking teeth no matter what the age of the patient.
How effective are sealants in preventing pit and fissure decay?
In the early days of sealants, the research was based on half-mouth studies, where teeth on one side of the mouth got sealants and teeth on the other side did not. A mathematical formula was then used to decide how many surfaces of decay were saved by sealant placement. Once it was shown that sealants were effective, this type of research could no longer be conducted because of the ethical obligation to put sealants on all susceptible teeth. Today sealant effectiveness is basically equated with sealant retentiveness. Retained sealants are likely to be effective. Studies6 show that about 85% to 90% of sealants are still intact after 1 year. Sealants that are partially lost may be as likely to decay as teeth with completely lost sealants.
What is the longevity of a sealant?
A study7 looked at first and second molars that were sealed for 15-20 years. The only time a sealant was replaced was on the first molar when the patient came in to have the second molar sealed. The second molar sealants were never replaced. After 15 or 20 years, the sealants were completely maintained on 65% of the first molars and 65% of the second molars. In the first year or so about 10% to 15% are lost. Then the retention rate drops down to about 70% at 3 years. Most of the studies6 go back 6 or 7 years and show complete retention rates at 65% and 70%. A fully retained sealant is intact and maybe a little worn, but not a fragment. The pits and fissures are still sealed.
What percentage of sealed teeth decay?
After 1 year, the percentage is around 5% or so and climbs to about 20% from 1 to 4 years.6 The caries occurs because the sealant is lost or at least partially lost. These are teeth that were sealed but not resealed. Subsequently, the sealant or some of the sealant is lost and the tooth decays. Retention starts out high and then level off at 65%. In sealed teeth that decay, the percentage starts out low, perhaps at 5%, and gets up to 30%.
When an adult patient presents with lost or partially lost sealants from childhood, what is the treatment?
The hygienist must do another risk assessment. Maybe this patient’s diet is under better control and his oral hygiene is improved. You can’t assume that because a tooth was considered at risk when the patient was 12 that 20 years later the tooth is still at risk. The risk for dental caries can change.
What is the treatment of choice for a broken sealant?
With a pediatric patient, I would reseal the tooth rather than remove the sealant even if the patient is no longer at high risk. In an attempt to remove a sealant with a rotary instrument, damage to the enamel could occur and leave the tooth more susceptible to decay. If the sealant is completely lost, a risk assessment should be done. Some speculate that even though the hygienist can’t detect the sealant, there may be some sealant present at the base of the pits and fissures. If the hygienist determines the tooth is at risk, relying on a little bit of sealant being left in the base is inadvisable. On the other hand, it could protect patients who have lost a sealant and can’t see a dentist for several months.
 |
The fissure pattern and “frosted” appearance are evident on this molar that has been etched and dried prior to sealant placement. |
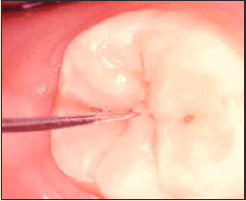 |
Careful visual and tactile evaluation of the pit and fissure systems aids in the determination of the caries risk of individual teeth. |
 |
Newly placed sealant on a permanent mandibular right first molar that has been isolated by rubber dam for a restorative procedureon the same molar. |
What methods are best in evaluating for decay under a sealant?
Careful evaluation of bitewing radiographs, looking around the margin of the sealant for obvious gaps, and chalky appearance of decalcified enamel are the clues for decay under sealants. Obviously, sealant loss or partial loss that leads to a ledge or other type of plaque trap should raise concerns as well.
What are the advantages of using glass ionomer sealants?
Glass ionomer can be effective when trying to seal a partially erupted or newly erupted molar that is difficult to isolate. Glass ionomers, since they don’t rely on a micromechanical bond like composites but rather on kelation, bond in a moist environment. This allows enough time to pass in order for the tooth to fully erupt so it can be isolated.
What other types of sealants are available?
A variety of resin, composite-based sealants are available. In this category, there are unfilled sealants, filled sealants, and flowable composites. Flowable composites are somewhere between not filled and highly filled sealant materials. In addition, color-changing sealants are available. At least one dental manufacturer makes a sealant that goes on pink and then once it’s cured, it becomes tooth colored. Another company offers sealant material that becomes visible under a curing light. This enables the hygienist to check for sealant failure. Fluoride releasing sealants are also available, however, resin composite materials release substantially less fluoride than glass ionomers.
When would you recommend using a fluoride varnish instead of a sealant?
The only time I would choose a fluoride varnish over a sealant for treatment or prevention of pit and fissure decay is with a partially erupted molar that I can’t isolate well enough to place a good sealant. I would consider a glass ionomer sealant or treat the occlusal surface with fluoride varnish, which only requires some degree of isolation. Like other fluoride modalities, fluoride varnish is most effective on smooth surfaces. So it may be a stopgap measure for pit and fissure management until the tooth is fully erupted and a sealant can be placed. The reapplication of varnish as a means to control pit and fissure caries is a more expensive method in the long run when compared to placing a sealant.
What are the important steps in the clinical placement of sealants?
Good diagnosis is number one—determining whether the tooth is sound or caries susceptible, questionable, or having enamel caries. Isolation is second, making sure that saliva is controlled and off the tooth. Acid etching is next and typically accomplished in about 15 seconds. It is important to etch a larger surface area than the surface to be sealed so the margin of your sealant will end in that etched enamel. Do not apply sealant materials beyond the etched area where it won’t be retentive.
Another important step is placing a bonding agent on the enamel after it has been etched—even if it comes in contact with saliva. Studies8 show that drying the tooth off and etching again are not necessary. If the sealant becomes contaminated, just place a bonding agent on the tooth and place the sealant on top of the bonding agent and cure the two together. Some clinicians use bonding agents almost routinely after they etch the tooth and prior to placement of the sealant. This obviously adds some expense to the sealant procedures but the retention rates are greatly improved.
Another product contains self-etching primer and adhesive that comes in one unit. This allows the clinician to place the material on the tooth in one step. Then the material is air thinned slightly and the sealant is placed. It removes the step of having to rinse and dry it again. This adds expense but reduces the number of steps.
Once you have the sealant in place, effective light curing is important. Make sure you understand the light requirements to cure the sealant and cure it according to the manufacturer’s specifications.
One of our residents just finished a research project with a dental materials faculty member that looked at sealant curing with different kinds of lights. They found that the blue LED light was very effective in curing the sealant in about 5 seconds as opposed to the standard 20 seconds. This can save a lot of time over a day of placing sealants. The blue LED lights are more costly, but speed is an advantage.
Does the dental hygienist need to be concerned with overfill?
If the hygienist is using a filled sealant, particularly a flowable composite, then checking and adjusting the occlusion is important. Filled sealants won’t wear down as quickly as lightly filled or not filled sealants. In the future, I would like to research whether adjusting the occlusion somehow affects the bond. Can the vibration on a newly cured sealant somehow disrupt the bond of the enamel? In our clinical observation, the bond appears unaffected. Patients can experience some sensitivity if the sealant is filled too high and doesn’t wear down quickly. If the hygienist is using this type of material, she needs to be aware of this issue and discuss it with the dentist. She must be careful not to overfill the occlusal surface with the sealant.
Are there any advantages in using filled sealants over unfilled?
I am not aware of studies showing that filled sealants are more retentive or have better caries reduction properties than unfilled. I don’t think there is a real advantage as they all wear away to some extent. I don’t believe the unfilled sealants are any less retentive. Some may suggest that unfilled sealants, being less viscous, might actually flow into pits and fissures better. Empirically this makes sense but I haven’t seen proof in the literature.
Are there indications for full mouth sealants?
If the patient is deemed caries susceptible and at risk for dental decay, then you evaluate tooth by tooth and make your decision. Sealants are relatively noninvasive but sealing every tooth in the mouth is very expensive and may not be necessary.
Sealants can be lost or partially lost, which can inadvertently predispose a tooth to caries. When I talk about sealants at continuing education courses, I hear one or two clinicians who say, “I’m seeing a lot of decay under my sealants.” What they seem to be saying is that the tooth was caries free and then they put a sealant on it and it decayed. Basically, this tells me that something is wrong with their technique. They didn’t get it sealed well, which can happen to anybody. Remember that the evaluation of sealants at follow-up appointments is equally important as the technique and placement.
References
- Handelman SL, Leverett DH, Solomon ES, Brenner CM. Use of adhesive sealants over occlusal carious lesions: radiographic evaluation. Community Dent Oral Epidemiol. 1981;9(6):256-259.
- Handelman SL, Leverett DH, Espeland M, Curzon J. Retention of sealants over carious and sound tooth surfaces. Community Dent Oral Epidemiol. 1987;15(1):1-5.
- Mertz-Fairhurst EJ, Schuster GS, Fairhurst CW. Arresting caries by sealants: results of a clinical study. J Am Dent Assoc. 1986;112(2):194-197.
- Mertz-Fairhurst EJ, Curtis JW Jr, Ergle JW, Rueggeberg FA, Adair SM. Ultraconservative and cariostatic sealed restorations: results at year 10. J Am Dent Assoc. 1998;129(1):55-66.
- Mertz-Fairhurst EJ, Adair SM, Sams DR, et al. Cariostatic and ultraconservative sealed restorations: nine-year results among children and adults. ASDC J Dent Child. 1995;62(2):97-107.
- Weintraub JA. The effectiveness of pit and fissure sealants. J Public Health Dent. 1989;49(5 Spec No):317-330.
- Wendt LK, Koch G, Birkhed D. On the retention and effectiveness of fissure sealant in permanent molars after 15-20 years: a cohort study. Community Dent Oral Epidemiol. 2001;29(4):302-307.
- Feigal RJ, Hitt J, Splieth C. Retaining sealant on salivary contaminated enamel. J Am Dent Assoc. 1993;124(3):88-97.
From Dimensions of Dental Hygiene. September 2003;1(5):22, 24, 26, 28.

