SARS—Confronting the Coronavirus
Understanding the detection, distribution, etiology, and case definition of Severe Acute Respiratory Syndrome is integral to maximizing infection control in the face of respiratory transmission.
Understanding the detection, distribution, etiology,and case definition of Severe Acute Respiratory Syndrome is integral to maximizing infection control in the face of respiratory transmission.
A previously undetected, life-threatening respiratory disease emerged on a worldwide scale in late 2002. This transmissible infection, termed Severe Acute Respiratory Syndrome (SARS), initially did not have an identifiable etiologic agent. The rapid spread of cases from Guangdong province in China to Hong Kong, Vietnam, Canada, and other countries1-3 caught global public health agencies by surprise. Fortunately, once jointly mobilized to utilize maximal resources, the World Health Organization (WHO) and other governmental health agencies were able to delineate the viral etiology, geographic sources, and epidemiologic factors that contributed to the spread of SARS. As a result, current efforts at diagnosing and ultimately controlling the epidemic have become more effective.
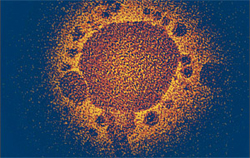
Figure 1.The genus that causes SARS—the coronavirus
SARS Defined
As the name implies, SARS is a previously unknown, febrile, respiratory illness that can progress from relatively mild flu-like symptoms to a potentially fatal pneumonia. Primary transmission of the causative virus appears to be through droplet and airborne mechanisms, although other mechanisms, ie, fecal, oral, have not been completely ruled out. Respiratory transmission is probably the major reason the spread of suspected and diagnosed cases was so rapid, as undiagnosed infected persons traveled from China and Hong Kong via airplanes to other susceptible countries.
Detection and Global Distribution
The development of improved epidemiological surveillance coupled with sophisticated, sensitive microbiological and immunological assays have allowed public health professionals to detect unusual infectious disease cases at earlier stages of suspected outbreaks. With regard to respiratory infections such as influenza, initial surveillance has often focused on the areas in Asia, where close proximity of humans and animals has been shown to cause “jumps” from one species to another and genetic nucleic acid changes in certain viruses. Consequently, the emergence of new potential pathogenic strains is not uncommon.4,5
In late 2002, reports of an unusual, life-threatening respiratory illness were detected in Guangdong province in China, Hong Kong, and Vietnam, followed soon thereafter by the subsequent spread of similar cases to Canada, the United States, and other countries by March 2003. Early information collected by WHO and Centers for Disease Control and Prevention (CDC) indicated the suspected infection was readily spread to both household family members and health care workers who came into contact with hospitalized patients.5,6 The observation that the causative microbe could apparently be transmitted to physicians and nurses caring for persons with SARS, sparked not only a massive worldwide effort to solve this new disease problem, but also fear within the general population and even among many health professionals. News photos and video tapes showing large groups of people wearing surgical masks while traveling or performing everyday tasks fed a noticeable public uneasiness. Fortunately, the application of good science, clinical medicine, and effective infection control precautions were able to dramatically curtail the rapid spread of SARS. Yet the WHO reported more than 8,400 documented cases as of July 11, 2003.7
Coronavirus—The Etiology of SARS
Prior to the SARS outbreak, three groups of coronaviruses (corona for the crown-like appearance of viral surface projections, see Figure 1) had previously been isolated and studied. Although some of these single-stranded RNA viruses are able to cause gastroenteritis, this genus is primarily known to cause respiratory tract infections similar to the common cold in humans and certain domestic animals. Specimens containing most corona- virus isolates grown in tissue culture were originally recovered from adult patients who were symptomatic of upper respiratory tract illness. Coronavirus respiratory infections have been found throughout the world, often occurring more frequently in the winter and spring than summer or fall.8 If this sounds very similar to what was observed in the current epidemic, it should be.
The historical lessons learned about coronaviruses greatly assisted in the search for a specific SARS etiology. Tissue cultures seeded with throat swab specimens from suspected patients were initially used to grow and amplify viral particles, followed by electron microscopy (EM) analysis to determine the ultrastructural characteristics of the virus. The early description of the classic “crown-like” appearance of the observed corona- viruses by EM was an essential step in the rapid progression toward defining this genus as the etiologic agent. Subsequent immunological assays confirmed the presence of a new, unique type of coronavirus called SARS-associated coronavirus (SARS-CoV). Genetic sequencing analysis of the nucleic acid has shown that SARS-CoV may be quite different from previously discovered strains. These data could partially explain why the SARS virus is capable of acting as a more virulent pathogen.9
Cumulative number of reported probable cases of SARS from November 1, 2002 to July 11, 2003
Current Case Definition For SARS
An abbreviated version of the updated version of the CDC case definition is included to provide major points. The complete document is available on the CDC website.7
Clinical Criteria:
- Asymptomatic or mild respiratory illness
- Moderate respiratory illness
- Temperature of > 100.4 F (> 38 C) and one or more clinical findings of respira– tory illness (eg, cough, shortness of breath, difficulty breathing , or hypoxia), and radiographic evidence of pneumonia or
- Respiratory distress syndrome or
- Autopsy findings consistent with pneumonia or respiratory distress syndrome without an identifiable cause
Epidemiologic Criteria:
- Travel, including transit in an airport, within 10 days of onset of symptoms to an area with current or previously documented or suspected community transmission of SARS or
- Close contact* within 10 days of onset of symptoms with a person known or suspected to have SARS.
*Defined as have cared for or lived with a person known to have SARS or having a high likelihood of direct contact with respiratory secretions and/or body fluids of a patient known to have SARS. Examples include kissing, embracing, sharing eating or drinking utensils, close conversation (<3 feet), physical examination, and any other10 direct physical contact between persons).
Laboratory Criteria:
Confirmed:
- Detection of antibody to SARS-CoV in a serum sample or
- Detection of SARS-CoV RNA reverse transcription-polymerase chain reaction (RT-PCR) confirmed by a second PCR assay or
- Isolation of SARS-CoV
Case Classification:
- Probable case: meets the clinical criteria for severe respiratory illness of unknown etiology and epidemiologic criteria for exposure; laboratory criteria confirmed or unconfirmed.
- Suspect case: meets the clinical criteria for moderate respiratory illness of unknown etiology and epidemiologic criteria for exposure; laboratory criteria confirmed or unconfirmed.
Even though the above criteria use a number of sensitive serological assays to assist in a SARS diagnosis, much work remains to develop a sensitive test to routinely detect SARS-CoV in a patient with symptomatic infection. The current status of confirming a diagnosis therefore primarily remains clinical. 5
SARS-CoV Transmission
The most common mode of viral spread is via close person-to-person contact, such as sneezing or coughing. Cross-infection of large droplets generated from the respiratory tract of infected persons appear to be important when a susceptible person is in close proximity to allow SARS-CoV to enter the respiratory tract. Other suggestions persist that the virus is also spread by micro-droplet nuclei of <10 um in diameter, in a similar manner as influenza and tuberculosis,4 along with the possibility of some unknown form of indirect transmission.11 Preliminary data suggests that the virus is able to survive for up to 3 hours on inanimate surfaces,7 although routine use of low- to intermediate-level disinfectants are recommended for decontamination of environmental surfaces. One example that reinforces possible indirect viral transmission from fomites comes from the fact that rhinoviruses, which cause the common cold, can be passed to susceptible persons from inanimate surfaces contaminated with respiratory secretions from a person with a symptomatic infection.
The unusually rapid spread of SARS coupled with investigations tracking paths of multiple infections associated with a specific person have led investigators to believe that some individuals can serve as “super shedders.” These people may either be infected with a more virulent strain of virus or their particular infection may cause them to be more capable of shedding infectious virions for longer periods to those with whom they come in close contact.
The SARS-CoV Course of Infection
The severity of disease after viral infection in a susceptible host can be variable with most patients recovering from the disease. The incubation period typically is 3-7 days, but could take up to 10 days. Early manifestations begin with abrupt onset of fever of 100.4 F or more and these are often accompanied by flu-like symptoms such as chills, headache, malaise, and muscle aches. Patients who progress to SARS subsequently develop a dry cough and sore throat. Worsening respiratory failure from resultant pneumonia can require mechanical ventilation.
Appropriate isolation precautions are required in hospitals for all patients suspected of or diagnosed with SARS, partially because high viral loads can be demonstrated in patients’ sputum up to 9 days after illness ensues. Despite treatment with a vast array of antiviral agents, at the present time no effective curative drug has been found, and 5%-10% of those whose infection progresses to SARS die. Cumulative reports from affected countries also indicate that persons with compromised immune defenses are most at risk for death from SARS.5
Efficacy of Current Infection Control Respiratory Precautions
At the present time, dental personnel have not been shown to have an increased occupational risk for SARS. The CDC and other health organizations continue to recommend that dental health care workers routinely use standard infection control precautions during provision of routine patient care. These precautions are second nature to most dental hygienists, including the use of personal protective equipment (gloves, masks, eyewear, protective clinic jackets, lab coats, or gowns), appropriate cleaning and sterilization of items that are reprocessed, and effective cleaning and disinfection of environmental surfaces. Rigorous compliance to hand hygiene protocols using either antiseptic agents with water or waterless hand hygiene products is imperative. When providing care to a patient exhibiting symptoms that may be suspicious for SARS, the use of N-95 disposable respirators provides better respiratory protection than regular surgical masks. These respirators have been effectively used in hospitals when health care workers come into contact with patients who have active tuberculosis (TB) in TB isolation rooms, when transporting TB cases, or in other treatment areas of the facilities. The better fit to the face and their ability to filter at least 95% of airborne particles 0.1 u in size allows the N-95 masks to more efficiently minimize passage through of microbes in airborne droplets. Masks that are able to filter down to 0.1 u can prevent much more potential exposure than masks that remove particles 1 or 3.0 – 3.2 u in diameter.
Summary
The emergence of SARS is only the latest reminder of how important an effective infectious disease surveillance network can be. In today’s world, microbial agents can rapidly spread to virtually any area of the world either by symptomatic or asymptomatic infected persons. The keys for clinicians in confronting and addressing SARS are not unlike those for other infections, such as influenza, TB, West Nile, or even HIV infection. These include early detection of cases, containment of infectious individuals, and use of appropriate infection control precautions to protect health professionals treating patients. An encouraging piece of information to come out of the SARS investigations is that despite its respiratory mode of transmission, SARS-CoV has not caused a worldwide pandemic with hundreds of thousands of cases. Much work needs to be done, but fortunately the precautions many of you are familiar with also appear to be protecting us against a wide variety of potential occupational pathogens.
References
- Outbreak of severe acute respiratory syndrome—worldwide, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(11):226-228.
- Update: Outbreak of severe acute respiratory syndrome—worldwide, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(12):241-246, 248.
- Update: Severe acute respiratory syndrome—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(16):357-360.
- Wenzel RP,EdmondMB. Managing SARS amidst uncertainty. New Engl J Med. 2003;348:1947-1948.
- Drazen JM. SARS—Looking back over the first 100 days. New Engl J Med. 2003;349:319-320.
- Severe acute respiratory syndrome (SARS). Wkly Epidemiol Rec. 2003;78:81-83.
- Centers for Disease Control and Prevention. Severe Acute Respiratory Syndrome (SARS). Available at: www.cdc.gov/ncidod/sars/index.htm. AccessedAugust 15, 2003.
- McIntosh K. Coronaviruses. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. Philadelphia: Churchill Livingstone; 2000:1767-1770.
- Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. New Engl J Med. 2003;348:1953-1966.
- Centers for Disease Control and Prevention. Severe Acute Respiratory Syndrome (SARS) Report of Cases in theUnited States. Available at: www.cdc.gov/od/oc/media/sars/cases.htm. AccessedAugust 15, 2003.
- Poutanen SM, Low DE, Henry B, et al. Identification of severe acute respiratory syndrome in Canada. New Engl J Med. 2003; 348:1995-2005.
From Dimensions of Dental Hygiene. September 2003;1(5):16, 18-20, 40.

