
Root Coverage Therapy
Jonathan H. Do, DDS, shares his perspective on surgical approaches and patient selection criteria for this approach to treating gingival recession.

Whether due to aggressive toothbrushing, trauma or periodontal diseases, gingival recession is frequently encountered in dental practice. Dimensions of Dental Hygiene asked Jonathan H. Do, DDS, of the University of California, Los Angeles, School of Dentistry to share his perspective on surgical approaches and patient selection criteria for root coverage therapy.
Editor’s Note: The views expressed in this interview are the author’s.
Clinicians can choose from a number of root coverage techniques. Will you briefly describe these procedures?
Free gingival grafts are indicated for narrow, isolated recession defects in nonesthetic areas. The palate serves as the donor for a free gingival graft that is placed on a deepithelialized recipient bed at the defect site. The survival of the graft depends on intimate contact between the donor tissue and vascular recipient bed. Thin free gingival grafts are susceptible to necrosis and sloughing, while thick free gingival grafts—which have higher survival rates— result in large and slow-healing donor sites. While this technique increases the amount of keratinized tissue at the defect site, the color match between the newly acquired and surrounding tissues may be poor.
Laterally positioned flaps are indicated for narrow, isolated recession defects on mandibular teeth. It is a technique in which the tooth adjacent to the recession serves as the donor for a flap that is laterally positioned to cover the defect. This procedure, because it can cause recession at the donor tooth, is only recommended when the tissue adjacent to the defect is thick and keratinized.
Coronally advanced flaps are most appropriate for treating patients with shallow recession (≤ 4 mm), thick existing tissue biotype (≥ 1 mm), and a broad zone of existing keratinized tissue (≥ 3 mm). Two vertical incisions bordering the papillae adjacent to the recession area are connected with a reverse-bevel scalloped incision along the gingival margin. A full-thickness mucoperiosteal flap is elevated. The periosteum of the flap is released at the base with a horizontal incision, and the flap is coronally positioned to cover the recession. This technique does not increase keratinized tissue, and may be susceptible to flap retraction and relapse of the recession.
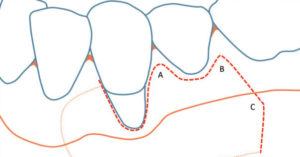
Subepithelial connective tissue grafts—when used with a bilaminar technique—are the gold standard for root coverage in terms of predictability, percentage of coverage, and long-term stability. The original Langer and Langer technique involves preparing a recipient site with a partial-thickness flap created by two vertical incisions placed at least one-half to one tooth wider mesiodistally than the area of gingival recession, and connected by a reverse-bevel horizontal incision at the level of the cementoenamel junction. A free subepithelial connective tissue graft is harvested from the palate and sutured over the denuded root surfaces. The outer partial-thickness flap is coronally positioned and sutured to cover as much of the connective tissue graft as possible (without completely covering it). More recently, the subepithelial connective tissue graft has been combined with partial- and full-thickness pouches, tunnels, and pedicle flaps (Figures 1 through Figure 5), all in bilaminar techniques with a dual blood supply.
Acellular dermal matrix is an allograft obtained from human dermis harvested and processed to remove all cells (while preserving the intact extracellular matrix). An acellular dermal matrix can be used as donor tissue in lieu of a connective tissue graft. It can be combined with a pouch, tunnel, or coronally advanced flap technique in patients who have limited donor connective tissue volume in the palate or who simply do not want a second wound at the donor site. Exposure of the acellular dermal matrix following the procedure may result in infections and compromised healing.
Enamel matrix derivative is a biologic (derived from natural sources and composed of sugars, proteins, nucleic acids, or actual living substances, such as cells and tissues) obtained from porcine fetal teeth. When used with a coronally advanced flap and/or connective tissue graft, enamel matrix derivative may enhance soft tissue healing and root coverage.
Guided tissue regeneration uses bioabsorbable or nonresorbable membranes—in combination with bone substitutes, biologics, and coronally advanced flaps—can be used in an attempt to regenerate the lost periodontium. The outcome of guided tissue regeneration can be unpredictable, however, and depends largely on the clinician’s technique.

VISTA is an acronym for vestibular incision subperiosteal tunnel access, and is a technique utilizing a vertical incision in the vestibule, away from the recession area, to provide access for full-thickness soft tissue elevation and insertion of graft materials, acellular dermal matrix, or a connective tissue graft. The outer tissue is coronally advanced and stabilized with suspensory sutures. This is a bilaminar technique using a dual blood supply.
Pinhole surgical technique uses a remote puncture in the vestibule away from the recession area to obtain access for full-thickness soft tissue elevation, and insertion of resorbable collagen graft materials. Because sutures are not used, this technique depends on the graft materials to coronally advance and stabilize the outer soft tissue. The pinhole surgical technique may be indicated when the recession is shallow and the existing soft tissue is thick, with a broad zone of keratinized tissue.
Please explain the criteria for patient selection when considering root coverage procedures.
The selection criteria for root coverage procedures is similar to any elective surgical treatment. Here are factors that must be taken into account.
Systemic health. Patients should be in good health, and systemic conditions must be under control. Patients with poorly controlled diabetes, for example, are at increased risk for post-operative infections, delayed healing, and necrosis of tissue at the donor and recipient sites.

Smoking. Following surgery, smoking may result in compromised healing. Necrosis and sloughing of donor tissue, and delayed wound healing at the donor and recipient sites are commonly seen in patients who smoke. These individuals should be informed of the risks and benefits of treatment, as well as alternatives. If possible, smoking should be avoided (or at least minimized) for 2 weeks post-surgery to avoid complications.
Patient education and oral hygiene. Whether it stems from a periodontal disease, aggressive toothbrushing, or other oral habits, patients should be educated about the etiology of their particular condition. Patients must have excellent and minimally traumatic biofilm control, and should be instructed to modify habits that may contribute to gingival recession.
Recession type. Gingival recession is commonly categorized using the Miller Classification system.
- Miller Class I: Gingival recession does not extend to the mucogingival junction, and there is no loss of interdental tissue.
- Miller Class II: Recession extends to or beyond the mucogingival junction, with no loss of interdental tissue.
- Miller Class III: The recession extends to or beyond the mucogingival junction, and the loss of interdental tissue is coronal to the apical extent of the defect; in addition, the dentition may be malposed.
- Miller Class IV: The defect extends to or beyond the mucogingival junction, and the loss of interdental tissue reaches the apical extent of the gingival recession; the dentition may also be malposed.
Following therapy, complete root coverage may be expected in patients with Miller Class I or II defects. In patients with Miller Class III or IV defects, however, complete root coverage cannot be anticipated. Nevertheless, patients with Miller Class III or IV defects and limited keratinized tissue may benefit from soft tissue augmentation to facilitate oral hygiene and prevent further recession.

How can clinicians identify patients who would benefit from this type of surgery?
Patients with limited keratinized tissue at sites with gingival recession may benefit from a graft to enhance soft tissue thickness, increase keratinized tissue, prevent further recession, and facilitate oral hygiene. Clinicians can determine the amount of keratinized tissue by examining the mucogingival junction (ie, the demarcation between mucosa and gingiva) at the defect site. The simplest way to accomplish this is to place a probe horizontally flat against the soft tissue in the vestibule, and use it to coronally roll the mucosa. The mucogingival junction is where the mucosa stops rolling or moving. Sites with existing recession and little or no keratinized tissue may be at risk for further recession.
In terms of scheduling, what impact does this surgery have on restorative treatment?
Root coverage surgery is usually used in lieu of restorative cervical bonding of teeth with noncarious cervical lesions and shallow cervical caries. When a tooth needs root coverage and restorative treatment, restorative procedures should be performed first (if possible) to eliminate caries and stabilize the tooth. In cases involving partial or full veneers in the esthetic zone, preliminary restorative work can begin prior to, or 6 weeks following, root coverage therapy. Final margin placement and impression should not occur, however, until the soft tissue margin has completely stabilized—typically, after 6 months of healing. In cases involving high esthetic demand, it may be prudent to wait as long as 12 months prior to final restorations to allow complete remodeling of the soft tissue.
Featured image by DANIELZGOMBIC/ISTOCK/GETTY IMAGES PLUS
From Dimensions of Dental Hygiene. October 2017;15(10):28,30.

