 PHOTO COURTESY OF DENTALVIEW INC
PHOTO COURTESY OF DENTALVIEW INC
Role of the Dental Endoscope in Calculus Detection
This technology can help clinicians in their efforts to completely remove subgingival calculus.
There is no longer mystery surrounding the basic etiologies of chronic adult periodontitis and the roles played by bacterial biofilm and calculus. The bacterial infection of gingival tissues in periodontal diseases is well documented.1–5 Although a much debated topic over the past decade, the presence or retention of calculus is clearly significant in disease progression and chronicity.1,2,6,7 Thus, successful long-term treatment of chronic periodontitis depends on the complete removal of subgingival calculus—not an easy task.2,3,7 Complete subgingival calculus removal using the conventional “blind” approach is complicated by root anatomy, pocket depth, and dependence on tactile sensitivity in a subgingival environment.5,8 These limitations have been repeatedly illustrated.7,9–11 The introduction of the dental endoscope has attempted to alleviate these challenges by enabling subgingival viewing of the pocket area during instrumentation.7,12,13 The effectiveness of this technology in periodontal and dental hygiene care has been studied in the literature.7,11,13–18
COURTESY OF DENTALVIEW INC
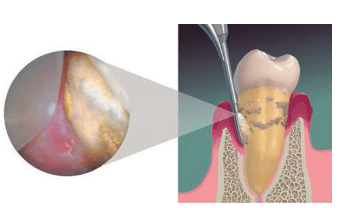
The dental endoscope is a subgingival viewing system that includes a fiber optic lens for relaying images, a water irrigation source, imaging electronics, and a monitor.11,13,14 The fiber optic lens used for capturing and transmitting images is 1 mm in diameter and covered by a single-use sterile sheath for clinical application on each patient.12–14 Images are displayed on the monitor for real-time viewing and are magnified 24 times to 48 times, with magnification depending on the proximity of the lens to the imaged tissue (Figure 1).12–14 Water flows consistently during use to aid in viewing pocket contents such as sulcular tissues, root surfaces, caries, and deposits.11 Hand-held metal handles control the position of the fiber optic tip and sheath so the endoscope can be inserted into the sulcus.11,14 These handles have multiple shank designs that facilitate access into different sites, much like #11/12 and #13/14 hand curets are designed to access specific areas.
In terms of clinical technique, there are two basic approaches to deposit removal when using the dental endoscope: two-handed perioscopy and what Pattison calls the “view, instrument, view” process.7,13 While two-handed perioscopy is theoretically more efficient, it requires more experience with the endoscope to achieve mastery. Pattison notes difficulty with this approach because of the tightly restricted spaces that remain when the endoscope and deposit-removal instruments are positioned in the subgingival site.7 Interpretation of the images also takes training and practice, as they continually change with illumination and magnification.12,17 In the “view, instrument, view” technique, the camera is removed from the pocket and the scaling instrument is inserted. This technique precludes visualization while instrumenting the tooth surface, but the ability to see the area post-instrumentation enables thorough calculus removal.19
There are two generations of the subgingival dental endoscope in the United States, with periodontal practices remaining the most frequent purchaser of the device. One hindrance to the adoption of the dental endoscope is high cost.
LITERATURE REVIEW OF CALCULUS DETECTION
The ability to detect and remove subgingival calculus has been an ongoing problem in dentistry.8–10,20 Residual calculus has typically been studied in one of two ways:
- Directly by looking at calculus on root surfaces via extraction of hopeless teeth or viewing the subgingival surface with a dental endoscope
- Indirectly by evaluating the level of inflammation of gingival tissues or the end results of scaling and root planing
Historically, practitioners have relied on tactile (exploring) methods to evaluate root surfaces before and after subgingival instrumentation.9,10,21 Such post-treatment tactile evaluations used in research have often revealed incomplete calculus removal in deep pockets, furcation areas, and at cementoenamel junctions.8–10,20 Additionally, what clinical researchers thought was a calculus-free root surface may not have been upon further examination after extraction of teeth. For example, Sherman et al10 revealed large discrepancies between tactile and visual (post-extraction using scanning electron microscopic magnification) evaluations of root surfaces. In this study, 77% of the surfaces deemed calculus free with the explorer were found to have retained subgingival calculus when examined visually under a microscope.10
Several studies have evaluated the use of the dental endoscope during and after scaling and root planing to add subgingival visual evaluations of calculus removal.17,21,22 Geisinger et al21 performed scaling and root planing on periodontally involved single-rooted teeth. One of each matched pair was visually examined with a periodontal endoscope for calculus removal and the other was tactilely examined with a hand explorer before extraction. A statistically significant decrease in residual calculus was found when the endoscope was used, especially in deep pockets.21 A similar study was conducted on multirooted teeth comparing the endoscope with tactile methods of calculus detection before extraction.22 Use of the endoscope facilitated calculus detection at interproximal sites, but not on facial/lingual surfaces, in furcations, or in deep pockets.22 In a nonextraction clinical study of periodontally involved teeth, my colleagues and l compared the endoscope with tactile evaluation of calculus immediately post-scaling and root planing and at two subsequent re-evaluation visits 6 weeks to 8 weeks apart.17 The outcomes indicated that the dental endoscope, while significantly improving calculus detection at all visits, was most beneficial when used during the re-evaluation phase of periodontal therapy.17
Patients’ gingival responses after periodontal treatment can provide indirect evidence of how the endoscope performs clinically, while illustrating the role that residual calculus plays in continuing periodontal inflammation. Several studies have examined tissue inflammation, bleeding on probing, and improvement in periodontal tissues.5,15,23–26 These studies have used the typical parameters of periodontal assessment: pocket depth, attachment level, bleeding on probing, gingival index, plaque index, and calculus index. However, additional indices have been developed for purposes of delineating subgingival findings when using an endoscope, such as endoscopic biofilm index, endoscopic calculus index, and endoscopic gingival index.5,15,23,24
Checchi et al5 hypothesized that bleeding on probing was indicative of residual subgingival calculus and used the endoscope to evaluate the relationship between these two clinical parameters.5 A strong positive correlation was found between bleeding on probing and presence of endoscopic-detected subgingival plaque and calculus deposits after scaling and root planing of periodontal sites. The authors highlighted persistent bleeding on probing as an indicator of retained subgingival deposits, while also acknowledging that differences in patient responses occur.5 Use of the endoscope also allowed researchers to determine a significant relationship between subgingival calculus covered with biofilm and inflammation of the subgingival sulcular tissue.23
Researchers have also noted significant anatomical relationships between retained subgingival biofilm/calculus and the proximate redness of subgingival sulcular tissues.23 More than 60% of the inflamed sites contained calculus with biofilm vs biofilm alone. In a companion study, the same authors used the endoscope to achieve thorough scaling and root planing of 12 periodontally involved teeth.24 After a healing period, the teeth were extracted. Biopsies of the adjacent gingival tissues determined that there were no histological signs of chronic inflammation.24
Clinical studies comparing traditional scaling and root planing to those incorporating the adjunctive use of the endoscope are few and they report varying results in pocket depth and attachment level outcomes.15,16,25,26 Stambaugh et al25 conducted a study in nonresponsive or declining periodontal sites. Approximately 800 sites were conventionally treated and maintained for 2 years, but were declining in terms of attachment loss, bleeding, and inflammation. Retreatment of these sites with the endoscope resulted in an average pocket depth reduction from 4.37 mm to 3.12 mm. A subgroup with attachment loss >2 mm within the 2 previous years was further analyzed. For this group, reduction in mean pocket depth went from 5.36 mm to 3.03 mm when using the endoscope, with an average attachment gain of 2.06 mm. Statistical significance was not reported.25 Kwan26 treated 270 patients with moderate to advanced periodontitis. All pocket depths >4 mm were treated with an endoscope in one visit followed by a course of systemic antibiotics. Patients underwent reevaluation and retreatment at 3-month intervals for 1 year, at which time comparison pocket depth measurements were made. Results revealed pocket depth reduction for all tooth types with the highest reductions occurring in deep pocket depths of posterior teeth. For example, in molars, 69% of pocket depths starting at 5 mm to 6 mm were reduced to <4 mm.26 Blue et al15 conducted an endoscopic clinical study of 26 patients with moderate periodontitis. The purpose was to compare the clinical outcomes of scaling and root planing in endoscope vs nonendoscope sites post-treatment and at subsequent re-evaluation visits. Using the endoscope provided significant improvement for bleeding on probing and gingival index, but not for reductions in pocket depth and attachment levels.15 Not all studies have shown better results using an endoscope. For example, a study of six patients with chronic periodontitis found no clinical improvements attributable to the use of the dental endoscope. However, minimal training was provided to the practitioner involved in this study.16
CALCULUS DETECTION
The previous extraction and clinical studies using the dental endoscope highlight the value of subgingival vision during scaling and root planing (Table 1 provides a summary). Overall, the literature has reported favorable results (compared with blind scaling and root planing) when a dental endoscope is used.7,13–15,17,18,21–27 Not only is subgingival calculus more thoroughly removed when using an endoscope, but a general improvement in periodontal tissues can be expected.7,13–15,17 Unfortunately, improved outcomes seem less likely when treating the furcal aspects of multirooted teeth.27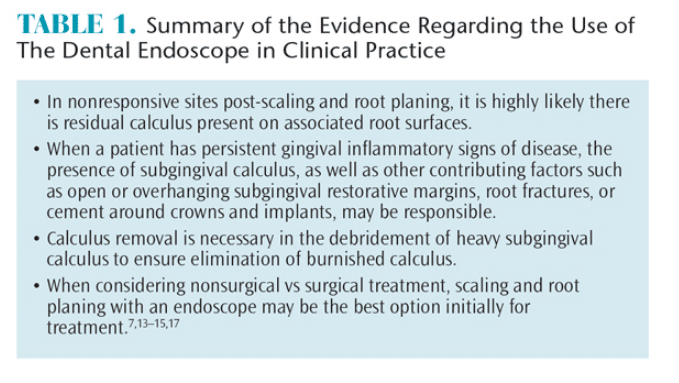
In studies where endoscope use had failed to show improvements compared with control therapies, authors agreed that limitations such as clinician training, experience, and calibration may have contributed to these outcomes.15–17 This technology requires hours of practice to achieve competency. Stambaugh14 estimated that rudimentary skill development for imaging and instrumentation would take approximately 2 months of using an endoscope for 2 hours to 3 hours per week.
Overall, there is convincing evidence for using an endoscope as an additional means of ensuring success in periodontal treatment and creating a healthy subgingival environment. Using available technology to provide for more predictable treatment outcomes is a positive step toward advancing the profession, as well as patient care.
References
- Cobb CM. Microbes, inflammation, scaling and root planing, and the periodontal condition. J Dent Hyg. 2015;82(Suppl 3):4–9.
- Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidence- based perspective of scaling and root planing. J Clin Periodontol. 2002;29(Suppl 2):6–16.
- Sherman PR, Hutchens LH, Jewson LG. The effectiveness of subgingival scaling and root planing, II. Clinical responses related to residual calculus. J Periodontol. 1990;61:9–15.
- Greenstein G. Nonsurgical periodontal therapy in 2000: a literature review. J Am Dent Assoc. 2000;131:1580–1592.
- Checchi L, Montevecchi M, Checchi V, Zappulla F. The relationship between bleeding on probing and subgingival deposits. An endoscopical evaluation: Open Dent J. 2009;3:154–160.
- Keptic TJ, O’Leary TJ, Kafrawy AH. Total calculus removal: an attainable objective? J Periodontol. 1990;61:16–20.
- Pattison AM, Pattison GL. Periodontal instrumentation transformed. Dimensions of Dental Hygiene. 2003;1(2):18–22.
- Brayer WK, Mellonig JT, Dunlap RM, Marinak KW, Carson RE. Scaling and root planing effectiveness: the effect of root surface access and operator experience. J Periodontol. 1989;60:67–72.
- Rabbani GM, Ash MM Jr., Caffesse RG. The effectiveness of subgingival scaling and root planning in calculus removal. J Periodontol. 1981;52:119–123.
- Sherman PR, Hutchens LH Jr, Jewson LG, Moriarty JM, Greco GW, McFall WT. The effectiveness of subgingival scaling and root planning. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Carroll J. The evolution of care: why ‘perioscopy’ could change the way you view your patients. Available at: periopeak.com/_media/pdf/Judy-Carroll-publications/MH1106_46-48_C-Perios.pdf. Accessed January 23, 2015.
- Stambaugh RV, Myers G, Ebling W, Beckman B, Stambaugh K. Endoscopic visualization of the submarginal gingiva dental sulcus and tooth root surfaces. J Periodontol. 2002; 73:374-382.
- Kwan J. Enhanced periodontal debridement with the use of micro ultrasonic periodontal endoscopy. J Calif Dent Assoc. 2005;33:241–248.
- Stambaugh RV. Perioscopy: the new paradigm. Dimensions of Dental Hygiene. 2003;1(2):12–16.
- Blue CM, Lenton P, Lunos SA, Poppe K, Osborn JB. A pilot study comparing the outcome of scaling/root planing with and without Perioscope™ technology. J Dent Hyg. 2013;87:152–156.
- Avradopoulos A, Wilder RS, Chichester S, Offenbacher S. Clinical and inflammatory evaluation of Perioscopy™ on patients with chronic periodontitis. J Dent Hyg. 2004;78:30–38.
- Osborn JB, Lenton PA, Lunos SA, Blue CM. Endoscopic vs tactile evaluation of subgingival calculus. J Dent Hyg. 2014;88:229–236.
- Poppe K, Blue C. Subjective pain perception during calculus detection with use of a periodontal endoscope. J Dent Hyg. 2014;88:114–123.
- Kiehl N. Five myths about periodontal instrumentation. Dimensions of Dental Hygiene. 2011;9(11):68–70.
- Stambaugh RV, Dragoo M, Smith DM, Carasali L. The limits of subgingival scaling. Int J Periodontics Restorative Dent. 1981;1:30-41.
- Geisinger ML, Mealey BL, Schoolfield J, Mellonig JT. The effectiveness of subgingival scaling and root planning: An evaluation of therapy with and without the use of the periodontal endoscope. J Periodontol. 2007;78:22–28.
- Michaud RM, Schoolfield J, Mellonig JT, Mealey BL. The efficacy of subgingival calculus removal with endoscopy-aided scaling and root planing: a study on multirooted teeth. J Periodontol. 2007;78:2238–2245.
- Wilson TG, Harrel SK, Nunn ME, Francis, B, Webb, K. The relationship between the presence of tooth-borne subgingival deposits and inflammation found with a dental endoscope. J Periodontol. 2008;79:2029–2035.
- Wilson TG, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: human biopsies—a pilot study. J Periodontol. 2008;79:2036–2041.
- Stambaugh RV, Myers, Watanabe J, Lass C, Stambaugh KA. Endoscopic instrumentation of the subgingival root surface in periodontal therapy. J Dent Res. 2000;79(Special issue):489.
- Kwan JY, Workman PD. Micro ultrasonic endoscopic periodontal debridement: retrospective analysis of treatment with at least 1 year follow-up. Available at: perioscopyinc.com/documents/aap_poster_boston_2009.pdf. Accessed January 23, 2016.
- Stambaugh RV. A clinician’s 3-year experience with perioscopy. Compend Contin Educ Dent. 2003;23:1061–1070.
From Dimensions of Dental Hygiene. February 2016;14(02):40,42–44.

