Risk Assessment for Autoimmune Diseases
Dental hygienists can serve as advocates for their patients with autoimmune diseases—from detecting immune system dysfunction to providing safe and effective treatment.
This course was published in the December 2012 issue and expires December 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the pathophysiology of immune system dysfunction.
- Recognize systemic and oral manifestations of autoimmune diseases.
- Utilize a risk assessment tool to assess for autoimmune diseases.
- Use the dental hygiene process of care to provide safe and effective oral treatment for patients with autoimmune diseases.
In the United States, over 50 million people, most of whom are women, have some type of autoimmune disease.1 There are more than 80 different kinds of autoimmune disorders.2 Autoimmunity is the second leading cause of chronic illness.1 Diagnosis of autoimmune diseases is often difficult and may take years to attain. The diseases themselves, as well as their medication management, can adversely affect the oral cavity and significantly impact quality of life.
IMMUNE SYSTEM DYSFUNCTION
The human immune system exhibits self-tolerance, meaning that it recognizes the difference between “self” and “foreign” antigens. When innate mechanisms that normally prevent the immune system from attacking self-antigens fail, activated T cells and antibodies begin to attack the body’s own tissues, a process known as autoimmunity. Conditions associated with autoimmunity are collectively called autoimmune diseases.3–5
Antibodies that cause autoimmunity bind to self-antigens and form complexes that are deposited in specific tissues and organs, or they travel throughout the bloodstream and become deposited in blood vessels. Deposition of these bound antibodies accounts for the tissue destruction, inflammation, and systemic complications observed with autoimmune diseases. Destruction of receptors that respond to stimulation from neurotransmitters and hormones may also occur, resulting in muscular and endocrine problems, such as multiple sclerosis and thyroid disease.3
The development of autoimmunity typically depends on two factors. First, genes are inherited that increase susceptibility and contribute to the failure of self-tolerance. Second, one or more environmental triggers, such as infection, fever, or severe trauma, initiate activation of autoantibodies.
AUTOIMMUNE DISEASE CHARACTERISTICS
Patients often present with more than one autoimmune disease. Because autoantibodies can travel throughout the body, patients usually experience multisystem organ involvement that may not be easily explained or diagnosed. Signs and symptoms of this involvement are nondescript, and often present as fatigue, joint pain, muscle aches, sleep disorders, and anemia. Patients may experience psychiatric difficulties because they often see multiple providers without receiving definitive diagnoses or treatment recommendations for a long time.
The result is that patients live with diminished quality of life and ongoing health challenges, including compromised oral health. Some of the most well-known autoimmune diseases include adrenal insufficiency, chronic fatigue syndrome, cicatricial pemphigoid, fibromyalgia, hyper- and hypothyroidism, multiple sclerosis, myasthenia gravis, pemphigus vulgaris, rheumatoid arthritis, scleroderma, Sjögren’s syndrome, and systemic lupus erythematosus. Addison’s disease and adrenal insufficiency occur when infections, cancer, or the chronic use of steroid hormones destroy the adrenal glands. Chronic fatigue syndrome is characterized by profound fatigue that is not improved with bed rest and is worsened by physical or mental activity. It is diagnosed with a blood test that reveals an immune response consistent with viral infection. Cicatricial pemphigoid is a benign, chronic blistering disease that affects oral and genital mucosa, as well as conjunctiva of the eye and skin. The resultant lesions scar when healing. A widespread musculoskeletal disorder characterized by pain in the muscles, ligaments, and joints, as well as fatigue, fibromyalgia is often accompanied by other autoimmune conditions, including chronic fatigue syndrome, rheumatoid arthritis, systemic lupus erythematosus, and hypothyroidism.
Also known as thyrotoxicosis, hyperthyroidism, occurs when too much thyroxine and triiodothyronine are present in the bloodstream, affecting the body’s metabolic rate. Hypothyroidism causes progressive gland deterioration, leading to fibrosis and reduced secretion of thyroid hormone. Multiple sclerosis is the most common autoimmune disease that affects the nervous system. It is caused by demyelination of nerves in the central nervous system due to chronic inflammation. A chronic autoimmune disease, myasthenia gravis affects the neuromuscular system, decreasing acetylcholine receptors in muscle fibers, resulting in progressive fatigability and abnormalities in skeletal muscle. Pemphigus vulgaris is a progressive, severe disease affecting the skin and mucous membranes characterized by bullae that rupture and form painful ulcers. Rheumatoid arthritis is a chronic inflammatory condition characterized by pain, swelling, stiffness, and loss of function affecting the joints. A chronic disease of the connective tissue, scleroderma affects all organ systems and includes both localized and systemic types. Sjögren’s syndrome, which includes both primary and secondary forms, causes dry eyes, xerostomia, and connective tissue problems. Systemic lupus erythematosus is characterized by periods of remissions and exacerbations, and affects the skin, joints, kidneys, brain, and other organs.
RISK ASSESSMENT MODEL
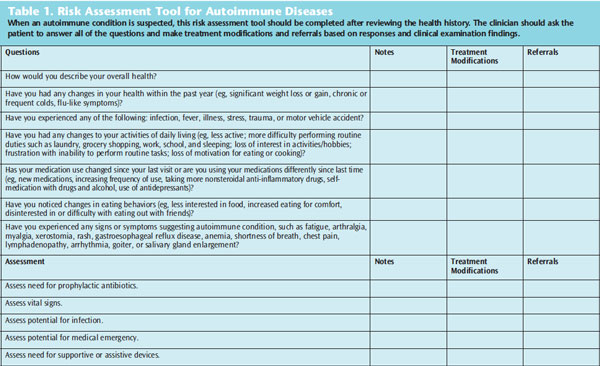
Dental hygienists have the opportunity to provide refined assessment for autoimmune diseases by taking a careful health history and using probing questions regarding manifestations that may suggest an autoimmune component. Table 1 presents a risk assessment tool that can be used to assist with decision making throughout the dental hygiene process of care.
APPLICATION TO THE DENTAL HYGIENE PROCESS OF CARE
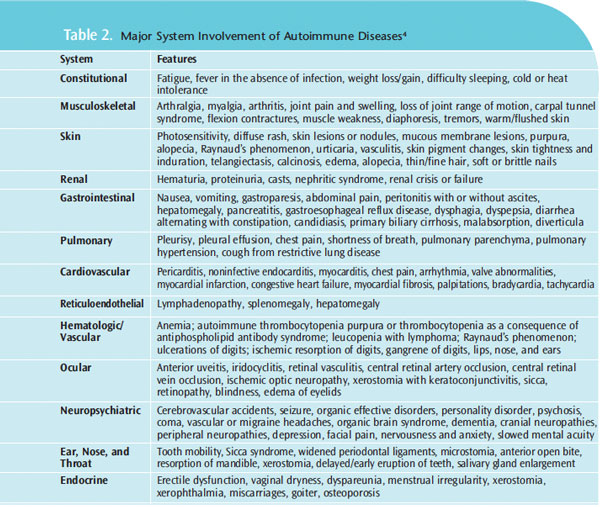
When planning care, the major system involvement of autoimmune diseases should be considered (Table 2).4 Given the nature and extent of systemic and oral involvement, using the dental hygiene process of care will ensure adequate planning for the delivery of safe and comprehensive oral treatment.
During the assessment phase, performing a thorough medical, oral, and pharmacologic history review is critical to identify conditions that warrant referral for medical evaluation. Using a risk assessment tool will assist dental hygienists to determine whether modifications are necessary to provide treatment (Table 1). The clinician must determine if the need for medical care supersedes oral care, whether it is safe to provide treatment, and what the patient can tolerate in terms of appointment scheduling and procedures. In some cases, oral care may be deferred until additional medical evaluation and/or treatment is provided.
The signs and symptoms observed and those reported by the patient are key to an effective assessment. Both objective and subjective assessment findings are used to identify key diagnostic findings. They are then summarized to support proposed treatment. Care planning takes into consideration the physical demands on the patient. Shorter appointments may be necessary to accommodate patients with joint pain, stiffness, swelling, shortness of breath, and other manifestations that affect their ability to sit for long periods. Assistive devices needed to provide comfort for the patient should be discussed in advance and outlined as part of the treatment plan. In some cases, the clinician may need to consult with the patient’s physician so that oral care can occur in concert with medical treatment in a safe manner. Dental hygienists have an opportunity to serve as an advocate for patients who require both physical and psychological support when recognizing that needs are not being met by current medical care.
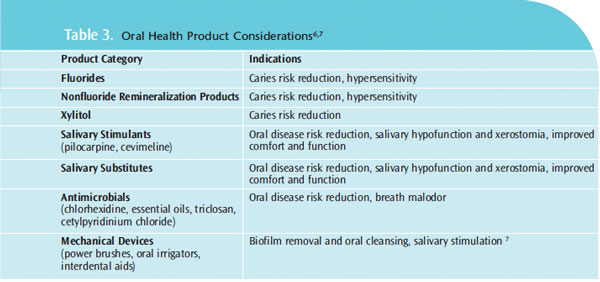
Implementation includes both the administration of dental hygiene interventions to minimize oral infections and restore health, and patient education. Patients need to understand the relationship between their autoimmune disease, medical management, and oral considerations. Some patients may require further care with an oral specialist if mucosal lesions are not responding to initial treatment protocols. Clinicians should consider recommending products that will provide the best possible results for biofilm, caries, and xerostomia management. Table 3 provides examples of product considerations that may be useful.6,7
The evaluation component of the dental hygiene process of care includes three main elements: time interval for regular dental hygiene appointments, follow-up to asses outcomes of treatment, and ongoing evaluation of the patient’s ability to adequately maintain oral health and hygiene. Patients with autoimmune disease may not have the same host defense ability to manage the challenges of oral diseases and risk for recurring infections. More frequent continuing care appointments are warranted. Two month to 3 month intervals may be important to assess patient oral disease states, provide further treatment, and reinforce self-care regimens. More frequent intervals of care will allow dental hygienists to monitor general health status and maintain communication with other health care providers. Further, once dental hygiene services have been rendered during initial implementation, the patient should return for a 6 week re-evaluation visit to assess treatment outcomes and the need for additional intervention.
The final step in the dental hygiene process of care is to document all findings at each appointment. Practitioners should report whether goals are met and the factors influencing outcomes. Further treatment, referrals, and patient response to dental hygiene care should be recorded.
CONCLUSION
Patients affected by autoimmune diseases are medically complex and present many challenges. Use of the risk assessment model can assist clinicians with decision making throughout the dental hygiene process of care. Careful analysis of systemic and oral health considerations helps to ensure that comprehensive dental hygiene care can be delivered safely to improve the oral health of this population.
ACKNOWLEDGEMENT
Laguna design/science photo library
REFERENCES
- American Autoimmune Related Diseases Association, Inc. AARDA Facts. Available at:www.aarda.org/aarda_facts.php. Accessed November 2, 2012.
- United States National Library of Medicine National Institutes of Health. Autoimmune disorders.Available at: www.nlm.nih.gov/medlineplus/ency/article/000816.htm. Accessed November 2, 2012.
- Abbas AK, Lichtman AH. Basic Immunology: Functions and Disorders of the Immune System. 2nded. Philadelphia: Elsevier; 2004.
- Gurenlian JR, Spolarich AE. Immune system dysfunction. In: Daniel SJ, Harfst SA, Wilder RS, eds.Mosby’s Dental Hygiene: Concepts, Cases, and Competencies. 2nd ed. St. Louis: Mosby Elsevier;2008:855–882.
- Walsh MM. Persons with autoimmune diseases. In: Darby ML, Walsh MM. Dental Hygiene Theoryand Practice.3rd ed. St. Louis: Saunders Elsevier; 2010:919–932.
- Spolarich AE. Xerostomia and oral disease. Dimensions of Dental Hygiene. 2011;9(11;Suppl):43–54.
- Papas A, Singh M, Harrington D, et al. Stimulation of salivary flow with a powered toothbrush in axerostomic population. Spec Care Dentist. 2006;26:241–246.
From Dimensions of Dental Hygiene. December 2012; 10(11): 30–33.



