Managing the Developing Occlusion
Dental hygienists who are well versed in normal and atypical development of the mixed dentition can significantly contribute to positive patient outcomes.
This course was published in the December 2012 issue and expires December 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the normal development of the primary and mixed dentitions.
- Identify potential problems that may compromise normal developing dentitions.
- Discuss the appliances commonly used to correct malpositioning in the primary and mixed dentitions.
While comprehensive orthodontics may be part of effectively addressing malocclusion, preventive and assessment protocols—typically provided by dental hygienists—are just as important. Dental hygienists reinforce the dentist’s treatment plan by helping patients and parents understand and accept proper treatment protocols. To accomplish this, dental hygienists need to be well versed in normal and atypical growth and development, as well as the importance of space preservation, guidance interventions, and corrective appliances in the developing occlusion.
PRIMARY DENTITION AND OCCLUSION
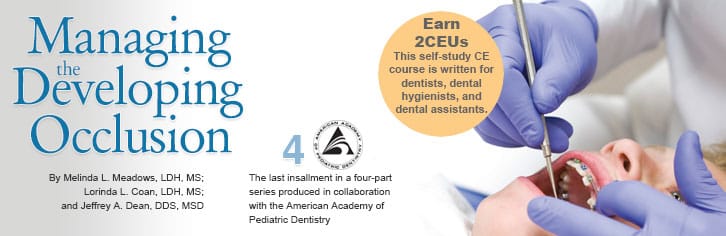
In most children, primary teeth erupt between 8 months and 30 months, following the same sequence in each arch (Figure 1). Eruption that differs from this pattern may warrant further evaluation.1 As the alveolar process grows, spaces develop between the primary incisors. This developmental spacing can add up to 6 mm of space per arch. Although the space looks different than the esthetic ideal, up to 4 mm of space gain is considered desirable.2 Dental hygienists can assure parents that this extra space is normal and helps to avoid transitional crowding.
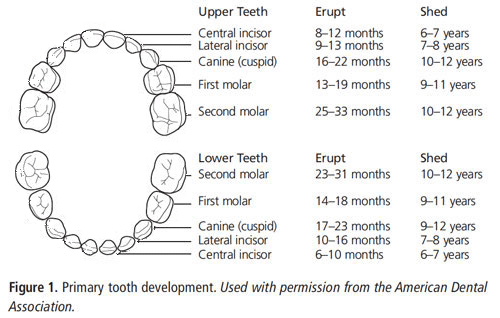
Malocclusion is any deviation from the normal relationship of the maxillary arch and/or teeth to the mandibular arch and/or teeth. In the primary dentition, the molar relationship is evaluated by observing the association between the terminal planes (the most distal line angle) of the second primary molars. The terminal plane of the maxillary second primary molar serves as the fixed point, and the relationship of the mandibular terminal plane has a mesial step, distal step, or flush (straight) relationship to the maxillary terminal plane (Figure 2). About 75% of children present with a flush terminal plane, with 15% exhibiting mesial step and 10% demonstrating distal step relationships.1,3 The majority of flush and mesial steps will develop into Class I permanent molar relationships. Some mesial steps can become Class III dental/skeletal relationships and distal steps often result in Class II permanent molar relationships.2,4
POTENTIAL CHALLENGES
The primary dentition maintains arch integrity and space for the permanent teeth. Problems may include: early tooth loss, ectopic eruption of teeth, nonnutritive sucking, and mouth breathing.2 Early loss of primary or permanent teeth can negatively impact the arch length, positioning of adjacent and opposing teeth, food impaction, and even speech. Caries and trauma are the most common reasons for early tooth loss, but ectopic eruption of teeth can also result in the loss of a tooth prematurely. In the primary dentition, early loss of teeth can cause supra-eruption of the opposing tooth and drifting of proximal teeth. The early loss of the second primary molar causes the most damage.2 The decision to maintain space using a fixed appliance should consider timing of the tooth loss relative to the eruption of other teeth, overall arch space, the specific tooth lost, caries risk, and patient compliance.
Nonnutritive sucking of both the fingers/thumb and pacifiers can result in anterior open bite, flared maxillary incisors, lingually-inclined mandibular incisors, and a narrow or v-shaped palate leading to a posterior crossbite. Damage to the dentition is often found among children who suck their thumb for 6 hours per day or more.4 As children mature, most will eliminate this habit. Encouragement and behavior management often end nonnutritive sucking, but the use of an appliance can be considered once children reach age 4. In situations where the child is a mouth breather or the airway is compromised, skeletal open bite may result from alterations to the craniofacial growth pattern. Such patients may need to be referred. Management of the developing occlusion may include palatal expansion.1
THE MIXED DENTITION
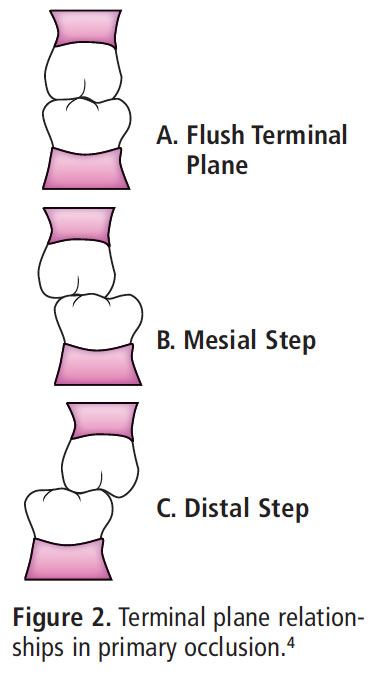
Between the ages of 6 and 12, dental hygienists help determine whether a patient’s developing occlusion is progressing appropriately (Figure 3). The pattern of the face does not change significantly during growth. Severe space deficiency in primary teeth is predictive of future space deficiencies in the mixed and permanent dentitions.2 Dental hygienists should assist patients and their families in understanding the existing situation, likely outcomes, and the possible interventions.1,2
Anterior crowding is common during incisor eruption, frequently from a tooth size/arch discrepancy that often benefits from intervention. Leeway space is the difference in total space occupied by the deciduous canine and first and second molars, and the permanent canine and first and second premolars that will replace them. Early orthodontic interventions often try to maintain this space so that it may be used to manage tooth/arch discrepancies. During this time, the erupting maxillary lateral and canine can exert pressure on the roots of the central incisors, causing distal tipping, which can result in an esthetically undesirable appearance.4 Parents and patients should be assured that this is a normal phase.
Ectopic eruption of the maxillary first permanent molar occurs in 2% to 3% of patients (Figure 4). Dental hygienists should evaluate bitewing or panoramic radiographs for evidence of ectopic eruption of the first permanent molar for each patient from age 5 until the first molar has erupted past the cervical neck of the second primary molar. Many of these self-correct, but a Humphrey or Halterman appliance may be indicated to distalize the ectopically-erupting first molar.2,4

When a single posterior tooth is lost prematurely, the maintenance of the arch space may be accomplished by using a unilateral space appliance, ie, band and loop2 (Figure 5). The appliance is cemented to the tooth posterior to the space, with the wire resting against the distal surface of the tooth mesial to the space, preventing mesial drift of the posterior tooth. If the second primary molar is lost prior to eruption of the first permanent molar, a distal shoe is placed to guide the first permanent molar into place.2 In mandibular bilateral tooth loss, a lower lingual holding arch is constructed using a similar approach, with bands placed on both permanent molars and a lingual wire that contacts the incisors (Figure 6A). A Nance appliance2 is used on the maxilla (Figure 6B). Since the presence of a bar against the lingual of the maxillary anterior teeth would interfere with occlusion, the rest is an acrylic button on the hard palate.2 Dental hygienists should check each appliance carefully for movement and remember that failed cement seals can allow caries development beneath the band.5
In the mixed dentition, maxillary arch expansion may be indicated to address severe crowding or crossbites. A fixed palatal expander (Figure 7) or a Haas appliance is used to gain space by expanding the midline palatal suture area. This results in an average increase of 6 mm in arch width. A Hawley appliance with a finger spring can be used to correct an anterior crossbite2,4 (Figure 8).


SYMMETRY

In the developing face, children should be evaluated for age-appropriate dental, skeletal, and functional symmetry. The analysis of the face includes: extraoral comparison of the right and left halves of the face for symmetry and evaluation of the balance between the upper, middle, and lower thirds of the face; intraoral assessment of the dentition and the oral structures; and an assessment of the panoramic and cephalometric radiographs. Any deviation from normal in these areas may warrant referral to a specialist.2
EARLY INTERVENTION
While early orthodontic treatment may provide benefit to some patients, the need for extractions or orthognathic surgery is not necessarily reduced. Nonetheless, certain patients may experience improvement in crowding, leveling, and the alignment of anterior teeth with early interventions.2 Concern about esthetics often prompts parents of children between the ages of 8 and 10 to inquire about orthodontics. Dental hygienists should interview the parent and patient to clarify concerns and provide education and referral as indicated.

Class II problems can be treated with both removable and fixed appliances. Removable appliances include the use of a headgear or an orthopedic corrector like a Bionator.2 Both restrain growth of the maxilla so that mandibular growth catches up with the maxilla, while the Bionator also helps stimulate growth of the mandible. Fixed appliances are another option, such as the Herbst appliance (Figure 9).4 Class III problems can also be treated with removable or fixed appliances. Removable appliances include a reverse headgear that protracts the maxilla forward with little effect on the mandible. Elastics are often used, as well. They attach to temporary anchorage devices fixed to the posterior of the maxilla and the anterior of the mandible, so that the maxilla is moved forward and the mandible is restrained backward.4
ORAL HYGIENE SELF-CARE
Effective oral hygiene is critical for patients undergoing orthodontic treatment. Most orthodontic treatments require patients to commit to 2 years to 3 years of active therapy and poor oral hygiene is associated with longer treatment times.6 Fixed appliances can also change the microbiological oral flora, which may affect gingival and periodontal health7 and increase caries risk.8 Decalcification can occur around orthodontic brackets in as little as 4 weeks.9 Appliances may prevent adequate plaque removal.10 Without an aggressive prevention program, as many as 50% of patients with appliances will develop white spot lesions.11
In 2008, Krishnan et al introduced the Visual Analogue Scale for Hygiene Assessment.12 It can be used by practitioners, patients, and/or parents to objectively assess the effectiveness of self-care during orthodontic treatment. The scale provides pictures of different levels of oral health status—from poor to excellent—from which patients choose the one that most closely resembles their own oral health status.

Mixed dentition patients are approaching adolescence, and effective rapport-building and communication are important. Adolescents may feel they are not being heard.13 They may have the perception that adults are too rushed to listen to their point of view or they are turned off by the offering of unsolicited advice. Explaining to adolescents the rationale for treatment, ie, “We ask all of our adult patients to floss because we know it works. This is why I’m asking you to do this now,” helps build a partnership between patient and provider. Questions that are open-ended and ask patients to develop their own solutions for identified problems can help compliance. For example, asking “What do you think is the best way to remove the plaque here?d may be more effective than simply telling them how to brush.
SUMMARY
Managing the developing occlusion involves understanding normal eruption sequence and timing. Dental hygienists must also be aware of common signs of atypical development, occlusal patterns, tooth loss, or potentially harmful developmental oral habits. Early intervention with appliances that maintain space, correct malocclusions, or guide the eruption and positioning of teeth can help reduce the need for additional orthodontic interventions. Involving patients and parents in the development of good oral hygiene practice can lead to improved patient outcomes.
ACKNOWLEDGEMENT
Figures 4 through 9 courtesy of kyla jones, chris locker, connie riech, and timothy centers
REFERENCES
- Nowak AJ, Casamassimo PS, eds. The Handbook ofPediatric Dentistry. 4th ed. Chicago: American Academy ofPediatric Dentistry; 2011;124–127.
- Dean JA, Avery DR, McDonald RE. McDonald and Avery’sDentistry for the Child and Adolescent. 9th ed. MarylandHeights, Mo: Mosby Elsevier; 2011.
- Babbush CA, ed. Mosby’s Dental Dictionary. 2nd ed. St.Louis: Mosby Elsevier; 2008.
- Proffit WR, Fields HW, Sarver DM. ContemporaryOrthodontics. 5th ed. St. Louis: Mosby Elsevier, 2012.
- Simmons LAB. Persons with orthodontic appliances. In:Darby ML, Walsh MM. Dental Hygiene Theory and Practice.3rd ed. St. Louis: Saunders Elsevier; 2010:1111–1136.
- Skidmore KJ, Brook KJ, Thomson WM, Harding WJ. Factorsinfluencing treatment time in orthodontic patients. Am JOrthod Dentofacial Orthop. 2006;129:230–238
- Petti S, Barbato E, Simonetti D’Arca A. Effect of orthodontictherapy with fixed and removable appliances on oralmicrobiota: a six-month longitudinal study. New Microbiol.1997;20:55–62.
- Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP.The effects of orthodontic therapy on periodontal health: asystematic review of controlled evidence. J Am Dent Assoc.2008;139:413–422.
- O’Reilly MM, Featherstone JD. Demineralization andremineralization around orthodontic appliances: an in vivostudy. Am J Orthod Dentofacial Orthop. 1982;92:33–40.
- Brightman, LJ, Terezhalmy GT, Greenwell H, Jacobs M,Enlow DH. The effects of a 0.12% chlorhexidine gluconatemouthrinse on orthodontic patients aged 11 through 17 withestablished gingivitis. Am J Orthod Dentofacial Orthop. 1991;100:324–329.
- Derks A, Kuijpers-Jagtman AM, Frencken JE, Van’t HofMA, Katsaros C. Caries preventive measures used inorthodontic practices: an evidence-based decision? Am JOrthod Dentofacial Orthop. 2007;132:165–170.
- Krishnan V, Daniel ST, Lazar D, Asok A. Characterizationof posed smile by using visual analog scale, smile arc, buccalcorridor measures, and modified smile index. Am J OrthodDentofacial Orthop. 2008;132:515–523.
- Oliver HE. Communication and behavioral changetheories. In: Darby ML, Walsh MM. Dental Hygiene Theoryand Practice. 3rd ed. St. Louis: Saunders Elsevier;2010:48–49.
From Dimensions of Dental Hygiene. December 2012; 10(11): 26–29.



