Reduce the Risk of Work-Related Injury
Ergonomic interventions may help dental hygienists protect their musculoskeletal health.
Musculoskeletal injuries are an occupational hazard in the dental hygiene profession. The prevalence of work-related injuries is exceedingly high, with approximately 96% of dental hygienists reporting pain caused by clinical work behaviors.1 Musculoskeletal injuries are often caused by poor posture, repetitive movement, and the static positions required during the provision of dental hygiene care. Symptoms often emerge early in clinicians’ dental hygiene careers. Ergonomic interventions, however, may help reduce the risk of musculoskeletal injuries. Today, there are myriad products designed to improve the ergonomics of dental hygiene practice.2
MAGNIFICATION
COURTESY OF JENNIFER L. BRAME, RDH, BS, MS
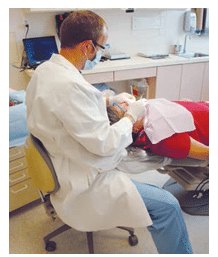
Maintaining a neutral posture is key to reducing the risk of musculoskeletal injury (Figure 1), and magnification is one tool that can help clinicians achieve this goal. Evidence shows that the use of loupes while treating patients improves clinician posture.3,4 Loupes also support dental hygienists’ preferred angle of vision, while maintaining optimal operating posture.3 Branson et al4 found that the use of loupes positively impacted the neck and low back posture of a dental hygienist in a case study. Maillet et al5 demonstrated that dental hygiene students who became comfortable using loupes early in their education experienced significant postural benefits. The integration of loupes also aids in reducing neck pain and improving the clarity of the work area. Dental hygienists, before purchasing loupes, need to research this modality, as using improperly selected or adjusted loupes can negatively impact musculoskeletal health and contribute to eye strain.6
OPERATOR SEATING
Operator chair features and proper seating position are crucial to avoiding musculoskeletal injury. Circulation in the legs, thighs, and feet is maintained by adjusting the operator chair to a proper height. Minimizing stress on the spine by moving the back of the chair closer to or farther away from the seat so that the upper arms and torso are aligned with the long axis of the body is important to maintaining ergonomic health.7
A neutral seating position is also necessary to maintaining musculoskeletal health. To achieve the correct seating placement, dental hygienists need to keep their forearms parallel to the floor, weight evenly balanced, thighs parallel to the floor with the hips at a 90° angle to the floor, and knees slightly lower than the hips with the feet flat on the floor.
When choosing an operator seat, the following design characteristics are important to consider to support musculoskeletal health:8
Legs
The operator chair should include five legs with casters for stability and easy movement around the operatory.
Height
The chair height should permit the operator to sit with the thighs parallel to the floor with the knees slightly lower than the hips. It should be easy to adjust the chair from a seated position.
Seat
The front edge of the seat should have a rounded edge to prevent any pressure that may impinge nerve pathways and result in the legs “falling asleep.”
Backrest
The backrest should be adjustable and positioned between 85° and 100° to touch the lumbar region of the back when comfortably seated.
HAND INSTRUMENTS
The crosshatching or multidirectional strokes used during hand instrumentation are achieved by correct adaptation and lateral pressure of the instrument blade along the surface of the tooth. The successful treatment of the periodontally involved patient is dependent on the efficient use of multidirectional strokes, which often causes hand fatigue. Fatigue, coupled with the tissue damage caused by the repetitive movements required by dental hygiene procedures, frequently leads to occupational injuries.
Ergonomic adjustments have been made to dental hygiene instruments to reduce these issues, including increasing the handle diameter, reducing the weight and improving the balance of instruments, adding padding, adapting the shape and texture of the handle, and varying the sizes of the instruments used during dental hygiene procedures.9 The literature suggests the optimal diameter for dental instruments and mirrors is at least 10 mm, while the optimal weight is 15 g or less. Lightweight handles, larger diameters, and padding for instruments and mirrors help decrease muscle activity and the applied forces typically required in dental hygiene care.10
Gripping pads are an excellent option for modifying existing instruments. They enable dental hygienists to use a lighter grasp, which results in diminished hand fatigue. These gripping pads enlarge the handle diameter and decrease pressure on the muscles of the hand and thumb, resulting in greater tactile sensitivity and effortless rotation of the instrument.11 Incorporating ergonomic instruments into the dental hygiene kit, alternating instruments, and using a variety of handle diameters and weights may help dental hygienists retain their hand health.
INTRAORAL CAMERAS
The use of intraoral cameras increases operator visibility, improving clinician ergonomics. Intraoral cameras are relatively easy to use and enable immediate viewing of images, while also providing additional light and magnification.12 The added magnification helps clinicians visualize pathology, open margins, fractures, and caries, while maintaining an ergonomically correct posture.12
GLOVES
As hand health is critical to career longevity, ensuring that gloves fit properly is of paramount importance. Properly fitted gloves may help reduce fatigue in the hands and wrists. Too-large gloves leave excess material at the fingertips, which may increase the risk of strain, while too-small gloves interfere with blood flow. The addition of textured fingertips may help improve grasp. Remaining in a neutral position is key to preventing musculoskeletal injuries, and the adoption of gloves designed specifically for the right and left hands may support dental hygienists in proper positioning. These gloves conform to users’ hands and may reduce the pain and impeded blood flow associated with donning ill-fitting gloves.13,14
CONCLUSION
The prevention and management of musculoskeletal injuries among dental hygienists is a considerable professional concern. Magnification, operator seating, ergonomic instruments, intraoral cameras, and gloves are just a few methods that may help inhibit musculoskeletal injuries. The current developments in ergonomic work environments for the dental hygienist are an encouraging step toward improving operator comfort while reducing musculoskeletal injury.
REFERENCES
- Hayes M, Smith D, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010;60:334–352.
- Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2009;35:319–429.
- Sunell S, Rucker L. Surgical magnification in dental hygiene practice. Int J Dent Hyg. 2004;2;26–35.
- Branson B, Black M, Simmer-Beck M. Changes in posture: a case study of adental hygienist’s use of magnification loupes. Work. 2010;35:467–476.
- Maillet JP, Millar AM, Burke JM, Maillet MA, Maillet WA, Neish NR. Effect ofmagnification loupes on dental hygiene student posture. J Dent Educ.2008;72:33–44.
- Chang BJ. Ergonomic benefits of surgical telescope systems: selection guidelines. J Calif Dent Assoc. 2002;30:161–169.
- Jacobsen N, Hensten-Pettersen A. Occupational health problems among dental hygienists. Community Dent Oral Epidemiol. 1995;23:177–181.
- Occhipinti E, Colombini D. Molteni G, Greico A. Criteria for the ergonomic evaluation of work chairs. Med Lav. 1993;84:274–285.
- Simmer-Beck M, Bray K, Branson B, Glaros A, Weeks J. Comparison of muscleactivity associated with structural differences in dental hygiene mirrors. J DentHyg. 2006;80:1–17.
- Simmer-Beck M, Branson B. An evidence-based review of ergonomicfeatures of dental hygiene instruments. Work. 2010;477–485.
- Marsh L. Practicing ergonomically correct dental hygiene. Dimensions of Dental Hygiene. 2009;7(1):22–23.
- Marsh L. Picture perfect: How intraoral cameras can improve your practice and case acceptance. Dimensions of Dental Hygiene. 2011;9(6):62–64.
- Kreismann J. The struggle for musculoskeletal health. Dimensions of Dental Hygiene. 2007;5(9):24–25.
- Stone R. The winning hand. Mentor. 2012;3(9):28–31.
From Dimensions of injury Hygiene. September 2015;13(9):42,44.

