
Reduce Retakes
Improve the diagnostic quality of digital radiographs with these tips.
This course was published in the October 2011 issue and expires October 31, 2014. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the relationship between radiation exposure and image quality.
- Relay the effect of digital sensors’ smaller recording dimensions on image specificity.
- Identify strategies for avoiding horizontal overlap.
- Explain how image reception size and position affect image capture.
- List the benefits of instantaneous image viewing.
RADIATION EXPOSURE
The benefits of digital imaging are well documented. The most notable advantage is the reduction of radiation exposure required to produce diagnostic-quality images. However, there is no standardization of dose reductions among digital imaging manufacturers. While film speeds have been categorized by the American National Standards Institute and the International Organization for Standardization, there is no equivalent on which to base digital image receptors.1,2
Estimates indicate that digital imaging can reduce radiation exposure up to 50% over the dose required for F-speed film.3 But some digital systems may not reduce radiation exposure at all,4 and some indirect digital panoramic imaging systems actually require more radiation exposure than film-based panoramic radiography.4–6This slight increase in radiation exposure, however, is considered acceptable because of the technology’s other benefits, including instantaneous viewing of the image and elimination of processing chemicals.
To improve diagnostic quality when switching from film-based radiography to digital imaging, the manufacturer’s recommended exposure settings should be carefully evaluated. If the radiation exposure setting is reduced too much, electronic noise—the equivalent of film fogging—can result, which lowers image contrast. If an image appears gray or grainy, the radiation exposure setting is probably too low. Practitioners often aggressively reduce radiation exposure when they first begin using a storage phosphor system (indirect digital imaging) with a photostimuable phosphor (PSP) plate. In general, indirect digital imaging systems require higher radiation exposure settings than direct digital systems.7 Direct digital imaging systems use a solid state sensor-based on charge-coupled device (CCD) or complementary metal-oxide-semiconductor (CMOS) technology, and usually tolerate a greater reduction in exposure without creating electronic noise. Careful evaluation of the images produced at various levels will help determine the ideal settings.

Reducing patient exposure to radiation is an important benefit of digital radiography, but it is quickly negated when careless technique leads to an abundance of retakes. In medicine, some reports show that digital radiography has an increased rate of retakes than film-based radiography.3 Practitioners may feel justified in retaking more radiographs, due to the ease of capture and the reduction in radiation exposure.8 The fact that many digital imaging systems reduce the level of radiation exposure should not lead to careless technique.
SMALLER RECORDING DIMENSIONS
The smaller recording dimensions of a digital sensor or PSP plate may also cause an increase in exposures. One of the first problems noted with digital imaging is the missing of important anatomy. To compensate for the smaller recording dimensions, manufacturers often recommend taking additional exposures. Another option is to alter the vertical or horizontal angulation of the X-ray beam to project the desired area onto the image receptor (Figure 1).
Smaller recording dimensions often result in cutting off the apices of the teeth on periapical radiographs. Wired sensors can make it difficult to place the image receptor far enough forward in the oral cavity to record the distal edge of the canines when exposing bitewing radiographs. These problems can be corrected by directing the vertical and horizontal angulations toward the image receptor. As long as the angulation is not shifted more than 15º away from perpendicular, the image will remain diagnostic, while recording portions of the anatomy that appear just beyond the dimensions of the sensor.
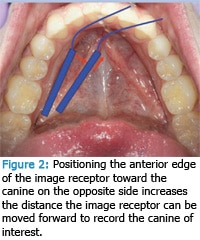
On premolar bitewing or periapical radiographs, position the anterior edge of the sensor farther away from the lingual surfaces of the teeth so the distal edges of the canines are recorded. To avoid overlap error in this angled position, move the sensor toward the middle of the oral cavity and guide the anterior edge of the sensor forward, closer to the canine on the opposite side (Figure 2).
AVOID HORIZONTAL OVERLAP
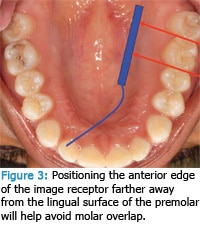
The size of digital sensors can compromise precise placement parallel to the desired teeth’s embrasures, which may cause overlap. The most common areas for overlapping error are the maxillary first molars with the maxillary second molars, and distal edges of the canines with the premolars. The maxillary first molar-second molar overlap often results because of the large rhomboid shape of the first molar. To rectify this problem, the image receptor can be placed as if taking a premolar radiograph (Figure 3). Position the anterior edge of the image receptor farther from the lingual surface of the premolar to help avoid overlap.
Anatomy also plays a role in producing overlap of the distal edge of the canine with the first premolar. The wide dimension of the first premolar will superimpose the lingual cusp onto the image of the canine. To avoid or minimize this overlap, shift the horizontal angulationof the tube head so the X-ray beam intersects the canine from a slightly distomesial position. If the tube head shift is less than 15º, little to no overlapping of the canine and premolar contact will occur.
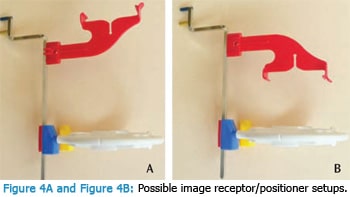
IMAGE RECEPTOR HOLDERS/POSITIONERS
The weight of the digital sensor, when combined with an image receptor holder/positioner, often contributes to bitewing radiographs that record more of the mandibular arch than the maxilla. Experimenting with image receptor holders of different sizes and weights may help avoid this error. Some manufacturers also make holders/positioners specifically designed to work with their image receptor.
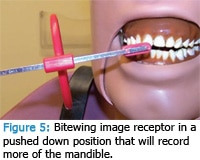
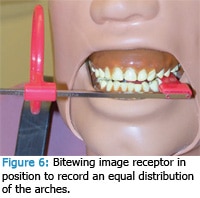
Figure 4A and Figure 4B show a commonly used holder/positioner. The assembly pictured in Figure 4A requires the patient to occlude on the bite block on the same side as the area of interest. If the patient has difficulty closing down completely, an unequal distribution of the arches will be recorded. Additionally, if the facial cusps of the maxillary posterior teeth are slightly longer than average, the image receptor and holder assembly will be pushed down excessively (Figure 5).9 Increasing the vertical angulation will compensate for this forceddown position as long as the increase does not exceed 15º. Another solution is to assemble the holder/positioner as illustrated in Figure 4B. This setup allows the patient to occlude on the opposite side of the area of interest and avoid the forceddown position of the holder/positioner (Figure 6).
Another common holder/positioner is the stick-on plastic tab or bite block. Careful attention must be paid to where the holders are affixed to the sensor. Failure to place the holder in the correct position may result in completely missing the area of interest (Figure 7). The advantage of this holder is its flexibility. By altering its position, the operator can ensure that the image receptor is lined up behind the area of interest (Figure 8).
The position of all types of holders/positioners should be evaluated once the patient has occluded completely. Due to the oversized physical dimensions of a digital sensor, the sensor is often moved deep into the oral cavity, away from the supporting structures of the teeth, in order to make it fit. While acceptable, the teeth should not occlude beyond the bite block because the incisal edges will not be recorded (Figure 1). If the image receptor holder/positioner can not be repositioned correctly, the vertical angulation may be adjusted to project the incisal edges onto the image, as long as the shift is less than 15º.
![]() INSTANTANEOUS IMAGE VIEWING
INSTANTANEOUS IMAGE VIEWING
An important advantage of direct digital imaging is the ability to see the image instantly. To reap the benefits of this feature, the sensor should be kept in position while the image is evaluated on-screen. Adjustments can then be made to the tube head or sensor position before additional exposures are taken. The patient needs to understand and be able to cooperate with this protocol. If an error has compromised the diagnostic quality of the image, the cause must be determined and a corrective action identified before retaking the exposure. The ability to evaluate the image while the sensor and X-ray tube head remain in position can increase the success of a retake.
For example, if an incorrect horizontal mesiodistal angle caused the overlap, the clinician can adjust the tube head to direct the horizontal angulation at a more distomesial angle while the sensor remains in position. If the overlapping resulted from the sensor not being positioned parallel to the embrasures of the teeth of interest, direct the patient to open slightly and correctly align the sensor. The ability to instantaneously critique the image for diagnostic quality while evaluating the position of the sensor and X-ray tube head angulation can assist the clinician in determining the appropriate corrective action.
![]() CONSIDERATIONS FOR THE DIGITAL FUTURE
CONSIDERATIONS FOR THE DIGITAL FUTURE
The ability to assess radiographic images immediately and simultaneously is changing the way radiographs are taken. As technology advances, adaptations to technique will be required. New strategies for obtaining diagnostic-quality radiographs will also emerge. For example, the recording dimension size of a digital image receptor may require that more radiographs are taken to complete a fullmouth series and the increased physical dimensions of the digital image receptor may eliminate the need for premolar bitewings to record the distal edge of the canines. Technology may one day allow the clinician to place an image receptor and determine the correct angulations for the X-ray beam with a few key strokes on a computer.
References
- Photography-intraoral Dental Radiographic Film-specification. New York: American National Standards Institute; 1997.
- Photography-direct Exposing Medical and Dental Radiographic Film Process Systemsdetermination of ISO Speed and ISO Average Gradient. New York: American National Standards Institute; 1983.
- Van der Stelt PF. Better imaging: the advantages of digital radiographs. J Am Dent Assoc. 2008;139:7S–13S.
- Van der Stelt PF. Filmless imaging: the uses of digital radiography in dental practice. J Am Dent Assoc. 2005;136:1379–1387.
- Horner K, Drage N, Brettle D. 21st Century Imaging. London: Quintessence Publishing; 2008.
- Angelopoulous C, Bedard A, Katz JO, Karamanis S, Parissis N. Digital panoramic radiography: an overview. Semi Orthod. 2004;10:194–203.
- White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation. 6th ed. St. Louis: Elsevier; 2009.
- Thomson EM, Johnson ON. Essentials of Dental Radiography for Dental Assistants and Hygienists. 9th ed. Upper Saddle River, NJ: Pearson Education; 2012.
- Thomson EM. Exercises in Oral Radiography Techniques: A Laboratory Manual. 3rd ed. Upper Saddle River, NJ: Pearson Education; 2012.
From Dimensions of Dental Hygiene. October 2011; 9(10): 58-61.

 INSTANTANEOUS IMAGE VIEWING
INSTANTANEOUS IMAGE VIEWING CONSIDERATIONS FOR THE DIGITAL FUTURE
CONSIDERATIONS FOR THE DIGITAL FUTURE