Preventing Bone Loss
While tooth extraction can often lead to bone loss, oral health professionals can use a variety of strategies to encourage bone health.
INTRODUCTION

Dental hygienists specialize in the prevention and treatment of oral disease, all while helping patients maintain their full dentition. Unfortunately, tooth loss is sometimes inevitable due to decay, periodontal diseases, or trauma. Upon tooth extraction, the gradual loss of bone and oral complications may ensue.
As dentistry continues to evolve, the ability to regenerate bone has expanded to include several new procedures. In the past when a tooth was removed, the solution was to place a bridge or a partial denture. Today, restoration is possible through implant therapy. The ability to place an implant, however, may be compromised by the lack of bone support needed to restore bone height. This month, Sebastiano Andreana, DDS, MS, shares his expertise on advances in surgical procedures and the materials used to fill empty sockets, in addition to discussing the role of dental hygienists in supporting these techniques.
Tooth loss can have devastating effects on both oral and systemic health and is most often caused by oral diseases such as dental caries and periodontal diseases, as well as root fractures, trauma, and orthodontic treatment.1–3 Tooth loss is affected by socioeconomic factors and is found more often among indigent populations.4–6 Age, education, access to dental care, dentist/population ratios, and insurance coverage also affect the prevalence of tooth loss.4,7,8 In the United States, the prevalence of tooth loss has declined since the 1970s; however, some groups remain more deeply affected than others. According to the National Health and Nutrition Examination Survey, older adults, black adults, smokers, and those with lower incomes and less education have fewer remaining teeth (Table 1).9
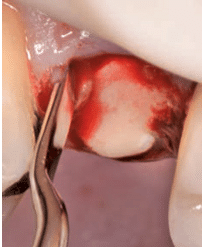
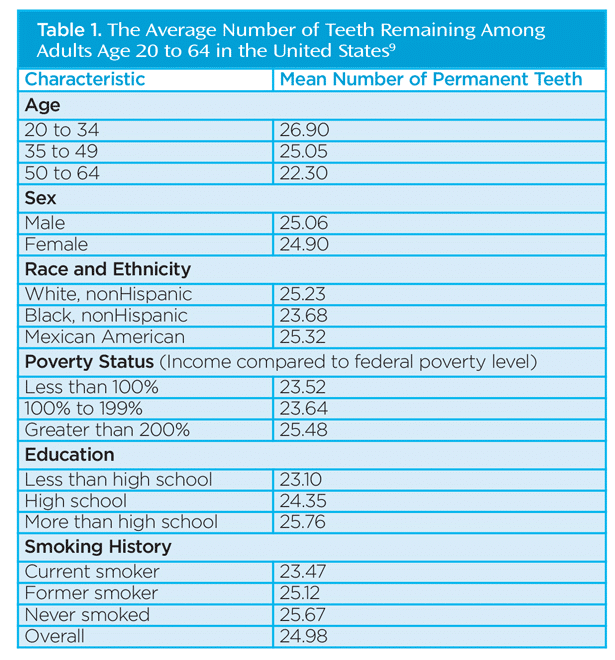 Approximately 20 million teeth are extracted every year in the US.1 Typical consequences of tooth extraction include loss of hard tissues, accompanied by alterations of adjacent soft tissues. According to Watzek,10 tooth loss is the single most important factor underlying alveolar bone loss. Classic, early studies by Atwood2 and Johnson3 showed that tooth extraction is followed by loss of alveolar bone. Highly detailed studies by Lekovic et al11 and Barone et al12 reported that bone loss at the site of the extraction is more prominent in the buccolingual dimension, particularly on the facial aspect of the socket, accompanied by minor but still recordable vertical bone loss. The combination of vertical and horizontal bone loss is classified as a Siebert Class III defect, representing a clinical challenge for oral health professionals. A reduced alveolar ridge with a defect visible mostly in the facial site is also due to bone loss (Figure 1). Typically, the bone loss progresses more rapidly in the first 6 months. Rates of progression vary, with Carlsson and Persson13 reporting an initial progression rate of 23% and an additional 11% within 2 years. On the other hand, Ashman and Bruins14 report the resorption rate at 40% to 60% within the first 2 years to 3 years, continuing at an annual rate of 0.25% to 0.5%.
Approximately 20 million teeth are extracted every year in the US.1 Typical consequences of tooth extraction include loss of hard tissues, accompanied by alterations of adjacent soft tissues. According to Watzek,10 tooth loss is the single most important factor underlying alveolar bone loss. Classic, early studies by Atwood2 and Johnson3 showed that tooth extraction is followed by loss of alveolar bone. Highly detailed studies by Lekovic et al11 and Barone et al12 reported that bone loss at the site of the extraction is more prominent in the buccolingual dimension, particularly on the facial aspect of the socket, accompanied by minor but still recordable vertical bone loss. The combination of vertical and horizontal bone loss is classified as a Siebert Class III defect, representing a clinical challenge for oral health professionals. A reduced alveolar ridge with a defect visible mostly in the facial site is also due to bone loss (Figure 1). Typically, the bone loss progresses more rapidly in the first 6 months. Rates of progression vary, with Carlsson and Persson13 reporting an initial progression rate of 23% and an additional 11% within 2 years. On the other hand, Ashman and Bruins14 report the resorption rate at 40% to 60% within the first 2 years to 3 years, continuing at an annual rate of 0.25% to 0.5%.
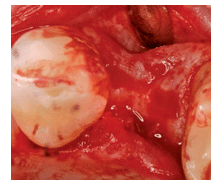
The bone loss at the extraction site is even greater in the presence of sockets that have lost one or more walls due to periodontal diseases, endodontic pathologies, and trauma.15 Several reviews16–18 have concluded that tooth extraction leads to malformations of the site, which could jeopardize the ability to place implants without complex surgical procedures. A fixed dental prosthesis can be placed as an alternative to implant placement to replace the missing tooth; however, with bone loss and soft tissue reduction, root exposure can occur, leading to root caries and compromising the bridge’s longevity. The complexity of this clinical situation has led to the development of methods to minimize or prevent bone loss following tooth extraction. Techniques and materials have been proposed, including different extraction techniques, followed by manipulating the alveolar soft tissue adjacent to the extraction sockets and addressing the filling of the socket with materials that eventually minimize bone loss.
CHANGES IN SURGICAL TECHNIQUE
The surgical technique used during tooth extraction is of paramount importance. Lisowski reported in 1945 that when performing a dental extraction, “Extensive surgery was contraindicated and that the resultant alveolar resorption was aggravated proportionately to the increase in the extent of surgery.”19 This could be interpreted as the first indication for what is known as “atraumatic extraction,” a gentle procedure that attempts to minimize the inflammatory processes after extraction. Inflammation adjacent to bone and within the bone leads to bone loss, as seen in periodontitis and endodontic lesions.
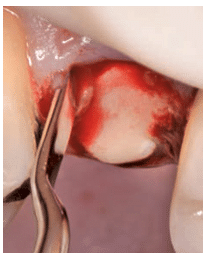
The atraumatic technique involves luxating the roots by using fine periotomes, aiming at preserving the alveolar walls (Figure 2).20 Previously, tooth extraction was performed and then the socket fill was done with a flap approach.21–23 Barone et al12 reported the clinical outcomes of flapless vs flap tooth extraction. The flap approach was used to facilitate the extraction and to encourage primary closure of the socket. The flaps were raised before tooth extraction. Further investigations addressed the fact that once the periosteum is removed from the bone, bone loss occurs at approximately 0.5 mm to 0.8 mm.24,25 The bone loss, which occurs primarily on the buccal soft tissue, is caused by a reduction in the blood supply at the bone surface and the inflammatory response initiated by the surgical trauma. Due to these physiological events, flapless extraction techniques have been introduced.20,26 The flapless approach is better for soft tissue healing and patient comfort, as well as minimizing bone loss after tooth extraction. It does not, however, allow for covering the grafted material. For this purpose, membranes of different materials have been used, including collagen and polylactic acid (Figure 3).27,28
MATERIALS USED TO FILL EMPTY SOCKETS
The materials used to fill empty sockets are divided into four groups: bone from the same patient (autograft); bone from donors of the same species; bone from donors of different animal species (xenograft); and synthetic bone.
Biologically, bone from the same patient would seem to be ideal. The bone is harvested from the patient from a different site than the socket itself. This technique, however, may lead to increased morbidity and increased discomfort for patients. The use of human bone from donors is also very common in the US. Several clinical studies have reported the use of demineralized freeze-dried bone allograft (DFDBA) and nondemineralized freeze-dried bone allograft (FDBA). Jambhekar et al26 summarized the clinical outcomes of these studies, which were conducted with a flapless approach. The authors reported a mean bone loss of 1 mm (in width) following the combined use of FDBA and DFDBA; 1.65 mm when only FDBA was used; and 2.18 mm when only DFDBA was used in a flapless approach. They also reported a buccal wall height of at least 0.37 mm when DFDBA was used and 0.8 mm when the combined approach was implemented.
The use of xenograft, or bone from bovine, equine, or porcine origin, is common in Europe. Similar to the results seen in humans, there was a typical bone loss of 1.3 mm in the buccolingual dimension, indicating a small narrowing of the alveolar ridge, and an average reduction of 0.57 mm at the crest in the coronoapical direction.
Synthetic bone materials have also been widely used in clinical practice. Among those, medical-grade calcium sulfate, hydroxyapatite, calcium phosphosilicate putty (bioglass), and beta-tricalcium sulfate are the most common. The clinical outcomes in terms of bone loss after socket fill with synthetic material is similar to the results found when other graft materials of biological origins are used.26
These materials may be used in combination with one another or mixed with human blood derivatives, such as platelet-rich plasma.27,29 Recently, platelet-rich fibrin has been added to the material armamentarium. Human recombinant technology has also been used successfully.22
Regardless of the material used, the graft material needs to be covered so it does not fall out of the socket and to prevent food debris from contaminating the graft. Covering the graft also provides a favorable environment for the gingival epithelium and fibrous connective tissue to close the socket, enabling soft tissue to protect the site while the graft material is turned into live, viable bone. Following successful bone regeneration within the socket and the preservation of healthy gingival tissues, a predictable implant placement is likely.30
A material composed of beta-tricalcium sulfate particles and coated with poly(lactide-co-glycolide) has been used as a membrane alone for several years. Because the beta-tricalcium phosphate particles are coated with a membrane material, a conventional membrane may not always be necessary.
ROLE OF THE DENTAL HYGIENIST
Regardless of the technique, materials used, and patient health status, the healing socket has to be monitored and managed. Dental hygienists are well positioned to assess the health of sockets at recare appointments and administer topical or local antimicrobials and wound healing promoters as needed.31,32 Patients undergoing bone regeneration need frequent recare appointments to reduce the bacterial burden. Scaling and root planing should be performed at 3-month to 4-month intervals. Patients should also receive intense oral hygiene education to ensure a high level of self-care, as well as dietary counseling to reduce the amount of sugar and acid consumed in order to decrease bacteria counts. If applicable, tobacco cessation therapies should be provided. Patients may also want to consider taking a vitamin C supplement, as it repairs and supports connective tissue.33
CONCLUSION
Tooth extraction is a common procedure in dentistry necessitating that oral health professionals be prepared to help patients prevent bone loss post-surgery. This is accomplished by using the most appropriate surgical techniques, filling the socket with materials that will encourage bone growth, and helping patients make the best decisions about their oral and systemic health to support a healthy environment in the oral cavity.
REFERENCES
- Encyclopedia of Surgery. Tooth Extraction. Available at: surgeryencyclopedia.com/St-Wr/Tooth-Extraction.html. Accessed March 20, 2015.
- Atwood DA. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971;26:266–279.
- Johnson K. A study of the dimensional changes occurring in the maxilla following tooth extraction. Aust Dent J. 1969;14:241–244
- Emami E, de Souza RF, Kabawat M, Feine JS. The impact of edentulism on oral and general health. Int J Dent. 2013;2013:498305.
- Millar WJ1 Locker D. Edentulism and denture use. Health Rep. 2005;17:55–58.
- Bedos C, Brodeur JM, Boucheron L, et al. The dental care pathway of welfare recipients in Quebec. Soc Sci Med. 2003;57:2089–2099.
- Elani HW, Harper S, Allison PJ, Bedos C, Kaufman JS. Socio-economic inequalities and oral health in Canada and the United States. J Dent Res. 2012;91:865–870.
- Brodeur JM, Benigeri M, Olivier M, Payette M. [Use of dental services and the percentage of persons possessing private dental insurance in Québec]. J Can Dent Assoc. 1996;62:83–90.
- National Insitute of Dental and Craniofacial Research. Tooth Loss in Adults (Age 20 to 64). Available at: nidcr.nih.gov/DataStatistics/ FindDataByTopic/ ToothLoss/ToothLossAdults20to64.htm. Accessed March 20, 2015.
- Watzek G. Implants in Qualitatively Compromised Bone. London: Quintessence Publishing; 2004.
- Lekovic V, Kenney EB, Weinlaender M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction: report of 10 cases. J Periodontol. 1997;68:563–570.
- Barone A, Aldini NN, Fini M, Giardino R, Calvo Guirado JL, Covani U. Xenograft versus extraction alone for ridge preservation after tooth removal: a clinical and histomorphometric study. J Periodontol. 2008;79:1370–1377.
- Carlsson GE, Persson G. Morphologic changes of the mandible after extraction and wearing of dentures. A longitudinal, clinical, and X-ray cephalometric study covering 5 years. Odontol Revy. 1967;18:27–54.
- Ashman A, Bruins P. Prevention of alveolar bone loss postextraction with HTR grafting material. Oral Surg Oral Med Oral Pathol. 1985;60:146–153.
- Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74:990–999.
- Jahangiri L, Devlin H, Ting K, Nishimura I. Current perspectives in residual ridge remodeling and its clinical implications: a review. J Prosthet Dent. 1998;80:224–237.
- Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36:1048–1058.
- Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014;93:950–958.
- Lisowki CS. A comparative study of the resorption of alveolar ridge tissue under immediate dentures. Dent Res Grad Study. 1944-1945;45:11–13.
- Kutkut A, Andreana S, Monaco E. Esthetic consideration for alveolar socket preservation prior to implant placement: description of a technique and 80-case series report. Gen Dent. 2012;60:398–403.
- Camargo PM, Lekovic V, Weinlaender M, et al. Influence of bioactive glass on changes in alveolar process dimensions after exodontia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:581–586.
- Fiorellini JP, Howell TH, Cochran D, et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol. 2005;76:605–613.
- Lekovic V, Camargo PM, Klokkevold PR, et al. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998;69:1044–1049.
- Tavtigian R. The height of the facial radicular alveolar crest following apically positioned flap operations. J Periodontol. 1970;41:412–428.
- Wood DL, Hoag PM, Donnenfeld OW, Rosenfeld LD. Alveolar crest reduction following full and partial thickness flaps. J Periodontol. 1972:43:141–144.
- Jambhekar S, Kernen F, Bidra AS. Clinical and histologic outcomes of socket grafting after flapless extraction: a systematic review of randomized controlled clinical trials. J Prosthet Dent. 2015 Mar 4. Epub ahead of print.
- Kutkut A, Andreana S, Kim HL, Monaco E Jr. Extraction socket preservation graft before implant placement with calcium sulfate hemihydrate and platelet-rich plasma: a clinical and histomorphometric study in humans. J Periodontol. 2012;83:401–419.
- Poulias E, Greenwell H, Hill M, et al. Ridge preservation comparing socket allograft alone to socket allograft plus facial overlay xenograft: a clinical and histologic study in humans. J Periodontol. 2013;84:1567–1575.
- Intini G, Andreana S, Margarone JE, Bush PJ, Dziak R. Engineering a bioactive matrix by modifications of calcium sulfate. Tissue Eng. 2002;8:997–1008.
- Kutkut A, Andreana S, Monaco E, Jr. Clinical and radiographic evaluation of single-tooth dental implants placed in grafted extraction sites: a one-year report. J Int Acad Periodontol. 2013;15:113–124.
- Sunkara S, Beneduce C, Andreana S. Socket preservation and implant insertion in a smoker with a 10-year history of bisphosphonate use: a case report. J Long Term Eff Med Implants. 2010;20:327–334.
- de Araújo Nobre M, Cintra N, Maló P. Peri-implant maintenance of immediate function implants: a pilot study comparing hyaluronic acid and chlorhexidine. Int J Dent Hyg. 2007;5:87–94.
- Nishida M, Grossi SG, Dunford RG, Ho AW, Trevisan M, Genco RJ. Dietary vitamin C and the risk for periodontal disease. J Periodontol. 2000;71:1215–1223.
From Dimensions of Dental Hygiene. January 2015;13(1):19–22.

