Prevent Infective Endocarditis
The debate over whether antibiotic prophylaxis is necessary to prevent this life-threatening infection remains ongoing.
This course was published in the January 2016 issue and expires January 31,2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain why prophylactic antibiotic premedication is now less favored.
- Discuss appropriate protocols for those patients still recommended for prophylactic antibiotic medication.
- Identify evidence that suggests that the debate about prophylactic antibiotic medication is not over.
Infective endocarditis is a rare but life-threatening infection of the endocardium that affects the heart valves and neighboring structures. It is caused by a variety of bacteria and fungi. While the oral cavity harbors more than 700 strains of bacteria, only a small number are associated with infective endocarditis, including Staphylococci and Viridans streptococci as well as Enterococcus, Pseudomonas, and Serratia species. The fungus Candida is another cause.1–3 The incidence of infective endocarditis ranges from five cases to seven cases per 100,000 people each year. Women are more likely to develop infective endocarditis than men.4 Post-surgical infections of prosthetic joints are also rare, but the mechanisms for infection appear similar to infective endocarditis.
While a healthy immune system typically prevents circulating microbes from causing harm, circulating bacteria can cause problems throughout the body in some individuals. The valves of the heart, as well as implanted orthopedic devices are typical targets. Bacteremia (presence of bacteria in the bloodstream) appears to be related to activities of daily living, such as eating and performing oral hygiene like flossing and toothbrushing (Table 1).1–3,5–7 The presence of dental disease, such as periodontitis, may also increase the incidence of bacteremia.6
To limit the likelihood of infective endocarditis and prosthetic joint infections, the American Dental Association (ADA), American Heart Association (AHA), and American Academy of Orthopaedic Surgeons (AAOS) previously recommended prophylactic antimicrobial therapy for patients with certain heart conditions and some or all patients with prosthetic joints prior to invasive dental procedures. However, this is no longer the case. Recent reviews of the scientific evidence suggest that the risk of adverse reactions to antibiotic therapy may outweigh the benefits of prophylaxis for most patients because the bacteria most often cultured from these infections do not appear to be of oral origin (Table 2).8,9 Authors have noted that the increased use of antibiotics, insufficient controls on drug prescriptions, and inadequate compliance with treatment regimens have resulted in increased resistance of bacteria to antibiotics.2,5,9–13 These observations, along with the fact that bacteremias commonly occur, led the ADHA and AHA to revise long-standing recommendations for antibiotic premedication for patients who may be prone to infective endocarditis.2,5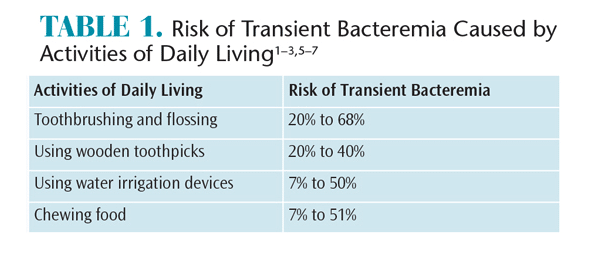
DECIDING WHO NEEDS ANTIBIOTIC PROPHYLAXIS TO PREVENT INFECTIVE ENDOCARDITIS
The updated AHA guidelines suggest there may be instances in which the use of antibiotics remains indicated for small numbers of patients.2,5,13 The guidelines recommend antibiotic prophylaxis only for patients with certain preexisting vascular conditions associated with the highest risk of adverse outcomes from infective endocarditis.2 It remains unclear if these patients are more prone to developing the infection. Patients with the following conditions may require antibiotic prophylaxis:
- One or more prosthetic cardiac valves or implanted prosthetic material used for cardiac valve repair
- History of endocarditis
- Valvulopathy (disease or disorder of the heart valves) following heart transplantation
- Heart diseases:
- Unrepaired cyanotic congenital heart disease, including palliative shunts and conduits
- Completely repaired congenital heart defect with prosthetic material or device, whether placed by surgery or catheter, during the first 6 months after the repair procedure; this is because endothelialization (formation of endothelial tissue) over prosthetic material is thought to consistently occur within 6 months of implantation
- Any repaired congenital heart defect with residual defect at the site or adjacent to the site of a prosthetic patch or a prosthetic device that is thought to inhibit endothelialization
![]()
After publication of the new AHA guidelines, a number of research studies have been conducted in the United States to examine the impact of these new guidelines on the incidence of infective endocarditis within the first 2 years after implementation.14–17 The studies found no evidence of increased incidence for infective endocarditis. A similar study was conducted in England after the National Institute for Health and Clinical Excellence recommended cessation of antibiotic prophylaxis for infective endocarditis prevention in 2008.18 Similar to the studies in the US, the study found no early changes in the incidence of infective endocarditis after 2 years of implementation. Analysis of 5-year data, however, revealed the incidence of infective endocarditis had significantly increased in England. In light of the fact that this study was not designed to demonstrate causality, the authors suggested a need for additional studies to explore the temporal association between changes in guidelines and increased incidence. While questioning some aspects of this study’s methodology, the ADA Council of Scientific Affairs also recommended additional research on the subject.19 In the meantime, the ADA suggested that dental professionals adhere to the most recent AHA guidelines regarding antibiotic prophylaxis and infective endocarditis.19
For many years, dental procedures have been considered a potential cause of infections that threaten orthopedic implants. Therefore, premedication prior to dental procedures was common for patients with joint replacements. Premedication was also routinely prescribed for patients with other implants, such as orthopedic screws, pins, etc. In 2013, the ADA and AAOS published updated, evidence-based guidelines that recommended dental professionals consider discontinuing the routine prescription of prophylactic antibiotics for patients with prosthetic joints.1,3,5,20–24
In 2014, a new review of antibiotic prophylaxis for patients with orthopedic implants was conducted by the ADA alone.5 This review, like the combined AAOS/ADA review published in 2013, found no association between dental procedures and prosthetic joint infections. The ADA review concluded more definitively that the use of prophylactic antibiotics prior to dental procedures was not recommended for patients with prosthetic joint implants. In January 2015, the ADA Council on Scientific Affairs continued to discourage prophylactic antibiotic use for most patients with prosthetic joint implants. However, it also reminded practitioners and patients to consider the use of antibiotic prophylaxis in clinical circumstances that pose a significant medical risk to the patient.5,21–23
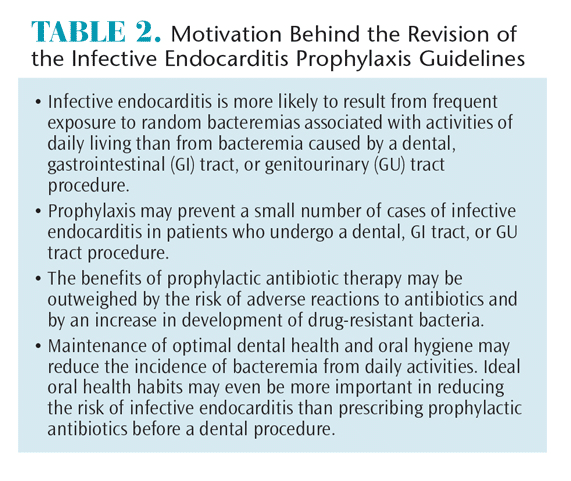
According to the AHA, antibiotic prophylaxis is recommended only for patients with conditions associated with the highest risk of infective endocarditis who will receive dental procedures that involve perforation of oral mucosa and manipulation of gingival tissues and/or periapical region of teeth. There is a wide variation in reported frequencies of bacteremia in patients receiving invasive dental procedures (Table 3).2,3,5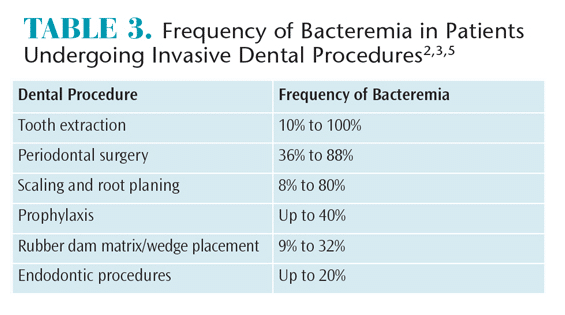
In light of the flurry of recent recommendations—as well as the data revealing an increasing incidence of infective endocarditis in England in the wake of ending antibiotic premedication for patients historically thought prone to the infection—the dental professional and the individual patient must weigh the risks and benefits of antibiotic use. It may be prudent to consult the patient’s cardiologist or orthopedist if doubt exists on whether the patient should receive antibiotic prophylaxis.25
IMPLEMENTING AN APPROPRIATE PROTOCOL
A decision to use a certain type of antibiotic should be based on a thorough medical and dental history with emphasis on the effects of past antibiotic use. Practitioners need to be especially aware of any previous adverse reactions to relevant antibiotics. Current medications and the possibilities for drug interactions, and risks of microbial resistance are other important considerations.3,9–11,20 Practitioners should select an antibiotic that is active against the pathogens likely to cause the relevant infection. For example, recent studies suggest that S. aureus appears to be the most common cause of acute infective endocarditis, as well as the late infections of prosthetic joints at which antibiotic prophylaxes are aimed.
There is also evidence that oral microflora is becoming increasingly more resistant to antibiotics.3,9–11,20 Repeated use of antibiotics can lead to antibiotic-resistant microorganisms in the oral cavity. Maintaining an interval of at least 10 days to 14 days between dental appointments to allow the patient’s normal oral flora to re-establish is recommended.2,10,12
The AHA and the ADA suggest that patients already on chronic antibiotic therapy should be prescribed an antibiotic from a different class for infective endocarditis prophylaxis, rather than increasing the dosage of the current antibiotic. For example, if the patient is taking amoxicillin, the practitioner might select clindamycin, azithromycin, or clarithromycin for prophylaxis.1,10,13,26 Patients who are allergic to penicillin can be treated 1 hour before the dental procedure with an alternate antibiotic such as second-generation erythromycin, azithromycin, or clarithromycin.
Amoxicillin (for patients not allergic to penicillin or cephalosporin drugs) is the preferred choice for oral therapy because it is well absorbed in the gastrointestinal tract and provides high and sustained serum concentrations. Two grams of amoxicillin is sufficient to reach adequate serum levels for several hours, and the inhibitory effect of the drug is enough to eliminate the need for a post-operative dose.2,12 Patients who are unable to take medications orally can be treated with an antibiotic injection 30 minutes prior to the procedure. For example, 2 g of intramuscular or intravenous ampicillin can be administered. To prevent possible cross-reactions, cephalosporin should not be administered to patients with a history of anaphylaxis, angioedema, or urticaria after treatment with any form of penicillin, including ampicillin or amoxicillin.
There are no current recommendations for antibiotic premedication for dental patients with prosthetic implants. In the wake of the ADA’s 2015 recommendations, which were developed and published independent of the AAOS, both organizations are now involved in a joint effort to develop appropriate use criteria to better guide future behaviors.
Prophylactic antibiotics should be consumed in a single dose 30 minutes to 60 minutes prior to dental treatment. This allows the antibiotic to reach adequate blood levels, thereby limiting the viability of bacteria introduced into the bloodstream. For individuals who are to be premedicated, practitioners must always ask if the patient has consumed the prescribed drugs before starting a dental procedure. If a patient has failed to take the prescribed drugs, it is unclear whether they should be treated until the prophylactic drug has been consumed.2 If the dental practitioner elects to proceed with treatment, the AHA recommends administering the appropriate prophylactic dose with 2 hours (Table 4).2

SUMMARY
The effectiveness of antibiotic prophylaxis to prevent infective endocarditis or prosthetic joint infection is questionable. Furthermore, serious risks are associated with adverse reactions to antibiotics. Antibiotic misuse and overuse also lead to the development of antibiotic-resistant bacteria. In response, the updated AHA guidelines for antibiotic prophylaxis to prevent infective endocarditis include recommendations that strictly limit premedication to small numbers of patients for whom contracting infective endocarditis would likely cause major morbidities or death. Short-term studies in the US have not reported an increased incidence of infective endocarditis during the interval subsequent to the current AHA guidelines. However, a longer study in England suggests that the incidence of infective endocarditis has increased significantly since the end of antibiotic prophylaxis.
Acknowledging the downsides to antibiotic use mentioned above and in light of limited supportive evidence, combined AAOS-ADA recommendations in 2013 suggested that practitioners consider not premedicating certain patients with orthopedic implants. For reasons unclear, in early 2015 the ADA published newer guidelines independent of the AAOS that recommended no prophylactic antibiotics for dental patients with orthopedic implants. The AAOS and ADA have since collaborated to establish joint appropriate use criteria for premedication, which should be released soon.
The ADA suggests that practitioners use their discretion to decide whether a particular patient receives antibiotic prophylaxis. Therefore, it is important for health care practitioners to consider antibiotic prophylaxis recommendations based on patients’ individual situations and to consult with patients’ cardiologists and/or orthopedists.
References
- American Dental Association. Antibiotic Prophylaxis for Heart Patients. Available at: mouthhealthy.org/en/az-topics/a/Premedication-or-Antibiotics. Accessed December 9, 2015.
- Wilson W, Taubert KA, Gevitz M, et al. Prevention of infective endocarditis: Guidelines from the American Heart Association—A Guideline From the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc. 2007;138:739–745.
- American Academy of Pediatric Dentistry. Guideline on Antibiotic Prophylaxis for Dental Patients at Risk for Infection. Available at: aapd.org/media/Policies_Guidelines/G_AntibioticProphylaxis.pdf. Accessed December 9, 2015.
- Correa de Sa DD, Tleyjeh IM, Anavekar NS, et al. Epidemiological trends of infective endocarditis: A population based study in Olmsted County, Minnesota. Mayo Clin Proc. 2010;85:422–426.
- Sollecito TP, Abt E, Lockhart PB, et al. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: Evidence-based clinical practice guideline for dental practitioners–a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146:11–16.
- Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis related bacteremia. J Am Dent Assoc. 2009;140:1238–1244.
- Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK. Bacteremia associated with tooth-brushing and dental extraction. Circulation. 2008;117:3118–3125.
- Oliver R, Roberts GJ, Hooper L, Worthington HV. Antibiotics for the prophylaxis of bacterial endocarditis in dentistry. Cochrane Database Syst Rev. 2013;10:CD003813.
- Enzler MJ, Berbari E, Osmon DR. Antimicrobial prophylaxis in adults. Mayo Clin Proc. 2011;86: 686–701.
- American Dental Association Council of Scientific Affairs. Combating antibiotic resistance. J Am Dent Assoc. 2004;135:484–487.
- Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001;345:1318–1130.
- Weinberg MA, Westphal CT, Fine JB. Oral Pharmacology for the Dental Hygienist. 2nd ed. Upper Saddle River, New Jersey: Pearson Education; 2012.
- American Dental Association. Antibiotic Prophylaxis. Available at: ada.org/en/member-center/oral-health-topics/antibiotic-prophylaxis. Accessed December 9, 2015.
- Desimone DC, Tleyjeh IM, Correa de Sa DD, et al. Incidence of infective endocarditis caused by viridans group streptococci before and after publication of the 2007 American Heart Association’s endocarditis prevention guidelines. Circulation. 2012;126:60–64.
- Pasquali SK, He X, Mohamad Z, et al. Trends in endocarditis hospitalizations at US children’s hospitals: impact of the 2007 American Heart Association Antibiotic Prophylaxis Guidelines. Am Heart J. 2012;163:894–899.
- Rogers AM, Schiller NB. Impact of the first nine months of revised infective endocarditis prophylaxis guidelines at a university hospital: so far so good. J Am Soc Echocardiogr. 2008;21:775.
- Bikdeli B, Wang Y, Kim N, Desai MM, Quagliarello V, Krumholz HM. Trends in hospitalization rates and outcomes of endocarditis among Medicare beneficiaries. J Am Coll Cardiol. 2013;62:2217–226.
- Dayer MJ, Jones S, Prendergast B, Baddour LM, Lockhart PB, Thornhill MH. Incidence of infective endocarditis in England, 2000–13: a secular trend, interrupted time-series analysis. Lancet. 2015;385:1219–1228.
- ADA News. Lancet article suggests increase in infective endocarditis tied to reduction in antibiotics use. Available at: ada.org/en/publications/ada-news/2014-archive/december/lancet-article-suggests-increase-in-infective-endocarditis-tied-to-reduction-in-antibiotics-use. Accessed December 9, 2015.
- Watters W 3rd, Rethman MP, Hanson NB, et al. Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures. J Am Acad Orthop Surg. 2013;21:180–189.
- American Dental Association. Management of patients with prosthetic joints undergoing dental procedures. Available at: ebd.ada.org/~/media/EBD/ Files/ADA_Chairside_Guide_Prosthetics.ashx. Accessed December 9, 2015.
- American Dental Association. Antibiotic Prophylaxis and Joint Replacement. Mouth Healthy. Available at: mouthhealthy.org/en/az-topics/a/joint-replacement. Accessed December 9, 2015.
- American Dental Association. Infective Endocarditis. Available at: ada.org/~/media/ ADA/Member%20Center/FIles/Infective_Endocarditis_FAQ.ashx. Accessed December 9, 2015.
- Rethman MP, Watters W 3rd, Abt E, et al. The American Academy of Orthopaedic Surgeons and the American Dental Association clinical practice guideline on the prevention of orthopaedic implant infection in patients undergoing dental procedures. J Bone Joint Surg Am. 2013;95:745–747.
- American Dental Association Division of Legal Affairs. An Updated Legal Perspective on Antibiotic Prophylaxis. Available at: jada.ada.org/article/S0002-8177(14)62746-X/fulltext. Accessed December 9, 2015.
- American Dental Association. Toolkit for discussing antibiotics with patients who have orthopaedic implants. Available at: ada.org/en/publications/ada-news/2013-archive/january/toolkit-for discussing-antibiotics-with-patients-who-have-orthopaedic-implants. Accessed December 9, 2015.
From Dimensions of Dental Hygiene. January 2016;14(01):48–51.




[…] to 2013, the ADA and American Academy of Orthopedic Surgeons recommended antibiotic prophylaxis before dental procedures for certain patients with prosthetic joints. The guidelines have since […]