
Caring for Older Adults Residing in Institutions
This vulnerable population is at increased risk for a variety of oral diseases, including caries, periodontal diseases, and fungal infections.
This course was published in the January 2016 issue and expires January 31,2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define residential care facilities (RCF) and the populations they serve.
- Discuss the effects of aging on the oral cavity.
- Identify the most common oral diseases found among older adults living in RCFs.
- List the services that dental hygienists are prepared to provide to an older adult population residing in institutions.
While many older adults are able to remain in their homes, those with extensive health care needs or disabilities may need to move into institutions where they can receive round-the-clock assistance. Residential care facilities (RCFs) are options for individuals who need assistance with dressing, bathing, and medication administration due to physical and mental disabilities. RCF is an umbrella term that comprises assisted living facilities, nursing homes, long-term care facilities, community residences, residential care, enriched housing communities, homes for the aged, shared housing establishments, and personal care facilities. Approximately 90% of those living in RCFs are 65 or older. As of 2010, more than 733,000 individuals were living in 31,100 RCFs across the US.6
ORAL HEALTH STATUS OF INDIVIDUALS LIVING IN RESIDENTAL CARE FACILITIES
Older adults living in RCFs receive help with activities of daily living and medical care, but oral health may be an afterthought. Additionally, professional oral health care services may not be easily accessed in RCFs. The 2004 National Nursing Home Survey noted that 62.5% of RCFs had an arrangement to provide professional oral health care services to their residents—usually through a community-based clinician—but this care was available only on an as-needed basis.7,8 Also, the daily oral hygiene services provided by RCF staff to residents who are unable to perform their own self-care are often provided sporadically and may be of poor quality. A study that looked at the oral health of more than 1,000 individuals living in RCFs in Missouri found that 22% had severe periodontitis (mobile teeth and visible roots) and 35% exhibited dry oral tissues.8,9 Dental hygienists are well positioned to help older adults living in institutions improve their oral health, increase their quality of life, and maintain their systemic health.
EFFECTS OF AGING ON ORAL HEALTH
Age can bring about a multitude of physical and mental changes that may diminish individuals’ ability to care for themselves. Musculoskeletal ailments are common, as is increased risk of fall, unstable gait, arthritis, and vision and hearing loss.10–12 An estimated 42% to 60% of older adults have some sort of musculoskeletal disease.12 These health issues can greatly impact older adults’ mobility. Mental issues, which affect approximately 40% of older adults, also impact older adults’ ability to remain independent.12 Dementia, Alzheimer’s disease, and depression are the most common mental illnesses seen in older adults.10–12 Research indicates about 29% of those living in RCFs experience dementia or Alzheimer’s disease, while about 17% have their mental diseases go undiagnosed.12 Limitations in mobility and cognitive status can significantly hamper older adults’ ability to perform adequate self-care and access professional oral health care services.
The oral cavity also changes with age, regardless of health status. The teeth darken over time, taking on a yellowish hue due to changes in the thickness and composition of the dentin and enamel. As individuals age, the blood flow to the dentition is reduced, so the teeth are not as sensitive to temperature changes. Additionally, the cementum in the teeth begins to thicken while the periodontal ligament shrinks. The tissue in the oral cavity changes with age. It begins to thin, making the floor of the mouth seem more vascular. Finally, the salivary glands tend to react more slowly, so the mucosa may be dry.13
The prevalence of a variety of oral diseases increases with age. Caries (especially root caries), periodontitis, xerostomia, fungal disorders, and dysphagia are often seen in older adults living in RCFs.2,3,10–12 While oral health professionals are well versed in the associations between oral health and systemic health, care providers and staff at RCFs may be unaware of the importance of preventing oral disease and supporting oral health.
DENTAL CARIES
Dental caries is common among older adults living in institutions because they frequently consume a high-carbohydrate diet, often experience diminished salivary flow, have limited self-care ability, and their access to professional oral health care services is reduced. Older adults living in institutions often have large wear facets, furcations, and recession due to the natural aging process.10 These issues often expose the soft dentin of the tooth, increasing susceptibility to caries.2,10,13
Cognitive ability can also impact caries risk. In one longitudinal study, researchers looked at whether older adults with dementia living in RCFs were more likely to develop caries than residents without any cognitive deficits.14 The study took place over 7 years and included 205 elderly residents. Their oral health and decayed, missing, filled teeth (DMFT) scores were recorded. The average DMFT score was a 25.9. Results showed that older adults with dementia experienced more caries lesions than those without dementia, even if the older adults were able to brush their teeth.14
PERIODONTAL DISEASES
Periodontal diseases are common among older adults living in RCFs as their prevalence increases with age.5 Approximately 70% of older adults exhibit some level of periodontitis, with about 64% presenting with moderate to severe forms of chronic periodontitis.5,15
It is well known that the inflammation present in periodontal disease has systemic health effects, as well.11 There may be an association between periodontal bacteria and Alzheimer’s disease. Individuals with Alzheimer’s disease and periodontitis have elevated plasma levels of tumor necrosis factor-alpha.11 Also, older adults living in RCFs with elevated levels of the bacteria Porphyromonas gingivalis have slower cognitive abilities.11 More research is needed to better understand these associations.
Periodontitis is often seen among older adults with diabetes—perhaps, in part, because of relationships between chronic periodontitis and blood glucose levels.10,11 Among those 65 and older, 27% have diabetes.11 Research shows that periodontally involved tissue releases biologically active mediators, bacteria, and bacterial products into the circulation. These products may cause systemic inflammation and activation of monocytes, leading to insulin resistance.11 One meta-analysis showed that routine periodontal treatment reduced HbA1c by 0.8%, but the researchers suggested that more studies were needed to better replicate these results as their sampling of patients may have had limited applicability to the population as a whole.18
FUNGAL INFECTIONS
Many hundreds of different microbial species can populate the oral cavity, including 20 species of Candida, which can cause fungal infections. Older adults who wear dentures have much higher levels of Candida than those with natural dentitions. This may be because edentulous older adults often have other systemic health problems, take multiple medications, and consume limited diets.10,11,19 Candida is associated with several types of pneumonia (Table 2).2,10–12 High blood sugar levels like those seen in individuals with diabetes are yeast friendly, increasing the risk of fungal infection.10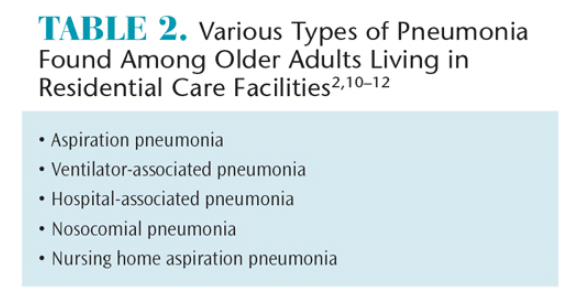
DYSPHAGIA AND XEROSTOMIA
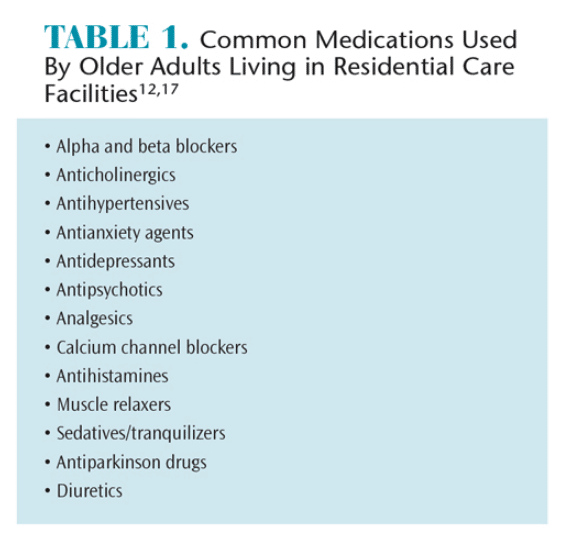
Dysphagia and xerostomia are common among older adults because the salivary glands diminish and the tissue thins with age.2,10,11,13 Additionally, older adults often take medications that may cause xerostomia (Table 1).12,17 On average, older adults take five medications or more each day.17 These medications often induce xerostomia, which may be implicated in dysphagia.2,10
ORAL CANCER
Oral cancer—especially squamous cell carcinoma—is typically found on the lateral border of the tongue, the floor of the mouth, lips, and oropharyngeal area. While tobacco users and heavy drinkers are at the greatest risk for oral cancer, older adults without these risk factors still need to be screened consistently. Oral cancer lesions may be very subtle in their initial presentation, so clinicians need to be vigilant in their evaluations. Older adults with visual and mental deficits may not notice an oral lesion until it’s in the advanced stages, emphasizing the importance of consistent and thorough oral cancer evaluation by oral health professionals.13
THE ROLE OF THE DENTAL HYGIENIST
Dental hygienists are well positioned to serve patients living in RCFs who are at high risk of oral diseases. Dental hygienists can perform routine oral prophylaxes, periodontal assessments, fluoride varnish applications, and oral cancer screenings. Oral hygiene instructions and nutritional counseling may also be provided by dental hygienists. Additionally, dental hygienists are qualified to take impressions for dentures where permitted. Finally, these oral health professionals are well prepared to make appropriate referrals to specialists. Educating RCF staff and residents’ family members is also the purview of dental hygienists. A collaboration between health care professionals working in RCFs, such as geriatric physicians and nurses, and dental hygienists will help improve residents’ oral and systemic health.
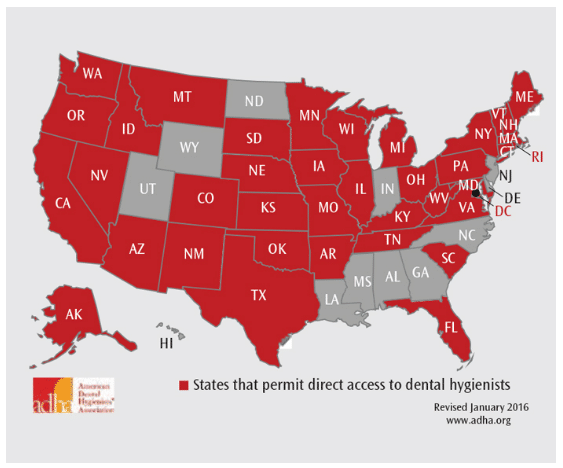
Dental hygienists who wish to work in RCFs need to live in states that allow this within the scope of practice. Currently, 38 states allow dental hygienists direct access to patients (Figure 1).21,22 According to the American Dental Hygienists’ Association, direct access is an arrangement that “allows dental hygienists the right to initiate treatment based on their assessment of a patient’s needs without the specific authorization of a dentist, treat the patient without the presence of a dentist, and maintain a provider-patient relationship.”23 Changes to state dental practice acts may be on the horizon, easing the ability of dental hygienists to reach this vulnerable population.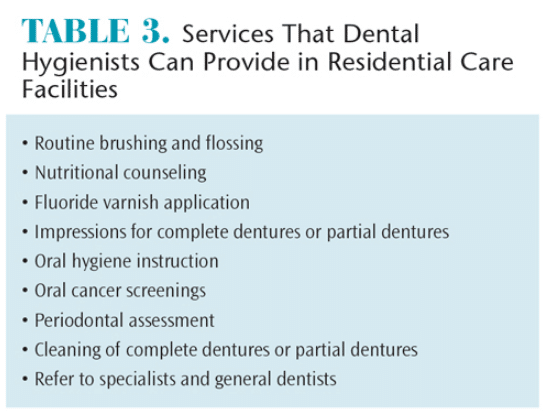
CONCLUSION
Older adults living in RCFs are dependent on others to provide the care they need to maintain their oral and general health. As these facilities become more crowded due to the growing numbers of older adults, this population will be dependent on health professionals for help. Dental hygienists can educate RCF staff, patients, caregivers, family members, and the general public about the relationship between systemic conditions and poor oral health commonly seen in elderly patients. As versatile health care providers, dental hygienists have much to offer this population (Table 3). As more opportunities for clinicians become available in this setting, the oral health of older adults living in RCFs will likely improve.
References
- The American Geriatrics Society. The demand for geriatric care and evident shortage of geriatrics health care providers. Available at: americangeriatrics.org/files/documents/Adv_Resources/demand_for_ geriatric_care.pdf. Accessed December 18, 2015.
- Moore L. Dental health and aging: the connection to overall health. Society of Certified Senior Advisors. 2013;57:10–13.
- The State of Aging and Health in America 2013. Atlanta: Centers for Disease Control and Prevention, United States Department of Health and Human Services; 2013.
- Slade GD, Akinkugbe AA, Sanders AE. Projections of US edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93:959–965.
- Prakasam S. Periodontal care for older adults. Dimensions of Dental Hygiene. 2015;13(7):45–50.
- National Center for Assisted Living. Assisted Living State Regulatory Review. 2013. Available at: ahcancal.org/ncal/resources/Documents/2013_reg_review.pdf. Accessed December 18, 2015.
- Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat 13. 2009;167:1–155.
- Branson B, Simmer-Beck M. Addressing the oral health needs of long-term care facility residents. Dimensions of Dental Hygiene. 2013;11(8):31–35.
- Missouri Department of Health and Senior Services. Adult Oral Health Assessment Executive Summary. Available at: health. mo. gov/ living/ families/ oralhealth/ pdf/ Adult_ Oral_ Health_ Assessment_Executive_Summary.pdf. Accessed December 18, 2015.
- Dahm T, Bruhn A, Lemaster M. Oral care in the long-term care of older patients: How can the dental hygienist meet the need? J Dent Hyg. 2015;89:269–277.
- Berkey DB, Scannapieco FA. Medical considerations relating to the oral health of older adults. Spec Care Dentist. 2013;33: 164–176.
- Qiu WQ, Dean M, Liu T, et al. Physical and mental health of the homebound elderly: an overlooked population. J Am Geriatr Soc. 2010;58:2423–2428.
- Gonsalves WC, Wrightson AS, Henry RG. Common oral conditions in older people. Am Fam Physician. 2008;78:845–852.
- Philip P, Rogers C, Kruger E, et al. Caries experience of institutionalized elderly and its association with dementia and functional status. Int J Dent Hygiene. 2012;10:122–127.
- Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914–920.
- Humphrey SP, Williamson RT. A review of saliva: normal composition, flow, and function. J Prosthet Dent. 2001;85:162–169.
- Wilson IR, Schoen C, Neuman P, et al. Physician patient communication about prescription medication nonadherence: A 50 state study of America’s seniors. J Gen Intern Med. 2007;22:6–12.
- Darre L, Vergnes JN, Gourdy P, et al. Efficacy of periodontal treatment on glycaemic control in diabetic patients: a meta-analysis of interventional studies. Diabetes Metabol. 2008;34:497–506.
- Mizugai H, Isogai E. Hirosc K, et al. Effect of denture wearing on occurrence of Candida species in the oral cavity. J Appl Res. 2007;7:250–254.
- Zenthofer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly—a RCT. Community Dent Oral Epidemiol. 2013;41:261–268.
- American Dental Hygienists’ Association. Facts About the Dental Hygiene Workforce in the United States. Available at: adha.org/resources-docs/75118_Facts_About_the_Dental_Hygiene_Workforce.pdf. Accessed December 18, 2015.
- American Dental Hygienists’ Association. Direct Access Map. Available at:?adha.org/resources-docs/7524_Current_Direct_Access_Map.pdf. Accessed December 18, 2015.
- American Dental Hygienists’ Association. Direct Access. Available at: adha.org/direct-access. Accessed December 18, 2015.
From Dimensions of Dental Hygiene. January 2016;14(01):52–55.



