 Computer illustration of Zika virus particles SELVANEGRA / ISTOCK / THINKSTOCK
Computer illustration of Zika virus particles SELVANEGRA / ISTOCK / THINKSTOCK
Preparing for the Zika Virus
Oral health professionals need to remain up to date on this viral epidemic so they can best protect themselves and their patients.
This course was published in the June 2016 issue and expires June 30, 2019. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the history of the Zika virus.
- Identify the signs and symptoms of Zika virus, as well as resultant complications.
- Explain how the Zika virus is transmitted.
- Discuss the prevention of Zika infection in the dental setting.
Since the beginning of the current Zika epidemic in May 2015, more than 500 cases of Zika virus infection have been diagnosed in the United States.1 Most of the infections occurred in Florida, New York, California, and Texas, but almost all other states and the District of Columbia have reported cases. Additionally, more than 800 cases of locally-acquired Zika virus infection have been reported in US territories, such as Puerto Rico, US Virgin Islands, and American Samoa. Confirmed reports of sexual transmission of the virus, infections in pregnant women, and several cases of Guillain-Barré syndrome have also been documented in the US and US territories. All of the cases reported in the US were travel-associated, prompting the US Centers for Disease Control and Prevention (CDC) to issue a “travel alert level 2,” which recommends practicing enhanced precautions while traveling to countries and territories affected by the Zika virus.2
Due to the fast spread of travel-related Zika virus infection and in anticipation of large and active mosquito populations in the continental US, especially in southern states, the Obama administration asked Congress for $1.9 billion in emergency funding to build preparedness aimed at better preventing and managing this disease.3 Table 1 lists the goals of this emergency funding. At press time, the Senate had approved $1.1 billion in emergency funding to address the Zika epidemic, while the House introduced a bill that would supply $262 million to fight the virus through the end of September.
The government’s concerns are justified. The current Zika epidemic began in Brazil in May 2015 and quickly spread across Latin America.1,4 Of the 9.9 million travelers who departed Brazil from airports located in areas conducive to year-round Zika viral transmission, 65% flew to the North America and more than 2.7 million arrived in the US.4 Adding to the travel-associated spread of disease, more than 60% of Americans reside in areas conducive to seasonal Zika transmission, while 22.7 million people in the US live in areas where year-round transmission is possible.4
Dental hygienists are well positioned to recognize the signs and symptoms of Zika virus infection in patients. State and local health departments, such as the New York State Department of Health, have responded to the threat by developing guidelines for Zika detection and testing for health care professionals and setting up Zika information hotlines for the general public.5 However, there are no guidelines specific to oral health care providers regarding identifying patients with signs of disease, referral for diagnosis and testing, or methods of prevention in the dental setting. As clinicians and educators, dental hygienists need to understand this emerging threat and be able to provide information and resources to patients who may be concerned about Zika virus infection.
This article will discuss the signs and symptoms of Zika virus infection, modes of transmission, association of Zika virus with microcephaly and other negative pregnancy outcomes, methods of preventing viral transmission in dental settings, and recommendations to health care providers by professional organizations and government agencies.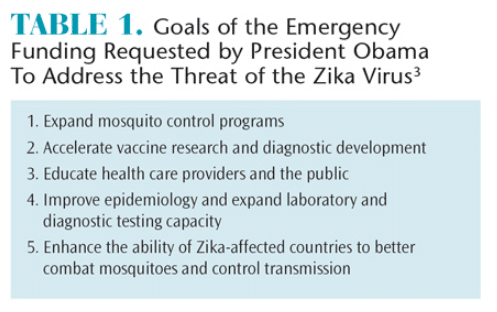
THE VIRUS AND ITS HISTORY
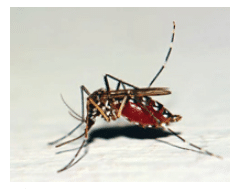
The Zika virus is a member of the Flaviviridae family. It is an arbovirus—one of the hundreds of RNA viruses transmitted by arthropods such as mosquitoes and ticks.6 Chikungunya, dengue, and West Nile viruses are also in this category. The Zika virus originated in the Zika forest in Uganda and was first isolated from a rhesus monkey in 1947. Only sporadic human cases of disease were reported until outbreaks occurred on Micronesia’s Yap Island in 2007 and in French Polynesia in 2013.6 Similar to most arboviruses, Zika is transmitted to humans through the bite of infected Aedes mosquitoes, specifically Aedes aegypti. This species lives predominantly in equatorial climates, although there is a possibility that the virus may adapt to transmission by the more widely distributed mosquito A. albopictus found in at least 32 US states.6
The current epidemic began in Brazil in May 2015 and quickly spread to Central America, Pacific Islands, Mexico, and the Caribbean.1,2
SELVANEGRA / ISTOCK / THINKSTOCK
SIGNS, SYMPTOMS, AND COMPLICATIONS
Zika is characterized as an asymptomatic or mild dengue-like disease with fever, muscle and joint aches, conjunctivitis, and maculopapular rash with an incubation period of 3 days to 12 days.5,7 Only about 20% of cases are symptomatic.7 There is no specific anti-viral treatment; management of symptoms may include the use of analgesics and antipyretics. Nonsteroidal anti-inflammatory drugs and aspirin should not be used due to a heightened risk of hemorrhage, at least until dengue is ruled out. Acetaminophen is recommended as an alternative.7,8 However, in more than 60 years of observation, the Zika virus has not been reported to cause hemorrhagic fever or death.6 Guillain-Barré syndrome or other neurologic conditions are potential complications. Such complications were diagnosed in 73 cases in French Polynesia.6,7,9
The most significant public health concern is the recently confirmed association between Zika infection during pregnancy and microcephaly or other severe fetal brain defects.10 The relationship between Zika infection and microcephaly has long been suspected based on detection of Zika viral RNA in mothers and amniotic fluid samples from fetuses, which demonstrates Zika virus’ potential to infect fetuses (Figure 1).6,8,10–12 An otherwise unexplained 20-fold increase in the incidence of microcephaly in Brazil occurred between 2014 and 2015, which prompted health authorities in the affected regions to develop recommendations for pregnant women.6 In the US, interim guidelines developed by the CDC include recommendations for travel, screening, testing, and management of returning travelers who are pregnant.8
Links between Zika infection and microcephaly and the precise cellular mechanisms of damage to neural cells are under investigation. Incomplete viral autophagy, centrosome abnormalities, and chromosomal instability have been observed in Zika-infected cells.11 Notably, no other flavivirus has been associated with teratogenic effects.6
IMNATURE / ISTOCK / THINKSTOCK
TRANSMISSION
The Zika virus is transmitted by Aedes mosquitoes, primarily A. aegypti (Figure 2). Experimental infections confirmed that this species is capable of transmitting Zika. Because A. aegypti mosquitoes bite during the day,1,13 mosquito nets are less effective in preventing Zika infection, although parents are encouraged to cover baby strollers, cribs, and baby carriers for daytime protection.13
Additional modes of transmission include perinatal transmission that can occur by transplacental transmission or during delivery by an infected mother.12 Zika viral RNA was also detected in breast milk, raising the concern of potential transmission by breastfeeding.12 Sexual transmission was reported in a few instances and replicative Zika viral particles were isolated in the semen of a patient who had a confirmed Zika infection a few weeks prior to developing hematospermia.14 The same patient had Zika viral RNA detected in his urine, which offers testing possibilities after early viremia is over.14
A potential risk of Zika virus transmission during a blood transfusion has been reported.15 Zika viral RNA was detected in blood samples from asymptomatic donors and the number of positive results was unexpectedly high (3%), although no post-transfusion infection has been reported in recipients of Zika virus-positive blood.15 However, on February 16, 2016, the US Food and Drug Administration (FDA) recommended the deferral of individuals from donating blood if they have traveled to areas with active Zika virus transmission, were potentially exposed to the virus, or have experienced a confirmed Zika virus infection.16
ZIKA VIRUS IN SALIVA
Zika virus RNA has been found in saliva during the acute phase of disease, although it is not yet known if the virus can be transmitted by saliva.17 It was found that the ability to detect the virus in saliva was greater than in blood.17 Both techniques could be used to facilitate diagnoses in young children or neonates, in remote regions with no testing facilities, or in community settings for routine surveillance.17 Dental offices and clinics may be appropriate venues for performing salivary diagnostics with dental hygienists performing these tests.
While there is no evidence that Zika infection can be spread via saliva, the presence of Zika viral RNA in saliva raises concerns. This is especially true in dental settings, where contact with saliva is frequent and where droplets and aerosols are often created during instrumentation.
PREVENTING ZIKA INFECTION IN THE DENTAL SETTING
In 1996, the CDC developed standard precautions to prevent the transmission of pathogens through blood and other potentially infectious materials. Recommended infection control practices for dentistry were provided in 2003 and recently updated.18 Standard precautions are designed to protect health care providers, including dentists, dental hygienists, and auxiliary dental professionals, from exposure to these pathogens. Although the effort to prevent transmission in the dental office has primarily focused on bloodborne pathogens, saliva is also a potential route of transmission for many pathogens. Infection control protocols are determined by the clinical procedures performed, not the patient’s health status. As such, all patients must be treated as if they are potentially infectious.
The primary methods of reducing transmission risk in the dental office combine standard precautions with performance-based standards. Hand hygiene, the use of personal protective equipment (PPE), reducing the risk of cross-contamination, incorporating both work practices and engineering controls, respiratory/cough etiquette, and safe injection practices comprise the backbone of the CDC’s recommendations.18
The second tier of infection control—transmission-based precautions—may be necessary when patients have a documented infection, may have been exposed to a highly transferrable pathogen, and when standard precautions may be insufficient to prevent disease transmission via airborne, droplet, or dry skin contact.19 Transmission-based precautions are specific to anticipated contact routes and are, by definition, limited in duration—typically to the contagious period of the disease in question.19 Enhanced precautions in the dental setting were implemented in 2009 during an H1N1 influenza pandemic. The CDC recommendations included rescheduling symptomatic patients’ nonurgent dental treatment, waiting 24 hours to treat such patients after fever had subsided, using respiratory/cough etiquette protocols, wearing appropriate PPE, and providing care—when urgent—with operatory doors closed.20
While the Zika virus has been detected in a number of body fluids, including blood and saliva, there are no reports of transmission from infected patients to health care providers.21 At this time, the CDC recommends all health care personnel practice standard precautions. The use of transmission-based precautions has not been recommended, even in instances when there is a potential for exposure to large volumes of blood, such as during labor and delivery.21
Patients will most likely delay seeking routine dental and dental hygiene treatment during acute illnesses. However, only one out of five patients with Zika virus infection will be symptomatic and those symptoms can be mild.7,9 It may be prudent to postpone nonurgent dental and dental hygiene treatment for patients with active Zika virus infection.
Vaccinations against communicable diseases may offer at least some protection for health care personnel, but there is no vaccine against Zika infection.9 Although the National Institutes of Health launched a Zika immunization initiative in late 2015, a safe and effective vaccine is likely years away, despite efforts to accelerate research and development.9
CONCLUSION
Much remains unknown about the Zika virus, the infection it can cause, and its consequences. Following the principle that prevention is better than cure, dental professionals must be prepared to manage the risks, recognize the signs and symptoms of illness, collect and analyze thorough medical and potential exposure histories, assess the possibility for transmission, and provide timely referrals for evaluation and treatment. Consistent adherence to standard precautions by every dental care team member is crucial. The effectiveness of infection-control programs should be continually evaluated to help ensure that policies, procedures, and practices are effective in preventing infection transmission in dental settings.
Because typical clinical manifestations of the symptomatic Zika virus disease are nonspecific, its differential diagnosis is broad. However, health care providers are encouraged to report suspected cases to their state or local health departments to facilitate diagnosis and reduce the possibility of local transmission.7 For example, in New York, laboratory diagnostic testing is available at the Department of Health’s Wadsworth Laboratories, one of only a few state public health laboratories that can test for Zika virus outside of the CDC.5
Dental professionals must also be able to dispel misinformation about the Zika virus and the illnesses it can cause by providing up to date, evidence-based information to patients. Dental professionals and patients appear to be adequately protected by the use of established standard infection control protocols. Dental hygienists, as oral heath educators, should keep abreast of any emerging epidemic or pandemic, including Zika. Some warn that climate changes, urbanization, population growth, and international travel may put increasing numbers at risk of disease like the Zika virus.22 Thus, health care providers must remain aware of emergent diseases and be ready to limit the spread of infection.
The CDC website is an excellent resource for the most current information about the Zika epidemic: cdc.gov/zika/index.html. Current information on infection control practices can be found at the Organization for Safety, Asepsis, and Prevention’s website: osap.org/?page=Issues_ZikaVirus
References
- Centers for Disease Control and Prevention. Zika Virus Disease in the United States, 2015–2016. Available at: cdc.gov/zika/geo/united-states.html. Accessed May 18, 2016.
- Centers for Disease Control and Prevention. Travel Health Notices Available at:?nc.cdc.gov/travel/notices. Accessed May 18, 2016
- The White House. Letter From the President—Zika Virus. Available at:?whitehouse.gov/the-press-office/2016/02/22/letter-president-zika-virus. Accessed May 18, 2016.
- Bogoch II, Brady OJ, Kraemer MU, et al. Anticipating the international spread of Zika virus from Brazil. Lancet. 2016;387:335–336.
- New York State Department of Health. Zika Virus. Available at: health.ny.gov/diseases/zika_virus. Accessed May 18, 2016.
- Fauci AS, Morens DM. Zika virus in the Americas—yet another arbovirus threat. N Engl J Med. 2016;387:601–604.
- Centers for Disease Control and Prevention. Zika Virus. Clinical Evaluation and Disease. Available at: cdc.gov/zika/hc-providers/clinicalevaluation.html. Accessed May 18, 2016.
- Petersen EE, Staples JE, Meaney-Delman D, et al. Interim guidelines for pregnant women during a Zika virus outbreak—United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:30–33.
- Lucey DR, Gostin LO. The emerging Zika pandemic: enhancing preparedness. JAMA. 2016;315:865–866.
- Centers for Disease Control and Prevention. CDC Concludes Zika Causes Microcephaly and Other Birth Defects. Available at:?cdc.gov/media/releases/2016/s0413-zika-microcephaly.html. Accessed May 18, 2016.
- Tetro JA. Zika and microcephaly: causation, correlation, or coincidence? Microbes Infect. 2016;18:167–168.
- Besnard M, Lastère S, Teissier A, Cao-Lormeau V, Musso D. Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill. 20143;19:20751.
- European Centre on Disease Prevention and Control. Zika Virus Infection: Fact Sheet for Health Professionals. Available at:?ecdc.europa.eu/en/healthtopics/zika_virus_infection/factsheet-health-professionals/Pages/factsheet_health_professionals.aspx. Accessed May 18, 2016.
- Musso D, Roche C, Robin E, Nhan T, Teissier A, Cao-Lormeau VM. Potential sexual transmission of Zika virus. Emerg Infect Dis. 2015;21:359–361.
- Musso D, Nhan T, Robin E, et al. Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill. 2014;19:1–3.
- Food and Drug Administration. FDA Issues Recommendations to Reduce the Risk for Zika Virus Blood Transmission in the United States. Available at:?fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm486359.htm. Accessed May 18, 2016.
- Musso D, Roche C, Nhan TX, Robin E, Teissier A, Cao-Lormeau VM. Detection of Zika virus in saliva. J Clin Virol. 2015;68:53–55.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for Infection Control in Dental Health-Care Settings, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(RR–17):1–61.
- Harte JA. Standard and transmission-based precautions: an update for dentistry. J Am Dent Assoc. 2010;141:572–581.
- Centers for Disease Control and Prevention. Prevention of 2009 H1N1 influenza transmission in dental health care settings. Available at: cdc.gov/OralHealth/infectioncontrol/factsheets/2009_h1n1. htm. Accessed May 18, 2016
- Olson CK, Iwamoto M, Perkins KM, et al. Preventing transmission of Zika virus in labor and delivery settings through implementation of standard precautions— United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:290–292.
- Gillis J. In Zika epidemic, a warning on climate change. New York Times. February 20, 2016.
From Dimensions of Dental Hygiene. June 2016;14(06):48–51.



