Diagnosis and Treatment of Internal Resorption
Early detection and treatment of this oral condition can help maintain the functionality of the tooth.
Tooth resorption is defined as a physiologic or pathologic process that results in the loss of dental tissue, such as dentin and cementum.1 Tooth resorption is classified as either internal or external, which can be further divided into specific types. Internal resorption originates from within the pulp, while external resorption begins in the periodontal ligament. Although external resorption is more common, it is often misdiagnosed as internal resorption.
An inflammatory process occurring within the pulp tissue, internal resorption ultimately leads to dentin loss.1 While the exact process is not fully understood, two histological characteristics are common. First, multinucleated giant cells (dentinoclasts, which are virtually identical to osteoclasts) are observed in granulation (ie, inflammatory) tissue in the pulp. Second, predentin and odontoblasts in the area of resorption are absent.2,3 Theories regarding etiology include trauma or pulpal damage that occurs during the preparation of a tooth for a restorative procedure.4 The dentinoclasts dissolve the dentin concentrically by producing an acidic environment. This leads to internal resorption’s characteristic radiographic appearance of a circular radiolucency continuous with the pulp canal space.
The diagnosis of internal resorption is made through a combination of clinical and radiographic findings. For internal resorption to occur, some vital pulp tissue must be present. Pulp test (electric, cold, heat) results are suggestive of tooth vitality. It is possible to obtain a negative result, however, if coronal pulp tissue is necrotic despite the apical pulp tissue remaining vital. Patients typically present with no pain and are asymptomatic.5 Internal resorption is typically detected during recare or routine radiographic examinations. However, a tooth experiencing internal resorption may appear slightly pink due to an enlarged pulp. This is called the “pink tooth of Mummery,” after an anatomist. The condition was once considered indicative of internal resorption, but it can also be seen in some forms of external resorption.
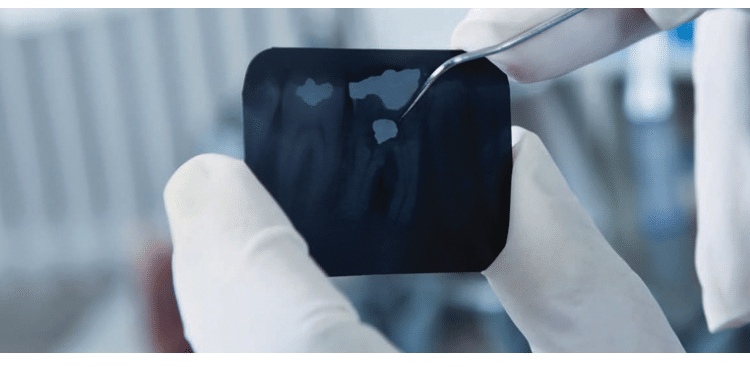
RADIOGRAPHIC DIAGNOSTICS
Radiographically, a uniform, semicircular radiolucent area contiguous with the pulp is a sign of internal resorption (Figure 1). In order to distinguish this from external resorption that may be on the facial or lingual surface of the root, an additional, angulated radiograph (shift-shot X-ray) can be helpful. This radiograph is exposed using exaggerated horizontal angulation of approximately 20° to 30° to the mesial or distal. If the radiolucent area remains over the canal space, internal resorption is likely. Conversely, if the radiolucent area appears to move away from the pulp, it is probably external resorption.

COURTESY FRANK GRAZIANO, DDS
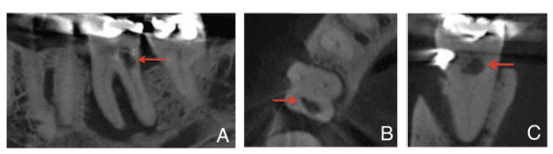
If two-dimensional radiography is not determinative, three-dimensional (3D) imaging can be useful. Cone-beam computed tomography (CBCT) uses a conically shaped exposure to create cross-sectional slices used to produce imagery made up of 3D voxels.6 Voxels permit the image to be viewed from different angles: axially (inferior–superior axis), coronally (anterior–posterior axis), and sagittally (mesial-distal axis).
Because endodontic procedures are usually concerned with a small area, or single tooth, it is best to use a limited field of view (FOV), as opposed to the larger FOVs used in other dental disciplines. A limited FOV yields several benefits–most important being that it increases image resolution, while at the same time administering a lower dose of ionizing radiation to the patient. For endodontic purposes, a resolution with a voxel size of 75 ?m to 125 ?m is appropriate.6,7 The effective radiation dose depends on the actual cone-beam device and the area being scanned. The dose can range from 5 ?Sv to 191 ?Sv. For comparison, a typical digital periapical radiograph exposes the patient to 6 ?Sv. Scans of the maxillary anterior require the least amount of ionizing radiation while the mandibular posterior region requires the most.8
The use of CBCT technology can provide great detail. In cases of internal resorption, the exact location and extent of the defect can be visualized (Figures 2A through 2C). Such information may help develop a better treatment plan with an improved prognosis compared with the use of traditional imaging.9 This leaves clinicians with the question of when CBCT should be used to supplement traditional radiography. This question remains contentious because the “as low as reasonably achievable” (ALARA) radiographic dosing principle should be observed. Thus, CBCT technology needs to be used judiciously–perhaps only when a definitive diagnosis or developing a quality treatment plan is challenging.
CLINICAL TREATMENT
Treatment for internal resorption includes root canal therapy, followed by restoration. Considering that vital pulp tissue is necessary for resorption, root canal therapy will stop the resorption.5 The chemical cleaning aspect of root canal therapy typically involves using various concentrations of sodium hypochlorite. This dissolves both necrotic and vital pulp tissue and disinfects root canals. Clinicians may also place calcium hydroxide as an intracanal medicament between root canal appointments if a multi-appointment approach is favored. This will help to dissolve any remaining granulation tissue prior to the completion of intraradicular treatment, followed by canal obturation with gutta-percha.
One aspect to consider during treatment planning is the size of the defect. Although root canal treatment will halt the internal resorptive process, if the defect is large, the tooth may be prone to fracture during function. It is best to detect such a circumstance early, so proper treatment can be initiated.
In summary, internal resorption is the loss of dentin contiguous to the pulp, and is mediated by multinucleated giant cells called dentinoclasts. Patients are usually asymptomatic, so an accurate diagnosis depends on a thorough radiographic examination, along with clinical observations and testing. If detected early when sufficient root structure remains, root canal treatment, followed by a restoration, can help maintain the tooth.
References
- American Association of Endodontists. AAE Glossary of Endodontic Terms. Available at: aae.org/clinical-resources/aae-glossary-of-endodontic-terms.aspx. Accessed May 10, 2016.
- Tronstad L. Root resorption–etiology, terminology and clinical manifestations. Endod Dent Traumatol. 1988;4:241–252.
- Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth–the development of pulp necrosis. Endod Dent Traumatol. 1985;1:207–220.
- Hargreaves KM, Cohen S. Cohen’s Pathways of the Pulp. 10th ed. St. Louis:Mosby; 2010.
- Ingle JI, Barkland LK, Baumgartner JC. Ingle’s Endodontics. 6th ed. Hamilton, Ontario, Canada: BC Decker; 2008.
- Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007;33:1121–1132.
- Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone-beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40:818–830.
- Ludlow JB, Timothy R, Walker C, et al. Effective dose of dental CBCT–a meta-analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 2015;44:20140197.
- Khojastepour L, Moazami F, Babaei M, Forghani M. Assessment of root perforation within simulated internal resorption cavities using cone-beam computed tomography. J Endod. 2015;41:1520–1523.leventince/istock/thinkstock
From Dimensions of Dental Hygiene. June 2016;14(06):46–47.

