 ALEX-MIT/ISTOCK/GETTY IMAGES PLUS
ALEX-MIT/ISTOCK/GETTY IMAGES PLUS
Occlusal Trauma and Periodontal Diseases
The implications of occlusal trauma should be part of a comprehensive periodontal examination.
This course was published in the August 2021 issue and expires August 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the relationship between occlusal trauma and periodontal diseases.
- Discuss the presentation of occlusal discrepancies.
- Explain how to perform a chairside occlusal assessment.
- Describe the therapies used to treat occlusal discrepancies.
According to the United States Centers for Disease Control and Prevention, nearly half of adults older than 30 have some form of periodontal disease.1 Diagnosis, treatment, and management of periodontal diseases are especially beneficial during their early stages when maintaining a healthy periodontium is achievable. Identifying occlusal trauma in the earlier stages of periodontitis is key to helping reduce the potential effects of inflammatory responses and excessive occlusal forces on the supporting bone around teeth.2,3 Oral health professionals, however, often overlook occlusal discrepancies that can lead to trauma as part of their overall periodontal assessment.4 It should become standard practice for clinicians to document and consider the implications of occlusal trauma as part of the comprehensive periodontal examination and incorporate routine occlusal evaluations.2,5
A cause and effect relationship between occlusal trauma and periodontal diseases has yet to be established. Ethical considerations confine research to retrospective and empirical trials rather than the prospective and longitudinal studies necessary for determining occlusion and periodontal correlation.6–8 Present theories suggest that by injuring gingival and periodontal fibers and enhancing tissue permeability, occlusal trauma serves as an aggravating factor or modifier of periodontal diseases.2,6
Periodontal pathogens are etiological causes for periodontal inflammatory responses.3,9 The potential risk for increased bone loss and pocket depth occurs when active periodontal infection and traumatic occlusion are present at the same time. Passanezi and Sant’Ana2 examined whether occlusal discrepancies played a role in the progression of periodontal diseases. They found that people with periodontitis and occlusal discrepancies who did not undergo occlusal therapy developed a significant and rapid increase in probing depths compared to those with periodontitis and occlusal discrepancies who underwent corrective occlusal treatment in conjunction with periodontal therapy. These results suggest that the assessment and documentation of occlusal discrepancies when performing a comprehensive periodontal examination are helpful.
Malocclusions and Occlusal Trauma
Dental occlusion refers to the relationship between maxillary and mandibular teeth when in contact with each other.2 Occlusal trauma, like periodontal diseases, is multifactorial.10 Normal occlusion helps to prevent disease, and is not only esthetically appealing but also supports proper oral functions such as mastication, speech, and balance of periodontal structures. Malocclusion occurs when teeth do not come together in normal occlusion, and is considered any deviation from the anatomically acceptable relationship of the maxillary and mandibular arch/teeth.2 In a random sample analysis to determine the prevalence of malocclusion among US adults, Asiri et al11 concluded that of the 8,804 examined, nearly 66% had at least one or more forms of malocclusion.
Contact discrepancies in the maxillary and mandibular arches are affected by the dentition’s interrelational contacts. Functional contacts refer to the harmonious relationship between the maxillary and mandibular teeth during mastication and swallowing.3 Parafunctional contacts are those produced outside of the normal range of function and can negatively impact the supporting periodontal structures.2,3,7 Parafunctional contacts can occur from oral habits or occlusal neuroses such as clenching, bruxism, and biting of nails, lips, or hard objects. Tooth extractions or pathological tooth migration may also result in parafunctional contacts.3,12
Occlusal trauma refers to injury resulting in tissue changes within the attachment apparatus, including periodontal ligament, supporting alveolar bone, and cementum.7,13 Primary occlusal trauma is caused by excessive occlusal forces applied to a tooth/teeth with a normal periodontium, and most commonly occurs following a newly inserted restoration with an altered contact point. Secondary occlusal trauma occurs when excessive or normal occlusal forces are applied to a tooth with reduced periodontal/bone support or when the tooth’s ability to absorb stress is impaired.3,7 This is more common in patients with mild to advanced periodontal diseases. In cases of secondary occlusal trauma, periodontal therapy to manage inflammatory responses should be first, followed by occlusal therapy to reduce forces that further injure the periodontium.
Chairside Occlusal Assessment
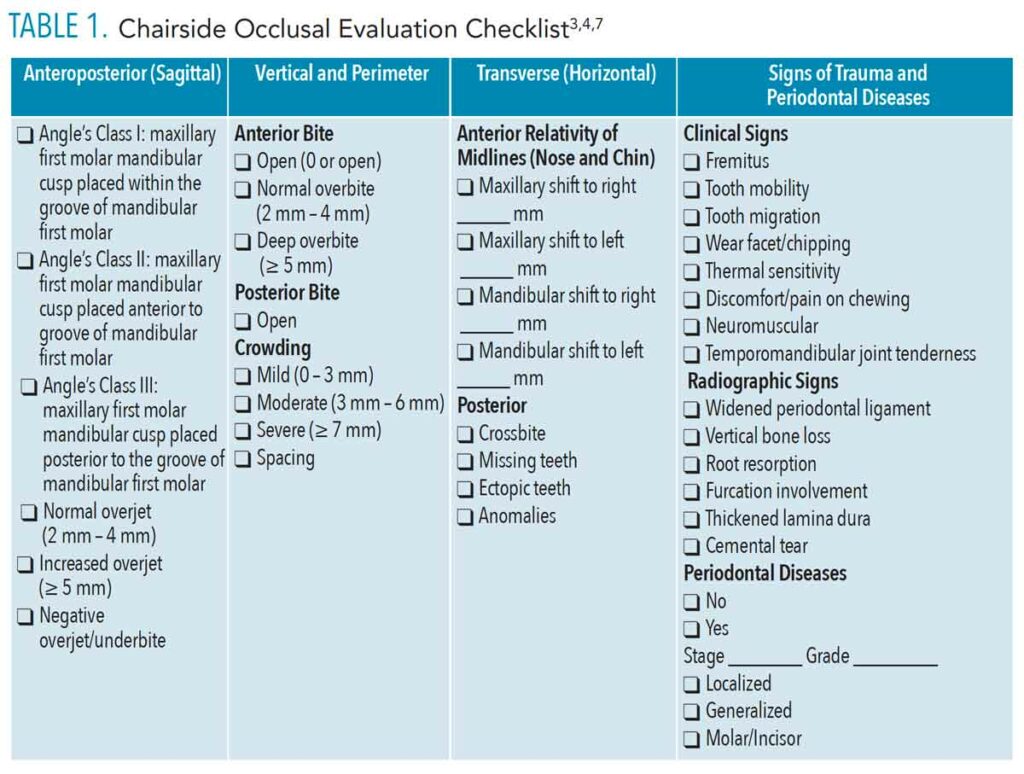
An occlusal evaluation of the four planes—anteroposterior, vertical, transverse, and perimeter—encompasses a comprehensive exam and identifies the need for referrals sooner.4 It begins with observing the patient’s face and dentition from the right and left profile. Positioning of the anteroposterior or sagittal plane determines the Angle’s classification of occlusion, which is used to identify the corresponding contact relationship between the maxillary and mandibular first molars. The contact relationship of the maxillary mesiobuccal cusp of the maxillary first permanent molar with the mandibular buccal groove of the mandibular first permanent molar is categorized as Class I occlusion and is considered ideal.2,3 Class II and III are noted as malocclusion, posing a greater risk for occlusal trauma. Class II occurs when the mesiobuccal cusp of the maxillary first molar is mesial to the buccal groove of the mandibular first molar. Class III happens when the mesiobuccal cusp of the maxillary first molar is distal to the buccal groove of the mandibular first molar. When the permanent first molars are missing, the canine relationship is used to identify occlusion.2,3
Determining the centric relation and maximum intercuspation, formerly known as centric occlusion, is an integral part of the occlusal assessment. Centric relation is the association of the mandible at the most relaxed and retruded anatomical position to the maxilla. In contrast, the condyle disk relation is balanced, and lateral movements can occur regardless of vertical space or tooth position.2,14 Tooth location and occlusion do not influence centric relation because it is solely a joint position. Maximum intercuspation refers to the relationship of the maxillary and mandibular teeth in maximum intercuspation.2,14 To achieve occlusal harmony, the maximum intercuspation needs to coincide with centric relation, so the teeth fully interconnect as the condyles are positioned in the joint space with the disk properly in place.14
Canine Guidance and Interference
Assessing a patient’s canine guidance during the occlusal evaluation will determine potential parafunctional activity when teeth come into contact. Canine guidance refers to the disocclusion of all other teeth by the canines when the jaw slides laterally from side to side. In other words, as the jaw slides laterally, the posterior teeth should not come into contact. If they do, it is considered an interference. When the posterior teeth come into contact, the muscles of mastication are actively engaged, significantly increasing the occlusal load.14 Conversely, as the canines come into contact during lateral motions, the muscles of mastication remain relaxed, and occlusal forces are minimal. If interference occurs during lateral jaw movements, chances are parafunctional contacts are causing abnormal occlusal wear patterns (facets), and occlusal therapy may be warranted.
Wear facets, which present as flat spots on the occlusal surfaces of teeth, are clinical manifestations of parafunctional activity. Apparent wear facets with a glassy surface typically indicate the patient is currently bruxing, while those with a dull surface indicate the patient was a bruxer in the past or bruxes sporadically.8
Clinicians can educate patients on the development of wear facets and assist them in making informed decisions about corrective treatment.14 Clinicians can also use emerging technologies, such as scanners, to assess and measure occlusal clearances, visualize the contact interaction between arches, locate abnormal occlusal stresses, and detect tooth wear or fractures (Table 1, page 33).3,4,7
Manifestations of Occlusal Trauma
Occlusal injury exhibits distinct manifestations of stress and pressure within the surrounding periodontium.6,7,9 Lesions that develop from excessive forces differ in location and severity depending on the degree and position of the forces applied.6,9 Radiographic signs of a periodontium impacted by traumatic occlusal forces may show a widening of the periodontal ligaments, thickened lamina dura, root resorption, furcation involvement, cemental tear, and localized vertical bone loss. When the cementoenamel junction (CEJ) between adjacent teeth is not evenly aligned, the bone slants vertically toward the CEJ with the greatest vertical depth. Misaligned teeth can cause a discrepancy between the proximal CEJs, leading to vertical bone loss with an intact lamina dura. When bone loss forms vertically and the white lining of the lamina dura is no longer visible on a radiograph, it may indicate that a vertical defect has developed from a combination of inflammatory factors and traumatic occlusal forces. When inflammation is the only destructive factor of bone loss, however, it typically presents as horizontal.3 Clinical manifestations of occlusal trauma may present as fractured incisal/occlusal surfaces, wear facets, temporomandibular joint tenderness, neuromuscular disturbances, tooth migration, sensitivity to pressure or temperature, tooth mobility, or fremitus.3,7
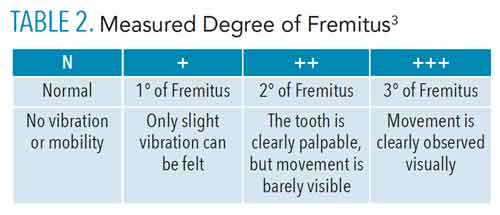
Fremitus is an indicator of excessive occlusal forces when teeth prematurely come into occlusal contact. Wilkins et al3 refer to fremitus as “the vibratory patterns of the teeth” exhibiting as “palpable vibration or movement” when excessive tooth contact is present. In tooth fremitus, tooth movements can be slight and may only occur upon excess occlusal contact. As fremitus occurs due to excessive tooth contact, a determination is measured using the maxillary teeth only.9
A clinician can check for fremitus by seating the patient upright with the head stabilized against the headrest and the occlusal plane parallel to the floor. He or she then places an index finger on each maxillary tooth at the cervical third. The patient is instructed to close the posterior teeth together in functional occlusion and tap up and down repeatedly. The vibration is recorded by the clinician as he or she moves his or her index finger to each tooth across the arch, beginning with the most posterior tooth (Table 2).3
Occlusal Therapies
Occlusal therapy may slow disease progression and improve the prognosis of periodontal diseases.7 Dental hygienists have the most consistent contact with patients and play a vital role in educating them on the various occlusal therapies for managing poor occlusal function and occlusal trauma.
Occlusal equilibration, also known as occlusal adjustment, is the process of selectively grinding tooth structure to reduce traumatic forces at contact points and restore occlusal harmony. For certain occlusal discrepancies, occlusal adjustments are an effective treatment. When used in combination with adequate care, occlusal modification principles and treatment can yield beneficial results for the patient in a shorter time frame and at a lower cost than other occlusion correction treatments.15
Occlusal splints (eg, occlusal guards, oral orthotics, and oral appliances) are removable dental appliances designed to reduce the harmful effects of traumatic forces from grinding, clenching, and other parafunctional habits. Occlusal splints can help manage fremitus and tooth mobility while improving periodontal regenerative outcomes and tooth retention. According to a longitudinal retrospective study, patients who didn’t use occlusal splints and had increased tooth mobility or parafunctional habits exhibited a poorer prognosis and were twice as likely to lose their teeth than those who did.16 Orthodontic treatment is routinely recommended for occlusal correction but may not be accepted by the patient due to expense and long treatment time.15 Additional occlusal therapies include corrective, restorative dental work, orthognathic surgery, and myofunctional therapy.
Additional Considerations
A causative relationship between traumatic occlusion and peri-implantitis, or peri-implant bone loss, has yet to be established. Due to experimental design challenges in regulating the effects of biofilm reduction and traumatic occlusal force, a wide range of variables could produce numerous outcomes.17–20 In the absence of clinical signs of soft tissue inflammation or mucositis, progressive crestal bone loss surrounding implants is rare.18 A human case study examining the correlation of peri-implant bone loss due to occlusal trauma found a correlation when peri-implant mucositis was also present.21 Yet, contrary to those findings, animal studies showed that peri-implant bone loss occurred even in the absence of inflammation.22 Further studies are necessary to determine a causative relationship when biofilm influence is excluded.20,22
Temporomandibular disorders (TMDs) are associated with occlusal disorders, as the muscles of mastication and the temporomandibular joint impact occlusion functions. Aspects of an occlusal evaluation can take place during routine dental hygiene visits. The patient’s inability to open his or her mouth more than four fingers wide may indicate potential TMDs. If a patient experiences a restricted opening, it may indicate an imbalance with the masticatory system. Using a bilateral technique, oral health professionals can assess the movements of the temporomandibular joint by placing fingertips over the joint (anterior to the tragus of the ear) while the patient opens and closes slowly. The patient then shifts his or her jaw to the left and right (movement should be approximately 7 mm to 15 mm in both directions).14 Atypical sounds may be heard or felt such as clicks, pops, and crepitus. While occlusion is not the principal cause of TMDs, it should be considered in treatment planning.
Decreased oral function may correspond to the early stages of cognitive decline. The maximal occlusal force was positively associated with cognitive function both directly and indirectly through dietary intake.23 Additionally, a study by Park et al24 suggests a relationship between cognitive function and chewing ability associated with the number of remaining teeth and the anterior/posterior occlusal patterns. Proper nutrition requires adequate masticatory function, creating a direct link between occlusal status and the risk for malnutrition.25 Chewing efficiency, which is the rate of breakdown of food during mastication, is dependent on the area of the antagonistic occlusal surface.26 The ability to crush and grind food for the intake of essential nutrients is clearly correlated with features of the dentition, such as the number of posterior teeth and occlusal relationships.25
Conclusion
Patients with periodontal diseases, as well as those at increased risk, will reap the greatest benefit from treatment aimed at reducing occlusal forces.13 Dental hygienists with more training or continuing education on identifying occlusal trauma may be better suited to provide guidance in such situations. If traumatic occlusal forces can exacerbate periodontal disease progression, then oral health professionals need to accurately assess occlusal discrepancies that could potentially compound the destructive nature of active periodontal diseases. Furthermore, while tooth mobility is one of the most common signs of occlusal trauma, it may result from periodontal inflammation alone. As such, proper diagnosis and treatment regarding the etiology of mobility can improve the prognosis of periodontal treatment.
References
- United States Centers for Disease Control and Prevention. Periodontitis Among Adults Aged ≥ 30 Years—United States, 2009–2010. Available at: click here. Accessed July 23, 2021.
- Passanezi E, Sant’Ana ACP. Role of occlusion in periodontal disease. Periodontol 2000. 2019;79:129–150.
- Wilkins EM, Wyche CJ, Boyd LD. Clinical Practice of the Dental Hygienist. 12th ed. Philadelphia: Wolters Kluwer; 2017:344–345.
- Chu I, Kennedy D, Hatzimanolakis P. Knowledge of malocclusion supports comprehensive dental hygiene care. Can J Dent Hyg. 2019;53:118–124.
- Kwon T, Lamster IB, Levin L. Current concepts in the management of periodontitis. Int Dent J. December 5, 2021.
- Rodriguez ML, Iturralde M, Vega J, Pinos X. Chronic periodontitis exacerbated by occlusal trauma: report of a case and revision of literature. Dentistry. 2017;7(5):1–4.
- Fan J, Caton JG. Occlusal trauma and excessive occlusal forces: narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S214–S222.
- Harrel SK. Impact of occlusal discrepancies on periodontal disease. Decisions in Dentistry. 2016;2(12):42–45.
- Lasserre JF, Brecx MC, Toma S. Oral microbes, biofilms and their role in periodontal and peri-implant diseases. Materials (Basel). 2018;11:1802.
- Nirola A, Batra P, Mohindra K, Kaur T. Role of occlusion as a risk factor in periodontal disease. J Int Clin Dent Res Organ. 2020;22:321–328.
- Asiri SN, Tadlock LP, Buschang PH. The prevalence of clinically meaningful malocclusion among US adults. Orthod Craniofac Res. 2019;79:129–150.
- Sanadi RM, Chelani LR, Bhakkand SR, Sheth JK. Role of trauma from occlusion in periodontal disease—acontroversy. IOSR J Dent Med Sci. 2016;15:118–122.
- Davies SJ, Gray RJ, Linden GJ, James JA. Occlusal considerations in periodontics. Br Dent J. 2001;191:597–604.
- Call SR. Demystifying occlusion. Dimensions of Dental Hygiene. 2013;11(6):60–65.
- Ferreira CF, Prado AM, Pereira MA, Cardoso AC. The value of occlusion in dentistry: a clinical report showing the correction of an anterior reverse articulation with selective occlusal adjustment. J Prosthodont. 2016;25:407–410.
- Sutthiboonyapan P, Wang HL. Occlusal splints and periodontal/implant therapy. J Int Acad Periodontol. 2019;21:45–50.
- American Dental Hygienists’ Association. Dental hygiene diagnosis: An ADHA white paper. Available at: click here. Accessed July 23, 2021.
- Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Periodontol. 2018;89(Suppl 1):S267–S290.
- Graves CV, Harrel SK, Rossmann JA, et al. The role of occlusion in the dental implant and peri-implant condition: a review. Open Dent J. 2016;10:594–601.
- Isidor F. Influence of forces on peri-implant bone. Clin Oral Implants Res. 2006;17(Suppl 2):8–18.
- Passanezi E, Sant’Ana AC, Damante CA. Occlusal trauma and mucositis or peri-implantitis?. J Am Dent Assoc. 2017;148:106–112.
- Bertolini MM, Del Bel Cury AA, Pizzoloto L, Acapa IRH, Shibli JA, Bordin D. Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review. Braz Oral Res. 2019;33(Suppl 1):e069.
- Ikebe K, Gondo Y, Kamide K, et al. Occlusal force is correlated with cognitive function directly as well as indirectly via food intake in community-dwelling older Japanese: From the SONIC study. PLoS One. 2018;13:e0190741.
- Park T, Jung YS, Son K, et al. More Teeth and posterior balanced occlusion are a key determinant for cognitive function in the elderly. Int J Environ Res Public Health. 2021;18:1996.
- Kikutani T, Yoshida M, Enoki H, et al. Relationship between nutrition status and dental occlusion in community-dwelling frail elderly people. Geriatr Gerontol Int. 2013;13:50–54.
- Schimmel M, Katsoulis J, Genton L, Müller F. Masticatory function and nutrition in old age. Swiss Dent J. 2015;125:449–454.
From Dimensions of Dental Hygiene. August 2021;19(8):32-35.



