 YODIYIM / ISTOCK / THINKSTOCKS
YODIYIM / ISTOCK / THINKSTOCKS
Maximize the Benefits of Computer-Controlled Local Anesthesia Delivery
Fluid pressure and tissue type play important roles in the success of this pain management approach.
The introduction of computer-controlled local anesthesia delivery (CCLAD) has simplified pain management in the dental setting. Ensuring patient comfort is integral not only to treatment outcomes but also in creating a positive dental experience for patients, to support compliance and their return for follow-up care. CCLAD devices deliver local anesthetic drugs in a slow and controlled manner compared with traditional manual syringes. They help improve patient comfort during local anesthesia administration and can be especially helpful for patients with a fear of injections, as the needle is less visible than in manual syringes.
 The ability to consistently maintain slow, safe deposition rates is one benefit of CCLAD devices because it results in reduced pain perception in adults and fewer pain-related disruptions among pediatric patients.1 CCLAD devices also offer rapid onset during administration of the periodontal ligament injection. This helps to address difficult-to-anesthetize teeth and improves the ability to administer supplemental injections when field or block anesthesia is incomplete.2,3 The administration of anesthesia with CCLAD devices offers ergonomic benefits for clinicians, including a reduction in the muscle activity and forces required to give injections and a decrease in the static postures necessary for local anesthesia administration.4
The ability to consistently maintain slow, safe deposition rates is one benefit of CCLAD devices because it results in reduced pain perception in adults and fewer pain-related disruptions among pediatric patients.1 CCLAD devices also offer rapid onset during administration of the periodontal ligament injection. This helps to address difficult-to-anesthetize teeth and improves the ability to administer supplemental injections when field or block anesthesia is incomplete.2,3 The administration of anesthesia with CCLAD devices offers ergonomic benefits for clinicians, including a reduction in the muscle activity and forces required to give injections and a decrease in the static postures necessary for local anesthesia administration.4
A previous publication discussed the ergonomic benefits, injection fluid dynamics, and needle positioning for CCLAD devices.5 This article will focus on the implications of fluid pressure and tissue type when administering local anesthesia with CCLAD systems.
FLUID PRESSURE
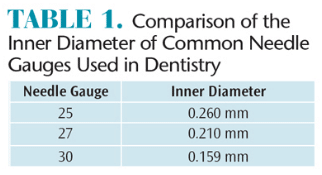
Fluid pressures are created when plungers are depressed to create a flow of anesthetic into the tissue. Many clinicians routinely use small diameter (30 gauge) needles during local anesthesia delivery, assuming they provide greater injection comfort compared with large diameter (27 gauge or 25 gauge) needles.6,7 When considering the fluid dynamics of smaller diameter needles, injection pressures with 30 gauge needles are actually higher than with 27 gauge and 25 gauge needles (Table 1). Increased injection pressure potentially results in increased pain and post-operative discomfort.8–10 In a study by Tzafalia and Sixou,10 significantly more anesthetic was expelled in the first 15 seconds with 27-gauge needles compared to 30-gauge needles.5 Overall, the authors found that more than 80% of the simulated depositions resulted in bursts capable of triggering injection pain during the first few seconds. CCLAD systems are able to administer the anesthetic drop by drop during the initial stage of the injection, with a slow, consistent increase in the injection rate over time, avoiding the pain caused by high fluid pressures. One CCLAD system also monitors and regulates real-time pressures generated at needle tips. This ensures the fluid dynamic pressures are continuously measured and limited to preset values in order to minimize fluid pressures.
TISSUE TYPE
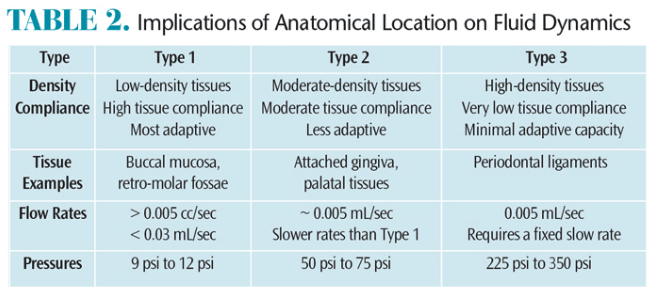
The oral cavity consists of a variety of tissue types. Research has demonstrated that tissue-specific flow rates and optimal pressure values are needed for safe and comfortable injections.1,9 The three basic tissue classifications—type 1, type 2, and type 3—are based on compliance (or distensibility).
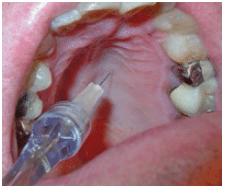
Type 1 refers to low-density tissues with high tissue compliance found in the buccal mucosa and retro-molar fossae (Figure 1). The optimal range of flow rate is greater than 0.005 mL/sec and less than 0.03 mL/sec, producing pressures from 9 psi to 12 psi.
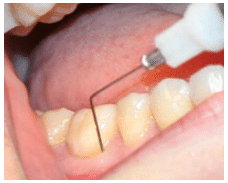
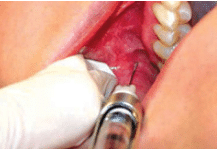
Type 2 includes moderate-density tissues with moderate tissue compliance found in attached gingiva and palatal tissues (Figure 2), which are less adaptive and require slower flow rates than type 1 tissues. The optimal flow rate is approximately 0.005 mL/sec, which produces moderate pressures that range from 50 psi to 75 psi.
Type 3 encompasses high-density tissues with very low tissue compliance (ie, minimal adaptive capacity) found in periodontal ligaments (Figure 3). This type requires a fixed slow flow rate of 0.005 mL/sec and produces a range of tissue pressures from 225 psi to 350 psi.
These tissue types, relevant flow rates, and pressures are summarized in Table 2.
![]() CONCLUSION
CONCLUSION
Patient comfort can be a significant contributor to successful treatment outcomes and patient compliance with recare intervals. Strategies that support patient comfort may help to reduce stress for both patients and clinicians. Implementing technologies, such as CCLAD devices, can reduce injection pressures and pain for patients.
References
- Gibson RS, Allen K, Hutfless S, Beiraghi S. The Wand vs. traditional injections: a comparison of pain related behaviors. Pediatr Dent. 2000;22:458–462.
- Bassett KB, DiMarco AC, Naughton DK. Local Anesthesia for Dental Professionals. Upper Saddle River, New Jersey: Pearson Education; 2010.
- Ferrari M, Crysanti C, Vichi A, Goracci S. Efficacy of the Computer-Controlled Injection System STA, the Ligmaject, and the dental syringe for intraligamentary anesthesia in restorative patients. International Dentistry SA. 2004;11(1):4–11.
- Kaufman KR, An KN, Litchy WJ, Cooney WP 3rd, Chao EY. In vivo function of the thumb muscles. Clin Biomech. 1999;14:141–150.
- Bassett K, DiMarco A. The next generation of pain relief. Dimensions of Dental Hygiene. 2014;12(7):36–38.
- Flanagan T, Wahl MJ, Schmitt MM, Wahl JA. Size doesn’t matter: needle gauge and injection pain. General Dentistry. 2007;55(3):216–217.
- Diggle L, Deeks JJ, Pollard AJ. Effect of needle size on immunogenicity and reactogenicity of vaccines in infants: randomized controlled trial. BMJ. 2006;333:571–578.
- Kudo, M. Initial injection pressure for dental local anesthesia: effectson pain and anxiety. Anesthesia Progress. 2005;52:95–101.
- Hochman MN, Friedman MJ, Williams W, Hochman CB. Interstitialtissue pressure associated with dental injections. Quintessence Int. 2006;37:469–476.
- Tzafalia M, Sixou JL. Administration of anesthetics using metalsyringes. an ex vivo study. Anesth Prog. 2001;58:61–65.
From Dimensions of Dental Hygiene. July 2016;14(07):37–38.