
Achieve Success With Ultrasonic Adaptation
Dental hygienists need to be well versed in technique to achieve positive outcomes with both magnetostrictive and piezoelectric devices.
While utilization of magnetostrictive and piezoelectric devices is similar, there are differences in technique. As dental hygienists become increasingly exposed to both devices, understanding how to use them properly is critical to achieving optimal outcomes. Eradicating the causes of gingival and periodontal inflammation generally requires complete root surface debridement. Disruption of tooth-adherent calculus and biofilm occurs via mechanical vibrations when the ultrasonic insert/tip (UIT) is sufficiently powered and in direct contact with the tooth surface.1 So as to not damage the tooth itself, clinicians need to understand the differences in lateral forces, tip adaptations, and power settings between magnetostrictive and piezoelectric devices.2–4
The most energized portion of a UIT is the tip. All sides of both magnetostrictive and piezoelectric UITs can transmit energy; however employing appropriate tip adaptation controls energy dispersion. Magnetostrictive inserts transmit energy on all sides, including concave and convex aspects. On the other hand, the lateral sides of piezoelectric tips are typically implemented because they are able to transfer the most energy during deposit removal.5,6
ADAPTATION WITH MAGNETOSTRICTIVE UNITS

COPYRIGHT MICHAELA NGUYEN, RDH, MS
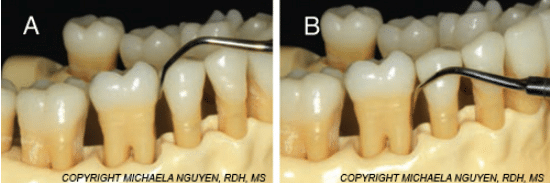
When using a magnetostrictive scaler for supragingival biofilm and calculus removal on the distal and mesial aspects of proximal teeth, the insert is adapted at 0° to 15° to the crown. The tip is pointed toward the apex of the tooth or underneath the contacts using vertical, oblique, or horizontal strokes into the interproximal aspects of the tooth surfaces. When using this technique subgingivally, the adaptation of the insert can be challenging. For example, if the concave face of the insert is against the distal surface, directed to the proximal surface, entry to the base of the pocket may be hindered and forced entry will distend the tissue. The middle to heel of the insert is inhibited by the gingiva, restricting access to the sulcus where soft and hard deposits reside (Figure 1).

COPYRIGHT MICHAELA NGUYEN, RDH, MS
On the other hand, if the insert is inserted below the cementoenamel junction with the tip toward the apex and the concave face against the distal surface, the adaptation is altered. The point of the insert is now against the tooth, increasing the risk of cutting a groove into the root surface (Figure 2). The contact between the point of the insert and the root surface increases when moving subgingivally with a choked-up pen grasp.
To reduce the likelihood of damage and to improve adaptation, start with the insert pointing toward the apex. Using a same-arch fulcrum, lower the handle slightly to better utilize the concave anterior portion of the insert. Proceed to the base of the pocket by repositioning the handle away from the tooth, using primarily the lateral side of the insert with a vertical probe-like stroke (Figure 3A and Figure 3B).

While correct adaptation to the curvatures of the tooth is applied during calculus removal, using the lateral sides of a magnetostrictive insert with inadequate power can result in burnished calculus. To prevent this, a systematic multidirectional stroke sequence with the use of the first 2 mm to 4 mm of the insert is key. When fracturing subgingival ledges of calculus, navigate from the gingival margin to the epithelial attachment and modulate the power from medium to high using methodical multidirectional strokes. In order to pulverize the calculus, insert the UIT in an apical direction. Use the tip’s point to tap on the top of the ledge with slow, channeling vertical strokes. Once the ledge has been fractured, follow with slow overlapping horizontal or oblique strokes, moving from areas with no deposits to areas with calculus present. Clinicians should not begin with horizontal strokes because they may shave the calculus and increase the risk of leaving burnished sheets on the root surface. On the mesial surface, the convex back side of the insert can easily adapt to the crown. To maintain tip adaptation subgingivally, negotiate the handle by either slightly lifting or lowering it to complement the root surface (Figure 4A and Figure 4B).
ADAPTATION WITH PIEZOELECTRIC UNITS

The adaptation when instrumenting with a piezoelectric unit is similar to that used with a universal curet. If the convex and concave backs of the tip are used, a high-pitched auditory sound is emitted and hammering to the tooth will occur (Figure 5). The initial application of the piezoelectric tip differs from the magnetostrictive because the concave face and convex back are not as effective as the lateral surfaces of the tip. For the mesial and distal surfaces, clinicians should swing the handle away from the tooth and use the lateral sides of the tip with vertical strokes
(Figure 6). The prospect of
burnishing calculus when using the lateral sides of a piezoelectric tip is less likely, predominantly due to tip design. The cylindrical tip design of a magnetostrictive insert increases the potential for shaving calculus and leaving burnished sheets. The beveled edge tip of a piezoelectric tip aids in breaking up the calculus, thus decreasing the risk of burnishing.5
An alternative approach involves crossing the tip over the occlusal plane, with the tip pointing into the sulcus and applying vertical probe-like or oblique strokes. As the tip advances under the contact, the tip will hit the crown of the tooth, which can obstruct the tip from fully reaching into the proximal surface (Figure 7). Both of these techniques can be effective, depending on the specific clinical case. Clinicians should pay close attention to tip adaptation/angulation, access to proximal surfaces, and root anatomy to determine the optimal technique.
To support optimal outcomes, a blended approach is most appropriate, using a variety of different hand and ultrasonic instruments depending on the task at hand.
References
- Pattison AM, Matsuda S, Kiehl N. Ultrasonic Therapy in the 21st Century. Dimensions of Dental Hygiene. 2014;12:40–44.
- Hodges KO. Decision making related to nonsurgical periodontal therapy. In: Dental Hygiene: Theory and Practice. 4th ed. St. Louis: Saunders/Elsevier; 2015.
- Flemmig TF, Petersilka GJ, Mehl A, Hickel R, Klaiber B. Working parameters of a magnetostrictive ultrasonic scaler influencing root substance removal in vitro. J Periodontol. 1998;69:547–53.
- Yousefimanesh H, Robati M, Kakhodazadeh M, Molla R. A comparison of magnetostrictive and piezoelectric ultrasonic scaling devices: an in vitro study. J Periodontal Implant Sci. 2012;42:243–247.
- Pattison AM, Matsuda SA, Pattison GL. Ultrasonics—A New Perspective. Dimensions of Dental Hygiene. 2003;1(3):32–35.
- Hodges KO. Ultrasonic instrumentation. In: Dental Hygiene: Theory and Practice. 4th ed. St. Louis: Saunders/Elsevier; 2015.
From Dimensions of Dental Hygiene. July 2016;14(07):32,34.

