 MAYA KOVACHEVA / ISTOCK / THINKSTOCK
MAYA KOVACHEVA / ISTOCK / THINKSTOCK
Addressing the Symptoms of Dentinal Hypersensitivity
Proper diagnosis and staying abreast of the latest treatment strategies are the basis of effectively Managing this common dental complaint.
Dentinal hypersensitivity (DH) is a common condition that can interfere with patients’ quality of life. Determining the exact number of adults affected is challenging because DH’s prevalence varies greatly among studies.1,2 This may be due to differences in study locations and assessment methods, such as questionnaires vs clinical examinations.2 In general, women age 20 to 40 are more likely to develop DH than men, and the prevalence is higher in periodontally involved patients (60% to 98%).1 Proper diagnosis and staying abreast of the latest treatment approaches are key to effective DH management.

Recession with dentinal exposure is one of the primary causes of DH. However, dentinal tubules can become exposed through other conditions, including erosion, attrition, and abrasion (Figure 1).3 Erosion results from recurrent intake of acidic foods, drinks, or substances, which then dissolve the apatite crystals of the enamel. Medical conditions that involve reflux or vomiting, such as gastroesophageal reflux disease and bulimia, can lead to erosion of the enamel. In addition, erosion can result from medications, such as effervescent cold tablets, vitamin C supplements, and aspirin. There have also been cases of swimmers developing erosion from swallowing excessively chlorinated pool water.4 Once the enamel is deteriorated by erosion, the acidic substance enters the dentin via dentinal tubules and causes DH.4
Abfraction can cause tubules to become exposed (Table 1). Abfraction is thought to be caused by opposing teeth that exert intermittent loading that flexes nonmobile teeth with which they occlude. Research has suggested that abfraction is not caused by normal mastication or swallowing; rather, it is caused by activities such as bruxism.5 These strong intermittent forces cause the facial and lingual surfaces of involved teeth to endure compressive forces that are much greater and of longer duration than normal. It is unlikely that mobile teeth will develop abfractive lesions because the teeth jiggle in response to loading and off-loading.6 Abfractions manifest as wedged-shaped lesions that typically appear in the cervical areas of the teeth. Over time, these lesions can increase in size as underlying dentin is exposed to the oral environment as brittle cervical enamal breaks away. Once the dentinal tubules are exposed, sensitivity may become a concern.
The pain sensation associated with DH can be explained according to the commonly accepted hydrodynamic theory, proposed by Brännström.7 Changes in the volume or direction of fluid flowing within dentin tubules triggers impulses to the pulpal nerves, which can result in the sensation of pain.8 DH is characterized by brief, sharp pain resulting from thermal, tactile, osmotic, chemical, or evaporative stimuli.9 In severe cases, vague, delayed, or prolonged pain may follow the stimulation.10 Before a DH diagnosis can be made, a careful differential diagnosis is needed. Other conditions that mimic DH—such as post-operative sensitivity following restorative dentistry, cracked teeth, whitening-related sensitivity, fractured restorations, dental caries, and related pulpitis—should be ruled out.2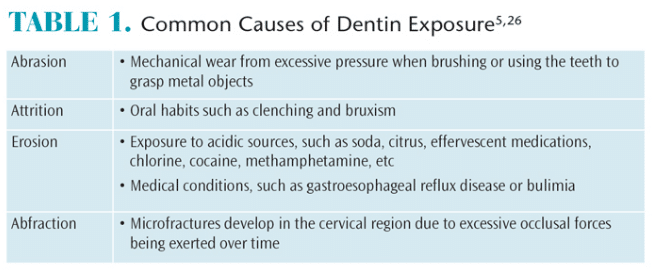
Theoretically, any substance that aids in tubule occlusion or reducing the number and/or diameter of tubules will help improve the symptoms of DH.11 Available agents to reduce or eliminate DH can be categorized by two mechanisms of action: reducing/blocking neural transmission and physically occluding open tubules.2 Strontium chloride, potassium nitrate, and fluoride varnish are helpful for decreasing nerve function.10 Traditionally, desensitizers based on oxalic and/or potassium oxalate have been the gold standard for occluding dentinal tubules.11
POTASSIUM NITRATE
Potassium nitrate is the most common therapeutic agent for decreasing pulpal nerve excitability. However, a recent meta-analysis of six studies on potassium nitrate dentifrices was unable to offer strong support for the use of potassium salts in DH management.2 Other research has found, however, that potassium nitrate-containing dentifrices produced a statistically significant reduction in DH after the product had been used for 2 weeks to 4 weeks.1 Patients should be informed that they must use the product as directed in order to obtain maximum results.
In an effort to find additional methods for DH relief, researchers are comparing traditional desensitizing dentifrices containing potassium nitrate to other products that might also be effective. For instance, a clinical trial compared the following treatment groups: sodium fluoride dentifrice used in conjunction with a mouthrinse containing 1.4% potassium oxalate; sodium fluoride dentifrice alone; and desensitizing toothpaste with 5% potassium nitrate alone.12 Both the potassium oxalate mouthrinse and potassium nitrate dentifrice groups showed decreased sensitivity compared to the group that used the sodium fluoride dentifrice alone.12 This study shows promising results for the use of potassium-based mouthrinse to help relieve DH symptoms.
Potassium nitrate has been shown to be effective alone or in combination with other agents, such as strontium chloride. A Chinese study found that patients with DH symptoms experienced rapid improvement after using a dentifrice containing 2% strontium chloride and 5% potassium nitrate.13
ARGININE-CALCIUM CARBONATE
Arginine is an amino acid that has been shown to provide DH relief. When calcium carbonate was combined with arginine, remineralization occurred that was similar to the naturally occurring biological process of tubule occlusion by salivary glycoproteins that may later calcify.2 A dentifrice containing 8% arginine, calcium carbonate, and fluoride (not currently available in the US) was found to be superior over a 2% potassium ion dentifrice at reducing the symptoms of DH in an 8-week study.2 A paste containing arginine and calcium carbonate is currently available for in-office use. This may be beneficial for patients who haven’t experienced DH relief with at-home products.
CALCIUM PHOSPHATE TECHNOLOGIES
Calcium phosphate technologies are also used to treat DH. Amorphous calcium phosphate (ACP) makes calcium and phosphate ions available in saliva, which may encourage remineralization, thus decreasing DH.14 Casein phosphopeptide-ACP, or Recaldent®, is a milk protein derivative that imitates the natural remineralization process. Kowalczyk et al15 evaluated the effects of Recaldent paste on DH and determined that it was not effective in the short term, but results of another study showed that topical placement of Recaldent reduced DH through the deposition of calcium phosphate compounds onto the tooth structure.16,17
Bioglass is a biocompatible material composed of silicon dioxide, sodium oxide, calcium oxide, and phosphorus oxide.9 Bioglass works to occlude dentinal tubules through the deposition of hydroxycarbonate apatite (HCA) onto the tooth surface.18,19 Studies have also investigated the potential use of bioglass–containing pastes in post-operative management of DH associated with periodontal surgery.2 Bioglass powder reacts with body fluids to deposit HCA, which is similar to natural tooth minerals. When this powder is applied through the use of an air polisher, it may ease DH symptoms by creating a dentin surface more resistant to citric acid attack.11 In addition, a recent clinical study demonstrated the effectiveness of bioglass in reducing DH when applied in a prophylaxis paste.1
Tri-calcium phosphate slowly releases calcium to the tooth surface. It is designed to improve the remineralizing effects of fluoride, while also decreasing DH.17,20
FLUORIDE
Fluoride applications through the use of dentifrice, varnish, or topical gel can help reduce DH caused by exposed dentinal tubules. Fluoride products work by occluding the tubules, which decreases fluid movement and permeability.21 High-concentration fluoride varnish (applied in the dental office) is effective in providing instant relief from DH through tubular occlusion.1
Fluoride products, such as sodium fluoride and stannous fluoride, aid in DH relief through tubule occlusion. A randomized controlled study demonstrated the effectiveness of 5% sodium fluoride varnish products for DH, as indicated by responses to air and cold tests using a visual analog scale over a 24-week period.2 Topical fluoride gel (1.23% sodium fluoride) may decrease post-operative sensitivity associated with tooth-whitening procedures.2 Fluoride gels are primarily applied in-office using disposable trays but can also be applied at-home using a custom tray.
GLUTARALDEHYDE AND DENTAL ADHESIVES
Glutaraldehyde is another desensitizing agent that blocks dentinal tubules. Because glutaraldehyde has been shown to be effective when used alone, there has been an effort to add products to glutaraldehyde to see if results can be improved. For example, a product composed of an aqueous solution of 5% glutaraldehyde and 35% hydroxyethyl methacrylate has shown to help reduce DH symptoms for up to 7 months to 9 months.2
The in-office application of dentin bonding agents can also be used to occlude dentinal tubules. Research has demonstrated their ability to reduce DH symptoms for up to 1 month.22,23 A light-cure resin may lengthen anti-DH effects to several months.24
CONSIDERATIONS FOR LASER USE
The use of lasers in DH reduction has gained considerable interest in the recent years. Some of lasers’ reported advantages in DH reduction include higher rates of patient response, longlasting results, predictable effects, and ease of application. However, the proper settings must be used in order to prevent any thermal damage to the pulp.9,10
Lasers used for the treatment of sensitive teeth are usually low-powered—such as helium-neon and diode lasers—or medium-powered lasers, such as neodymium-doped yttrium aluminum garnet (Nd:YAG) and carbon dioxide (CO2) models. Based on a clinical evaluation, the diode laser and sodium fluoride varnish showed similar effectiveness in reducing DH. However, the low-level laser showed better results for treating teeth with high levels of sensitivity.3 In a laboratory study by Al-Azzawi and Dayem,25 the findings suggest there was no significant difference between the occluding effect of an Nd:YAG laser and potassium nitrate toothpaste.
An in vitro study evaluated the occluding effects of four different lasers. Results showed that all four lasers were able to melt the peri- tubular dentin and partially or totally occlude dentinal tubules. However, the 810-nm diode laser did not seal the tubules as completely and may not be as helpful with DH reduction.10 In order to most effectively manage DH symptoms using lasers, clinicians must have a thorough understanding of the benefits and limitations of each type of laser. When considering lasers for the treatment of DH symptoms, studies should be reviewed to determine if there is a clinical example that indicated the effectiveness of the laser in a similar case.
PATIENT EDUCATION
Early detection and mitigation of circumstances that expose patent dentinal tubules are important to preventing further damage to the dentition and to managing DH. Fewer exposed and patent dentinal tubules will reduce the pain caused by thermal, tactile, evaporative, osmotic, and chemical stimuli.9 Determining the cause of DH is critical to providing proper counseling and education for patients (Figure 2). Patients may need guidance on proper nutrition and appropriate oral hygiene instructions so as not to cause the re-exposure of occluded tubules or the exposure of additional dentinal tubules to the oral environment. Clinicians should advise patients to choose less acidic foods and suggest ways to consume acidic foods without causing additional damage.
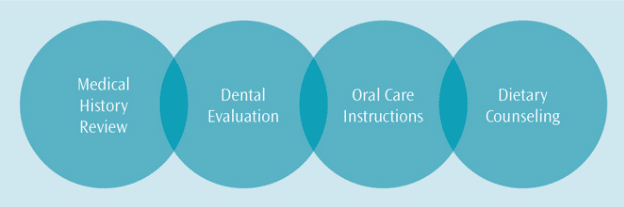
If diet is suspected as a significant factor in DH, patients should record their complete dietary intake for four consecutive days, including the time of day and exact quantities of all ingested foods and beverages.26 The diary will shed light on what types of foods are being consumed, length of time the dentition is exposed to acids, and provide information that may be used to modify diet so as to help mitigate DH. Follow up is crucial to monitor patients’ conditions and compliance.
CONCLUSION
Dental hygienists play important roles in the detection and management of DH. Educating patients on the etiology of DH and providing appropriate management strategies can be helpful to patients. Providing counseling, recommending self-care products, and applying in-office agents as needed fall under the purview of dental hygienists. Placing the patient at the center of the process, while incorporating the latest evidence and professional insight, will lead to more successful management of DH symptoms.
References
- Mantzourani M, Sharma D. Dentin sensitivity: Past, present and future. J Dent.2013;41(Suppl 4):S3–S17.
- Shiau H. Dentin hypersensitivity. J Evid Base Dent Prac. 2012;S1:220–228.
- Corona S, Nascimento T, Catirse A, Lizarelli R, Dinelli W, Palma-Dibb, R.Clinical evaluation of low-level laser therapy and fluoride varnish for treating cervical dentinal hypersensitivity. J Oral Rehab. 2003;30:1183–1189.
- Meurman JH, ten Cate JM. Pathogenesis and modifying factors of dentalerosion. Eur J Oral Sci. 1996;104:199–206.
- Bartlett DW, Shah P. A critical review of non-carious cervical (wear) lesionsand the role of abfraction, erosion and abrasion. J Dent Res. 2006;85:306–312.
- Grippo J, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfractionrevisited: A new perspective on tooth surface lesions. J Am Dent Assoc. 2004;135:1109-–1118.
- Brannstrom M. The elicitation of pain in human dentine and pulp bychemical stimuli. Arch Oral Biol. 1962;7:59–62.
- Li Y. Dentin hypersensitivity: diagnosis and strategic approaches. Available at:cdeworld.com/courses/4674. Accessed June 22, 2016.
- Lee B, Chang C, Chen W, Lan W, Lin C. in vitro study of dentin hypersensitivitytreated by Nd:YAP laser and bioglass. Dental Mater. 2005;21:511–519.
- Gholami G, Fekrazad R, Esmaiel-Nejad A, Kalhori K. An evaluation of theoccluding effects of Er; Cr:YSGG, Nd:YAG, CO2 and Diode lasers on dentinal tubules: a scanning electron microscope in vitro study. Photomed Laser Surg. 2011;29:115–121.
- Sauro S, Watson T, Thompson I. Dentine desensitization induced byprophylactic and air-polishing procedures: An in vitro dentine permeability and confocal microscopy study. J Dent. 2010;38:411–422.
- Sharma D, McGuire JA, Gallob JT, Amini P. Randomised clinical efficacy trialof potassium oxalate mouthrinse in relieving dentinal sensitivity. J Dent. 2013;41:S40–S48.
- Liu H, Hu D. Efficacy of a commercial dentifrice containing 2% strontiumchloride and 5% potassium nitrate for dentin hypersensitivity: a 3-day clinical study in adults in China. Clin Ther. 2012;34:614–620.
- Orchardson R, Gillam DG. Managing dentin hypersensitivity. J Dent Assoc.2006;137:990–998.
- Kowalczyk A, Botulinski B, Jaworska M, Kierklo A, Pawinska M, Dabrowska E.Evaluation of the product based on Recaldent technology in the treatment ofdentin hypersensitivity. Adv Med Sci. 2006;51(Suppl 1):40–42.
- Yuan P, Shen X, Liu J, et al. Effects of dentifrice containing hydroxyapatite ondentinal tubule occlusion and aqueous hexavalent chromium cations sorption: a preliminary study. PLoS One. 2012;7:45283.
- Withers S, Friesen D, Li Y. Dentinal Hypersensitivity Management.Dimensions of Dental Hygiene. 2015;13(4):25–32.
- Lynch E, Brauer D, Karpukhina N, Gillam D, Hill R. Multicomponentbioactive glasses of varying fluoride content for treating dentin hypersensitivity. Dent Mater. 2012;28:168–178.
- Wang Z, Sa Y, Sauro S, et a;. Effect of desensitising toothpastes on dentinaltubule occlusion: A dentine permeability measurement and SEM in vitro study. J Dent. 2010;38:400–410.
- Karlinsey RL, Mackey AC. Solid-state preparation and dental application ofan organically-modified calcium phosphate. J Mater Sci. 2009;44:346–349.
- Galvao Arrais CA, Micheloni CD, Giannini M, Chan, DCN. Occluding effect ofdentifrices on dentinal tubules. J Dent. 2003;31:577–584.
- Ozen T, Orhan K, Avsever H, Tunca YM, Ulker AE, Akyol M. Dentinhypersensitivity: A randomized clinical comparison of three different agents in a short-term treatment period. Oper Dent. 2009;34:392–398.
- Yu X, Liang B, Jin X, Fu B, Hannig M. Comparative in vivo study on thedesensitizing efficacy of dentin desensitizers and one-bottle self-etching adhesives. Oper Dent. 2010;35:279–286.
- Shiau HJ. Chairside management of dentinal hypersensitivity. Dimensions ofDental Hygiene. 2016;14(4):18–23.
- Al-Azzawi L, Dayem R. A comparison between the occluding effects of theNd:YAG laser and the desensitising agent Sensodyne on permeation through exposed dentinal tubules of endodontically treated teeth: An in vitro study. Arch Oral Bio. 2006;51:535–540.
- Lussi A, Jaeggi T, Zero D. The role of diet in the aetiology of dental erosion.Caries Res. 2004;38(Suppl 1):33–44.
From Dimensions of Dental Hygiene. July 2016;14(07):40–43.

