Material Selection and Maintenance
By staying abreast of today’s restorative materials, clinicians will be prepared to safely and effectively care for them.
This course was published in the March 2014 issue and expires March 31, 2017. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Examine the physical and mechanical properties of restorative materials.
- Discuss the durability, function, and esthetic qualities of available restorative materials.
- Detail how to optimally maintain esthetic restorations.
- Educate patients on how to care for their restorations.
Oral health professionals work with a variety of dental restorative materials. Material selection hinges on several factors that are individual to each patient. In order to help patients understand the different restorative options, clinicians need to be well versed in the properties of each material.
When considering which restorative material is best for the patient, the physical and mechanical properties of the material must be considered. Physical properties include color, density, and thermal conductivity, while mechanical properties pertain to the material’s ability to withstand forces.
Oral health professionals should be able to explain the benefits of restorative selections to patients and provide proper care and maintenance of restorations once they have been placed.
CONSIDER THE OPTIONS
While many restorative materials offer similar characteristics, each type brings its own element of value and benefit. For instance, density refers to the mass/unit volume of a material but does not necessarily rate the hardness or toughness of a material. Where the restorative material will be placed in the oral cavity may aid clinicians in the selection process. For example, posterior restorations need to withstand the forces of mastication, so the material should be able to resist varying amounts of stress, such as compression and shearing forces.
Amalgam and composites are direct restorations commonly used to replace tooth structure. These materials are mixed and placed directly into the oral cavity, where they will chemically set to restore the lost dentition. Amalgams gain their strength by the mixture of metals used to create the final restoration. Particle size and shape of the metals contribute to amalgam’s hardness and durability. These metal alloy particles may be irregularly shaped or spherical. The shape of the particles affects the overall mix of the material. The resulting dental amalgam may produce a consistency that is comparatively dry, with irregular-shaped particles, or wet, with spherical particles. This will affect the setting time of the material, as well as the strength of the final restoration.
Composites are also classified according to filler particle size and shape. Manufacturers use engineered glass materials coated with a silane coupling agent to formulate a material that has strength, hardness, and an esthetic appearance. The characteristics of composite filler particles encompass macro-, micro-, and nanoparticles. Microhybrid composites, also referred to as universal restorative composites, are made of different-sized filler particles.1 These composites have good mechanical properties and are suitable for posterior restorations. Restorations that require increased strength for functional reasons often provide relatively poor esthetic qualities. Therefore, microhybrid composites are not the material of choice for anterior restorations.2
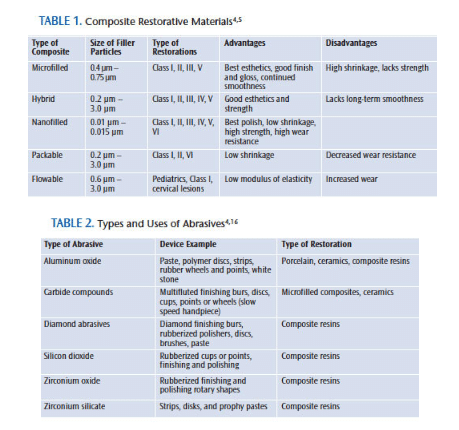
Anterior restorations must match the natural dentition, so color and hardness are important. Microfilled composites offer high-quality esthetics, but relatively poor mechanical strength. Nanocomposites offer superior esthetic and mechanical characteristics, great polishability, and maintain a lustrous finish. This smooth surface finish provides a reduced chance of discoloration and staining—making nanocomposites an excellent choice for anterior restorations.3 Table 1 provides details on the different kinds of composite restorative materials.1,4,5
When evaluating a restorative material, three main components should be considered: durability, function, and esthetics. Location of the restoration within the dentition, amount of existing tooth structure, and intended longevity of the restoration’s use should also be considered during material selection. Amalgams, composites, veneers, crowns, and removable dentures are the main types of restorations used today.6
![]() DURABILITY
DURABILITY
Durability refers to the ability of a material to withstand wear, pressure, or damage. Metals and porcelains are very durable materials, and are often used in crowns and other types of restorations. They are both resilient and tough, and can absorb forces without easily breaking or becoming deformed. Porcelain may fracture, however, under certain shearing stresses, and amalgam may creep or become distorted in shape under compression. Generally, porcelain and amalgam are used when significant tooth structure has been lost. Metals are durable but not esthetically appealing. They are often used for casting crowns, and they provide strength without being visible. Porcelain, when used properly, is very esthetic, but it has limitations. An indirect material, porcelain requires special processing outside of the mouth. It may present challenges with creating defined margins that may appear bulky.
All-ceramic crowns and bridges have replaced porcelain-fused-to-metal fixed restorations in some instances. The most commonly used ceramic materials include dispersion-strengthened glass ceramics, which are suitable for anterior crowns and inlays; glass-infiltrated ceramics used for anterior bridges and posterior crowns; and Y-TZP zirconia utilized for all-ceramic crowns and multiple-unit posterior bridges. These fracture-resistant ceramic materials provide excellent mechanical properties and pleasing esthetics.7
Composites provide durable options but may not resist abrasion, and they can discolor over time. Advances in resin technology have created more choices with nanocomposites, of which there are two main groups: nanohybrids and nanofilled composites. Nanohybrids consist of particles of various sizes and shapes, whereas nanofilled composites contain particles of nearly uniform size and consistency. Nanofilled composites may provide the refined polishing properties of microfilled composites and the mechanical strength of hybrid composites.8
FUNCTION
Function refers to a material’s performance. The amount of force a restoration may endure, the way a restoration is fabricated or placed, and the patient’s personal expectations should all be considered when choosing the best-suited material. The use of mercury-containing amalgams is controversial, but studies support its use as a safe restorative option. Amalgam provides longevity, is cost effective, and is less technique sensitive than other restorative materials. However, it is esthetically unappealing and requires preparatory considerations that may result in removing sound tooth structure.9
Amalgam cavity preparation requires significant tooth structure removal in order to facilitate contoured undercuts for mechanical retention of the material. Composites, on the other hand, require little tooth structure removal due to the bonding adhesion that is used to retain the restorative material. Composites have greatly improved over the years. Their functionality equals amalgams in most situations. However, cost considerations and/or the amount of remaining tooth structure may necessitate the need for other restorative choices.10
Crowns and veneers are excellent choices when significant tooth structure has been lost. Fracture resistance is a consideration with veneers and crowns. Porcelain is strong and resilient but stiff. Zirconia, which is used as an orthopedic material, exhibits high flexural strength and toughness. Innovations to this material have offered alternative clinical options to patients who prefer all-ceramic restorations. They provide a lustrous finish with strong mechanical strength and high fracture resistance.8
ESTHETICS
Cosmetic restorations, including composites, ceramics, and dentures, are used to improve an individual’s appearance. For the most part, this negates the use of metals. These options provide esthetic results, but each has unique properties. Composites provide a cost-effective choice, and may offer an interim option for cases that need extensive restorative care. Porcelain restorations provide extended longevity and more luster due to the glazing phase that provides a smooth surface. This finish corrects the microscopic voids that occur during the fabrication process, strengthens the restoration, and helps to reduce bacterial growth on the final prosthesis.9
RESTORATION MAINTENANCE
The care and maintenance of dental restorations are the responsibility of both dental hygienists and patients. In clinical practice, the appropriate use of dental instruments and polishing agents is important to maintaining the original integrity of the restoration. Rough surfaces on composite restorations favor bacterial adhesion and biofilm formation. These areas may be more prone to secondary caries, gingivitis, and periodontal diseases. Surface roughness of resin composites can be iatrogenic if inappropriate polishing agents are used or if hand or ultrasonic instruments are incorrectly adapted to the tooth surface.11
Defects can occur on tooth structures and restorative materials, creating an environment that harbors plaque accumulation. Surface roughness of the teeth and dental restorations can cause esthetic and gingival problems. Gingival-contact sites can be prone to constant plaque accumulation, which leads to gingival irritation. These areas may be congenital or iatrogenic in nature.
Hand instrumentation is the prudent choice when scaling and root planing patients with dental restorations. The mechanical energy produced by ultrasonic scalers on the tooth surface can create surface roughness.12 The incorrect adaptation of ultrasonic inserts/tips (UITs) can cause scratches, gouges, and surface irregularities that promote microleakage of microorganisms into dental tissues, leading to recurrent decay or pulpitis.13
Arabaci et al14 found that the use of an ultrasonic scaler caused more surface roughness on amalgam restorations when compared to composite and porcelain restorations. In the study, the amalgam restorations sustained chips, scratches, and loss of material after instrumentation with UITs. Two of the UITs tested caused roughened composite surfaces and removal of the porcelain glaze on veneers and crowns, which caused pores in the surface.14
INDICATIONS FOR POLISHING
Crowns that require occlusal adjustment lose their glazed finish when an occlusal correction is required. These surfaces need to be properly polished to restore a fine finish. Otherwise, the roughened surface will lead to debris and calculus adhesion.15
Composite restorations undergo a different process than amalgams, due to polymerization of the material. Unlike amalgams, which are carved and burnished to create a restoration with no irregularities, composite restorations are completed with finishing burs and diamond burs. Polishing begins with discs and finishing strips, then polishing pastes are used. Abrasive agents affect the integrity of tooth surfaces and restorations. These agents contain natural and synthetic materials that vary in hardness, particle shape, and particle size. A very hard abrasive can produce minimal abrasion if its particle size is very fine to superfine. Fine pumice, silicon dioxide, zirconium silicate, and/or calcium carbonate are some of the active ingredients used in prophylaxis pastes. Table 2 describes the types of abrasives used in restorative care.4,16
Several factors determine the abrasiveness of a polishing agent. Hardness of the agent is related to its effectiveness. To polish a surface, the particles of the abrasive agent must be harder than the surface being polished. Ideally, the least abrasive agent should be used to minimize scratching the surface and to achieve a lustrous finish. Particle shape in an abrasive or cleaning agent can be angular or spherical. Irregular particle shapes have angular edges that can scratch the surface being polished. Particle size, also known as grit, affects the surface texture after polishing. A fine grit produces the least amount of surface abrasion, even if the particles are extremely hard. A coarse grit can scratch and roughen surfaces, degrading the overall finish of a restoration or tooth structure. Prophylaxis pastes containing microfine white sapphire particles are suggested to preserve the luster of veneers, gold, and porcelain restorations, as well as natural teeth.
Choosing an appropriate prophylaxis paste for different restorative materials can be challenging. Manufacturers’ standards for defining superfine, fine, medium, or coarse grit can vary. It is important to read product descriptions to determine the polishing agent’s indications and compatibility with various dental materials.17
Proper technique is imperative when polishing restorations. Ideally, clinicians should use the least abrasive agent on wet surfaces to minimize scratching enamel or restorations. Abrasive agents applied to a moist tooth surface or a restoration will elicit a smoother effect than applying the agent to a dry surface. If a coarse agent is utilized, it should be followed by a finer abrasive to establish a lustrous finish. Agents that are too abrasive for cosmetic restorations can result in the creation of rough surface textures and the retention of biofilm and deposits. The rule of thumb is to select the least abrasive grit that will effectively remove discolorations.
Amalgams, gold, and composite restorations will exhibit some surface roughness with abrasive pastes. Therefore, clinicians should use pastes specially designed for cosmetic restorations or mild, nonabrasive toothpastes to maintain restorations properly. Polishing removes extrinsic stain and soft deposits. However, no single polishing agent is appropriate for all situations. The selection of the proper polishing agents and the delivery system is important to maintain the integrity of the existing restorations.
Rubber cup selection may also help with reducing the amount of cleaning agent needed. Webbed prophy cup designs are flexible and retain less paste than ribbed cups. In cases where using less polishing paste is indicated, the use of a web-shaped prophy cup can reduce abrasiveness. Light, intermittent strokes with the rubber cup are recommended.
AIR POLISHING AND RESTORATIVE MATERIALS
Recent research shows that air polishing may be more effective at stain and plaque removal than polishing with rotating cups, brush cones, and abrasive pastes.18,19 Air polishing on some restorative materials, however, should be avoided to prevent a matte finish, surface roughness, pitting, and loss of marginal integrity. When air polishing is indicated, powder selection is very important. Sodium bicarbonate-based powders were the first powders used in air polishing, but the armamentarium has expanded to include glycine, calcium sodium phosphosilicate, calcium carbonate, and aluminum trihydroxide powders. Manufacturers of recently developed powders claim these are less abrasive than traditional sodium bicarbonate-based powders.18
 Pelka et al19 found that glycine powder produced significantly less surface damage on restorative materials than two sodium bicarbonate-based powders. Calcium sodium phosphosilicate powder is a bioactive glass that, in addition to excellent plaque and stain removal, has exhibited positive results with dentinal hypersensitivity. Calcium carbonate is an air-polishing powder with spherically agglomerated crystals. This powder has been effective in stain removal, but more clinical studies are needed to determine its effect on root surfaces.
Pelka et al19 found that glycine powder produced significantly less surface damage on restorative materials than two sodium bicarbonate-based powders. Calcium sodium phosphosilicate powder is a bioactive glass that, in addition to excellent plaque and stain removal, has exhibited positive results with dentinal hypersensitivity. Calcium carbonate is an air-polishing powder with spherically agglomerated crystals. This powder has been effective in stain removal, but more clinical studies are needed to determine its effect on root surfaces.
Aluminum trihydroxide air-polishing powder has particles that are harder but comparable in size to sodium bicarbonate. Due to the hardness of this powder, aluminum trihydroxide should be avoided on most esthetic restorations. Whenever air polishing is indicated, the spraying distance from the nozzle to the tooth structure must be considered. An optimum distance of 2 mm to 7 mm from the polishing tip to the tooth restoration will reduce the risk of damage to the restoration and improve patient comfort.13
SELF-CARE RECOMMENDATIONS
Self-care instruction is relatively straightforward, but should be individualized for each patient. Plaque biofilm management and dietary guidance must be addressed.
The decision on whether to use a manual toothbrush or power toothbrush is dependent on individual patient factors, but soft toothbrush bristles should be recommended. Patients should be advised against using abrasive toothpastes. Interdental cleaning is recommended in all situations, and can include the use of floss, interdental brushes, picks, flossing aids, wooden or rubber tips, or toothpicks. Mouthrinses that contain carbamide peroxide, chlorhexidine gluconate, and alcohol can damage some composite restorations, so prolonged use should be avoided.4,20–22
When providing dietary counseling, patients should be informed that different foods and drinks can stain restorative materials. Coffee, tea, blueberries, red wine, and tobacco products can cause discoloration, so patients should be advised to reduce or eliminate their exposure to these potentially discoloring substances.4
SUMMARY
Utilizing a patient-centered approach and encouraging patient participation are key to improving oral health. Dental hygienists need to consider the available research, individual patient needs, and their clinical experience to provide the most effective care possible.23
Evaluating material content and suggesting proper care instructions to patients are paramount to sustaining the overall performance of restorations. Dental hygienists need to stay abreast of any advancements in restorative materials in order to best advise patients and provide the most effective care.
REFERENCES
- Puckett AD, Fitchie JG, Kirk PC, Gamblin BS. Direct composite materials. Dent Clin N Am. 2007;51:659–675.
- Vanable ED, LoPresti LR. Using Dental Materials. Upper Saddle River, NJ: Pearson Prentice Hall. 2003.
- Lainovic T, Vilotic M, Blazic L, Kakas D, Markovic D, Ivanisevic A. Determination of surface roughness and topography of dental resin-based nanocomposites using AFM analysis. Bosn J Basic Med Sci. 2013;13:34–43.
- Calley KH. Maintaining the beauty and longevity of esthetic restorations. Dimensions of Dental Hygiene. 2009;7(6):38–41.
- Powers JM, Sakaguchi RL. Craig’s Restorative Dental Materials. 12th ed. St. Louis: Mosby Elsevier; 2006:191.
- Bird DL, Robinson DS. Modern Dental Assisting. 10th ed. Philadelphia: Saunders; 2011:680-695.
- Kosmac T, Dakskobler A, Oblak C, Jevnikar P. The strength and hydrothermal stability of Y-TZP ceramics for dental applications. International Journal of Applied Ceramic Technology. 2007;4(2):164–174.
- Buchgraber B, Kqiku L, Allmer N, Jakopic G, Stadtler P. Surface roughness of one nanofill and one silorane composite after polishing. Coll Antropol. 2011;35:879–883.
- Rathore M, Singh A, Pant V. The dental amalgam toxicity fear: A myth or actuality. Toxicol Int. 2012;19:81–88.
- Al-Samhan A, Al-Enezi H, Alomari Q. Clinical evaluation of posterior resin composite restorations placed by dental students of Kuwait University. Med Princ Pract. 2010;19:299–304.
- Kitayama S, Nikaido T, Ikeda M, Alireza S, Miura H, Tagami J. Internal coating of zirconia restoration with silica-based ceramic improves bonding of resin cement to dental zirconia ceramic. Biomed Mater Eng. 2010;20:77–87.
- Nakamura Y, Sato H, Ohtsuka M, Hojo S. Polishing of dental porcelain by polycrystalline diamond. Biomed Mater Eng. 2010;20:283–293.
- Graumann SJ, Sensat ML, Stoltenberg JL. Air polishing: a review of current literature. J Dent Hyg. 2013;87:173–180.
- Arabaci T, Cicek Y, Ozgoz M, Canakci CF, Eltas A. The comparison of the effects of three types of piezoelectric ultrasonic tips and air polishing system on the filling materials: an in vitro study. Int J Dent Hyg. 2007;5:205–210.
- Vitalariu AM. Effect of surface polishing and glazing on the roughness of the dental acrylic resins. Available at: daaam.info/Downloads/Pdfs/ proceedings/proceedings_2010/17664_Annals_1_head.pdf. Accessed February 26, 2014.
- Jefferies SR. Abrasive finishing and polishing in restorative dentistry: A state-of-the art review. Dent Clin N Am. 2007;51:379-397.
- Darby ML, Walsh MM. Dental Hygiene Theory and Practice. 3rd ed. St. Louis: Saunders; 2009:512–522.
- Gladwin M, Bagby M. Clinical Aspects of Dental Materials. 4th ed. Baltimore: Lippincott Williams & Wilkins; 2012:185–191.
- Pelka MA, Altmaier K, Petschelt A, Lohbauer U. The effect of air-polishing abrasives on wear of direct restoration materials and sealants. J Am Dent Assoc. 2010;141:63–70.
- Penugonda B, Settembrini L, Scherer W, Hittelman E. Alcohol-containing mouthwashes: Effect on composite hardness. J Clin Dent.1994;5:60–62.
- Celik C, Yuzugullu B, Erkut S, Yamanel K. Effects of mouth rinses on color stability of resin composites. Eur J Dent. 2008;2: 247–253.
- Gurgan S, Yalcin Cakir FY. The effect of three different mouthrinses on the surface hardness, gloss and colour change of bleached nano composite resins. Eur J Prosthodont Restor Dent. 2008;16:104–108.
- Rantanen M, Johansson K, Honkala E, Leino-Kilpi H, Saarinen M, Salantera S. Dental patient education: a survey from the perspective of dental hygienists. Int J Dent Hyg. 2010;8:121–127.
From Dimensions of Dental Hygiene. March 2014;12(3):63–67.


 DURABILITY
DURABILITY
