Is Double Gloving Advantageous?
We explore the ongoing debate over the efficacy of double gloving in infection control.
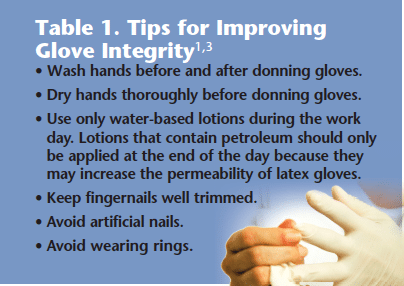
To ensure the safety of providers and patients, dental professionals must don personal protective equipment (PPE) when there is the possibility of occupational exposure to blood, bodily fluids, or other potentially infectious materials.1,2 Gloves are a vital component of PPE, and their widespread use among health care providers has dramatically reduced infection transmission in medical and dental settings. In order for gloves to provide protection, however, their integrity must not be compromised (Table 1).1,3 Although the rate of glove perforation during routine dental procedures is fairly low—between 4% and 8%—dental professionals may be unaware that their hand protection has been jeopardized.1,4-7 In medicine, particularly in the surgical setting, the wearing of two pairs of gloves (or double gloving) has been suggested to reduce the risk of exposure when glove perforation occurs.1,4,5,8,9
WHAT THE EVIDENCE SAYS
The body of research on double gloving in dentistry is small. A systematic review conducted by the Cochrane Collaboration looked at whether double gloving decreased the rate of infection among providers and patients, and whether double gloving reduced the risk of glove perforations of the innermost layer closest to the skin.10 The authors did not find enough compelling evidence that showed the use of double gloving decreased the incidence of infection at surgical sites, although there were too few studies conducted to fully support this theory. On the other hand, 31 studies were available that looked at glove perforation. The authors found that glove perforations to the innermost layer were reduced by 2% to 9% by double gloving.10
GLOVE TYPE![]()
The leakage rate of gloves varies by the type of material (latex, vinyl, or nitrile) used in their manufacture.1,4 Pitten et al11 researched the integrity of four types of nonsterile latex gloves in dental practice. After dental treatment, 847 gloves were tested for leakage. The duration of glove usage, as well hand disinfection practices, were recorded. Results revealed that gloves leaked up to 29% of the time. This number was increased by the use of alcohol-based hand sanitizer prior to donning gloves. The study concluded that the differences among leakage rates were based on the varying quality of the gloves tested and how dry the hands were before the gloves were donned. Higher quality gloves placed on thoroughly dry hands had the lowest rates of leakage.11 Dirschka et al6 microscopically evaluated the perforation rate of sterile, powder-free, surgical latex gloves after use.
Defects in the gloves were observed with the water inflation technique and through a microscope. Of the 660 gloves evaluated, 20 were found to have defects, and only five gloves showed visible signs of leakage. Most of the leakage occurred in gloves worn by the nondominant hand and when needles were used during the procedure.6
Some examination gloves may have pre-existing defects, compromising infection control efforts.5 Patel et al12 assessed pre-existing defects among five different nitrile examination gloves and two types of latex gloves by air inflation, followed by submersion in water to observe leakage indicated by air bubbles. Powdered latex gloves exhibited defects 3% of the time. On the other hand, three types of nitrile gloves were defect-free and only one type of nitrile gloves showed small holes.12 Glove leakage does occur, but there is insufficient evidence to show a direct link between glove perforation and cross-contamination or infection.10 Also, innovation in glove manufacturing continues to evolve. As the quality of medical gloves increases, the debate over double gloving’s efficacy may become moot.
TYPE OF PROCEDURE
Gloves should be selected based on the type of procedure to be performed. Studies on the glove perforation indication system suggest no benefit of double gloving during routine dental procedures.1,4,5,9 Avery et al9 researched the incidence of glove puncture among clinicians who double gloved vs those with single gloves during the dental treatment of 138 patients. Each time a glove perforation was observed, the gloves were inspected using the water inflation technique. Perforation was noticed in only four gloves. All tears occurred during restorative procedures when a drill or instrument was used. Three of the micropunctures were noticed in the double-gloved group, whereas one tear was noted in the single-gloved group. No additional benefit from double gloving was reported.9
When the use of double or triple gloving was evaluated during oral surgery and dental hygiene procedures, the leakage rate for gloves used by surgeons was higher than the rate for dental hygienists.5 The study also found that double gloving decreased the rate of cross-contamination.5
Another trial used the water inflation technique to examine the perforation rate of 420 sterile surgical gloves during the extraction of wisdom teeth. The rate of glove leakage was 2.1% per procedure. More than half of the glove defects went unrecognized by the operator.7 Baggett et al4 examined the rate of latex glove punctures using the water inflation technique after various dental procedures.
Endodontic therapy and crown preparation procedures resulted in the highest rate of defects, 7.5% and 6.3%, respectively. Dental scaling with the use of an ultrasonic insert or tip caused a 5% puncture rate. The glove puncture rate increased the longer the procedure lasted and when sharp instruments were used.4
DURATION OF USE
Although glove perforation rates increase when gloves are worn for a longer period of time,1,4,5,10 the rate of perforation varies. One study reported that glove perforation increased when gloves were worn longer than 2 hours.13 On the other hand, Patton et al5 found that the leakage rate for outer latex gloves was higher during procedures that extended beyond 45 minutes. Other studies have noted that gloves start to develop defects between 30 minutes to 3 hours of use.1,4,14 The quantity of bacteria found on the hands also increases when gloves are used for longer periods.10
Currently, there is no standard interval at which gloves should be changed, though the United States Centers for Disease Control and Prevention (CDC) recommends that gloves be changed when any tear or puncture is observed1 and after completing treatment with sharp instruments on high-risk patients.4 Gloves do provide an important barrier to infection but they can be compromised without the clinician’s knowledge, and therefore should be changed at regular intervals to minimize the possibility of cross-contamination.
CONCENSUS
Currently, the CDC does not recommend the use of more than one pair of gloves during routine dental procedures.1 Dental hygienists should assess the risks associated with a procedure and then decide whether double gloving may be a prudent choice. Wearing more than a single pair of gloves may be beneficial when completing high-risk procedures.9
Double gloving has been more thoroughly researched in the biomedical field.6,10,13,15 More studies must be conducted in dentistry to determine whether double gloving should be used in the dental setting.
REFERENCES
- Kohn WG, Collins AS, Cleveland JL, Eklund KJ, Malvitz DM. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52:1-61.
- United States Department of Labor, Occupational Safety and Health Administration. 29 CFR Part 1910. Occupational exposure to bloodborne pathogens; needlestick and other sharps injuries. Federal Register. 2001;66:5317-5325.
- Nicolay CR. Hand hygiene: an evidence-based review for surgeons. Int J Surg. 2006;4:53-65.
- Baggett FJ, Burke FJ, Wilson NH. An assessment of the incidence of punctures in gloves when worn for routine operative procedures. Br Dent J. 1993;174:412-416.
- Patton LL, Campbell TL, Evers SP. Prevalence of glove perforations during double-gloving for dental procedures. Gen Dent. 1995;43:22-26.
- Dirschka T, Winter K, Kralj N, Hofmann F. Glove perforation in outpatient dermatologic surgery. Dermatol Surg. 2004;30:1210-1213.
- Avery CM, Hjort A, Walsh S, Johnson PA. Glove perforation during surgical extraction of wisdom teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:23-25
- Burke FJ, Baggett FJ, Lomax AM. Assessment of the risk of glove puncture during oral surgery procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:18-21.
- Avery CME, Gallagher P, Birnbaum W. Double gloving and a glove perforation indication system during the dental treatment of HIV positive patients: are they necessary? Br Dent J. 1999; 186:27-29.
- Tanner J, Parkinson H. Double gloving to reduce surgical cross-infection. Cochrane Database Syst Rev. 2006;3:CD003087.
- Pitten FA, Herdemann G, Kramer A. The integrity of latex gloves in clinical dental practice. Infection. 2000;28:388-392.
- Patel HB, Fleming GJP, Burke FJT. A preliminary report on the incidence of pre-existing pinhole defects in nitrile dental gloves. Br Dent J. 2003; 195:509-512.
- Misteli H, Weber WP, Reck S. Surgical glove perforation and the risk of surgical site infection. Arch Surg. 2009;144:553-558.
- Otis LL, Cottone JA. Prevalence of perforations in disposable latex gloves during routine dental treatment. J Am Dent Assoc. 1989;118:321-324.
- Phillips S. The comparison of double gloving to single gloving in the theatre environment. J Perioper Pract. 2011;21:10-15.
From Dimensions of Dental Hygiene. December 2011; 9(12): 22, 24.