 MANJURUL / ISTOCK / GETTY IMAGES PLUS
MANJURUL / ISTOCK / GETTY IMAGES PLUS
Insight into Chronic Kidney Disease
Oral health professionals need to be aware of the oral implications of this serious disease.
This course was published in the October 2022 issue and expires October 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define chronic kidney disease (CKD).
- Describe the diagnostic process for CKD.
- Identify the oral manifestations of CKD and treatment strategies.
Chronic kidney disease (CKD) is the progressive loss of kidney function due to cumulative damage.1 In the United States, approximately 37 million adults, or one in seven, have CKD, with nearly 90% of those cases remaining undiagnosed.2,3 Socioeconomic status, race and ethnicity, lifestyle choices, and other systemic diseases all impact the incidence of CKD and end stage renal disease (ESRD).
Studies show that individuals of lower socioeconomic status have a higher incidence of CKD.4 Moreover, Black individuals are four times more likely to develop CKD than white individuals. Black Americans also have a higher prevalence of diabetes and hypertension, which both lead to CKD.2
Lifestyle choices can influence the probability of CKD or ESRD. Unhealthy diet and physical inactivity are among the key modifiable risk factors for chronic conditions. Diabetes and high blood pressure are the most common causes of CKD in the US.5
High blood pressure, swelling in the hands or feet, and blood in the urine are three early signs of CKD.6 Oral health professionals often assess and record blood pressure for all patients, providing an opportunity for referral if results are outside of the normal range. Patients are commonly referred for primary hypertension or essential hypertension, which accounts for about 95% of high-blood pressure cases.7 However, secondary hypertension is associated with undiagnosed chronic systemic conditions such as CKD.
Physiology of Kidneys
The kidneys control acid-base balance, water balance, electrolyte maintenance, toxin and waste product removal, blood pressure, production of the hormone erythropoietin, and activation of vitamin D.8 Kidneys maintain and regulate sodium, potassium, phosphorus, calcium, and magnesium. Failure to filter out excess sodium contributes to hypertension and insulin resistance, which impacts urine output. Thus, one of the earliest signs of undiagnosed kidney disease is high blood pressure. An imbalance of potassium can lead to hyperkalemia, raising the risk for cardiac arrhythmia.9–11 Decreased kidney function affects activation of vitamin D and the absorption of calcium, which may signal the parathyroid hormone. Increased levels of parathyroid can lead to osteoporosis, gastralgia, and asthenia. Imbalance of minerals can cause bone demineralization of the jaw, decreased trabeculation, and reduced thickness of cortical bone, all of which would cause complications affecting osteointegration of dental implants, periodontal disease risk, and increased likelihood of jaw fracture.12
Diagnosis
Routine blood and urine testing is important to diagnose CKD and assess the stage of disease progression. Blood tests are used to evaluate serum creatinine levels, glomerular filtration rate (GFR), and blood urea nitrogen (BUN).13,14 GFR measures kidney function and creatinine levels, whereas BUN tests measure the amount of urea nitrogen and the breakdown of protein in foods. Urine tests evaluate urinalysis, protein, microalbuminuria, and albumin-to-creatinine ratio. In stage 3 of CKD, individuals present with signs and symptoms, including fatigue, nausea, loss of appetite, fluid retention, shortness of breath, muscle cramps, and dark urine.15
Preliminary research shows that measuring the level of creatinine in saliva may provide an early diagnostic tool for CKD.16 Salivary creatinine concentrations above 8.5 umol/L indicate the need for referral to a healthcare provider for additional testing.16,17 Saliva testing may help diagnosis CKD early, before clinical symptoms occur.
The dental management of patients with CKD is based on their stage in the disease process (Table 1). CKD has five stages classified by a patient’s GFR. A GFR of 60 or higher is in the normal range. A GFR below 60 may mean kidney disease. A GFR of 15 or lower indicates kidney failure. In stages 1 and 2, many individuals do not experience any changes in their overall health. Moderate kidney damage is present at stage 3 and has two substages: 3a (45 mL/min to 59 mL/min GFR) and 3b (30 mL/min to 44 mL/min GFR).15 In addition to the clinical symptoms of stage 3, patients may report a metallic taste, oral malodor, difficulty concentrating, and numbness in toes and fingers.15 In stage 4, the kidneys display moderate to advanced damage, signalling that patients will need dialysis and/or a kidney transplant. Stage 5 of CKD is referred to as ESRD, meaning there is need for long-term dialysis or a kidney transplant in order to maintain life.18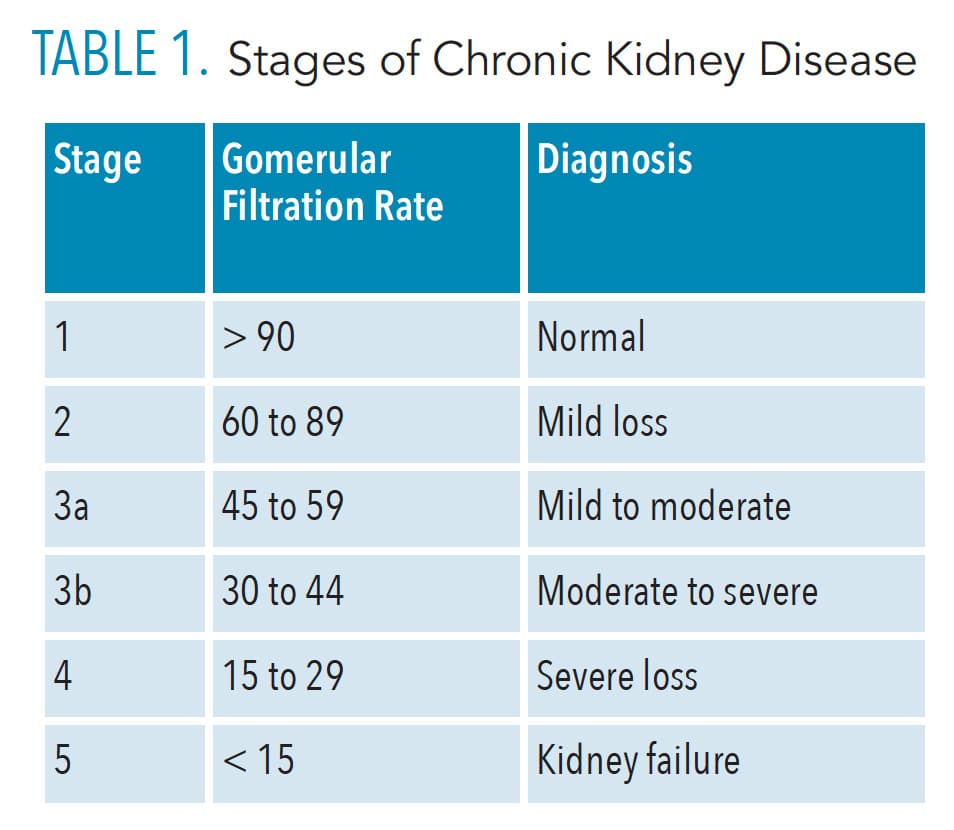
Medical Management
For patients with ESRD, treatment includes hemodialysis, peritoneal dialysis, and kidney transplant. Hemodialysis is scheduled three times/week at a hospital or dialysis center and the process requires 3 hours to 4 hours. Individuals undergoing hemodialysis must abide by strict dietary restrictions regarding the consumption of fluid, phosphorus, potassium, and sodium. This population often experiences xerostomia due to fluid restrictions, and oral malodor because of reduced salivary flow, increasing their risk for mucosal lesions, such as candidiasis and dental caries, as well as alveolar bone loss and periodontal diseases.19 Peritoneal dialysis removes waste products from the blood.20 A catheter is placed in the abdomen, and treatment takes approximately 8 hours to 10 hours per day.20 Patients awaiting a kidney transplant often have an alkaline oral pH, causing increased accumulation of dental calculus.
Children with CKD may present with developmental defects of the enamel, tooth staining, stomatitis, gingivitis, gingival overgrowth, oral malodor, xerostomia, and dysgeusia.21,22 Among children with CKD, 31% to 83% will experience enamel hypoplasia due to their need for corticosteroid and tetracycline medications. Developmental defects of enamel increase the risk of caries and, as such, parents/caregivers must be educated on appropriate dietary choices and effective oral hygiene.
Pharmacology
The vast majority of prescribed medications and supplements are either metabolized by the kidneys or the liver. Medications that are nephrotoxic, or those that may decrease renal blood flow, are contraindicated for patients with CKD.23 If medications that are metabolized/excreted by the kidneys must be prescribed, their dosages and intervals may need to be adjusted.
In regards to dental pain management for patients with CKD, acetaminophen should be recommended. Based on the patient’s GFR, the dosing interval may need to be increased. Nonsteroidal anti-inflammatory drugs should be avoided, or the dosage reduced in patients with advanced renal failure due to their nephrotoxic and hypertensive effects.24 For patients with CKD who have uremia, a condition in which high levels of urea is in the blood, aspirin should also be avoided because it will increase the risk of bleeding.
When treating an infection, the standard doses of penicillin, clindamycin, and cephalosporin may be administered at prolonged dosing intervals as needed. Dosage reductions are typically proportional to the degree of renal insufficiency.23 Clinicians should consult with the patient’s nephrologist prior to treatment.25
Gingival enlargement is common among patients with CKD due to their taking cyclosporine or calcium channel blockers. Cyclosporine is prescribed to help prevent acute rejection and the loss of the renal allograft. The calcium channel blockers are prescribed for patients with CKD-related hypertension. Dental lasers can be used to remove excess gingival tissue. Oral health professionals should inform a patient’s primary care provider about the presence of gingival enlargement in the hopes that alternative medications can be prescribed. If this is not possible, patients should be scheduled for more frequent recare intervals.
Patients with CKD who are receiving long-term adrenal-suppressive doses of corticosteroids may need additional prednisone before stressful, lengthy, or invasive surgical procedures. The amount of prednisone necessary depends on the degree of suppression along with the length and invasiveness of the surgery itself.26 For example, procedures involving multiple extractions, bony impactions, periodontal surgery, bone resections, osteotomies, or any surgical procedure lasting longer than 1 hour should be supplemented with 10 mg to 20mg of prednisone the day of the surgery and for at least 1 day post-operatively.26
Oral Manifestations
Intraoral changes may occur in patients with CKD, such as uremic stomatitis, xerostomia, taste alterations, mucosal petechiae, ecchymosis, renal osteodystrophy, and periodontal diseases.15,27 During routine dental visits, oral health professionals may note signs of undiagnosed CKD, such as uremic stomatitis, which is typically associated with untreated chronic renal failure. A painful lesion caused by elevated levels of urea nitrogen in the blood, uremic stomatitis may manifest as four forms: ulcerative, hemorrhagic, nonulcerative, and hyperkeratotic. It may present with red mucosal ulcers or thick gray exudate covering the oral mucosa. Nonulcerative and hyperkeratotic types appear as white lesions. Hyperkeratotic lesions are more often found around the tongue and floor of the mouth. The pain associated with uremic stomatitis may be managed by using a mildly acidic mouthrinse, such as diluted hydrogen peroxide; sucking on ice chips; or applying topical anesthetics.15
Xerostomia and taste alterations commonly seen in patients with stage 4 CKD are due to increased uremic levels in the salivary glands, which causes an ammonia-smelling odor or metallic taste due to the increased pH level. Petechiae and ecchymosis are caused by a decrease in platelet factor III, and are often found on the soft palate, tongue, and buccal/labial mucosa.15,27 Oral candidiasis affects 20% to 30% of patients with kidney transplants, and may be treated with topical antifungals, nystatin, miconazole, gentian violet, and amphotericin B.15
Renal osteodystrophy is a bone disease that occurs when the kidneys are unable to maintain proper levels of calcium, phosphorus, and vitamin D, and may arise from parathyroid malfunction.15 Renal osteodystrophy causes “brown tumors” and loss of the lamina dura. In adults and children, renal osteodystrophy appears on Xrays as a ground glass appearance. It may lead to delayed tooth eruption, severe periodontal destruction, and tooth mobility.15
Role of the Dental Hygienist
Oral hygiene instruction should be emphasized pre- and post-kidney transplant. Pre-transplant individuals are more prone to dry mouth and increased calcium due to the presence of uremia in their saliva. Prior to a kidney transplant, dental clearance should be obtained first and any teeth with a poor prognosis or periodontal abscess should be extracted.21 After the kidney transplant, individuals are at an increased risk of dental caries and gingival enlargement due to their medication use. Oral hygiene instructions must be provided to reduce potential caries and oral infections and with specific strategies on how to decrease calculus accumulation. Ninety percent of patients with CKD experience one or more of the following oral health problems: xerostomia, oral malodor, uremic stomatitis, mucositis, and glossitis.28 Fluoride toothpastes, oral rinses, and fluoride application should be recommended. Oral health professionals should be cautious to prescribe systemic fluoride supplements to children with CKD because kidney impairment may cause fluoride retention.21 Dentists and dental hygienists can use caries risk assessment to assess, manage, and select appropriate therapeutic aids for patients with CKD.
Progression of periodontitis in patients with CKD is based on host, environmental, and bacteriological factors.28 Patients with CKD have a higher concentration of urea, sodium, and phosphate in addition to a decreased salivary rate and buffering capacity. Reduced saliva flow increases the risk for calculus buildup, caries, and periodontal diseases.29 Individuals with CKD may have loose or painful teeth due to their inability to absorb calcium properly.30 Oral health professionals should recommend nonsurgical periodontal therapy to reduce the bacterial load and reduce inflammation, while monitoring bone levels and periodontal pockets.28
Dental providers need to be mindful of oral lesions, taste changes, and xerostomia linked to CKD or ESRD. Blood pressure screenings can improve patients’ awareness of their overall health and enable clinicians to make proper referrals to address kidney concerns. Early diagnosis of CKD is key to reducing the risk for further kidney damage and to providing a wider variety of treatment options. For patients undergoing dialysis, dental treatment should be provided the day after dialysis. Premedications are given after recommendation by the patient’s physician or according to the American Heart Association guidelines.
For all patients, prevention is always best, which includes baseline screenings, dietary counseling, and tobacco cessation. Dental hygienists can educate their patients on eating nutrient-rich foods and discuss the importance of exercise to help them achieve overall health.
Conclusion
Interdisciplinary collaboration between dental and medical providers supports early diagnoses, proper treatment, and better outcomes in those with CKD. As patients often visit their oral health professionals more frequently than their primary care provider, they may be the first to note signs of CKD, helping patients achieve the best possible outcomes.
References
- National Institute of Diabetes and Digestive and Kidney Diseases. What Is Chronic Kidney Disease? Available at: niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease ckd#: ~:text=%E2%80%8B%E2%80%8BWhat%20Is%20Chronic,family%20history%20of%20kidney%20failure. Accessed September 27, 2022.
- Brown JS. Addressing the issue: health disparities and social determinants of health among Blacks/African Americans in comparison to non-minorities with chronic kidney disease. Nephrol Nurs J. 2021;48:489.
- United States Centers for Disease Control and Prevention. Chronic Kidney Disease Basics. Available at: cdc.gov/kidneydisease/basics.html. Accessed September 26, 2022.
- Brown JS, Elliott RW. Social determinants of health: understanding the basics and their impact on chronic kidney disease. Nephrol Nurs J. 2021;48:131.
- Proctor R, Kumar N, Stein A, Moles D, Porter S. Oral and dental aspects of chronic renal failure. J Dent Res. 2005;84:199–208.
- American Kidney Fund. All About Kidneys. Available at: kidneyfund.org/all-about-kidneys. Accessed September 26, 2022.
- Carretero OA, Oparil S. Essential hypertension, part I: definition and etiology. Circulation. 2000;101:329–335.
- National Institute of Diabetes and Digestive and Kidney Diseases. Your kidneys & how they work. Available at: niddk.nih.gov/health-information/kidney-disease/kidneys-how-they-work. Accessed September 26, 2022.
- Simon LV, Hashmi MF, Farrell MW. Hyperkalemia. Treasure Island, Florida: StatPearls Publishing; 2022.
- Lerma E. Approach to the patient with renal disease. Prim Care. 2008;35:183–194.
- Pun PH, Smarz TR, Honeycutt EF, Shaw LK, Al-Khatib SM, Middleton JP. Chronic kidney disease is associated with increased risk of sudden cardiac death among patients with coronary artery disease. Kidney Int. 2009;76:652–658.
- Kanjevac T, Bijelic B, Brajkovic D, Vasovic M, Stolic R. Impact of chronic kidney disease mineral and bone disorder on jaw and alveolar bone metabolism: a narrative review. Oral Health Prev Dent. 2018;16:79–85.
- Renal blood flow and glomerular filtration. In: Eaton DC, Pooler JP, eds. Vander’s Renal Physiology. 8th ed. New York: McGraw Hill; 2016.
- III JLL. Overview of acid-base balance—hormonal and metabolic disorders. Available at: merckmanuals.com/home/hormonal-and-metabolic- disorders/acid-base-balance/overview-of-acid-base-balance. Accessed September 26, 2022.
- Ravisankar A, Selvarasu K. Oral and maxillofacial manifestations of chronic kidney diseases—a review. Drug Invention Today. 2020;13(6):868–873.
- Temilola DO, Bezuidenhout K, Erasmus RT, et al. Salivary creatinine as a diagnostic tool for evaluating patients with chronic kidney disease. BMC Nephrol. 2019;20:387.
- Goldman L, Schafer AI, Cecil RL. Goldman-Cecil Medicine. Philadelphia: Elsevier/Saunders; 2016.
- Centers for Medicare & Medicaid Services. End-stage renal disease (ESRD). Available at: cms.gov/Medicare/Coordination-of-Benefits-and-Recovery/Coordination-of-Benefits-and-Recovery-Overview/End-Stage-Renal-Disease-ESRD/ESRD. Accessed September 26, 2022.
- López-Pintor RM, López-Pintor L, Casañas E, de Arriba L, Hernández G. Risk factors associated with xerostomia in haemodialysis patients. Med Oral Patol Oral Cir Bucal. 2017;22:e185–e192.
- National Kidney Foundation. What is peritoneal dialysis? Available at: kidney.org/content/what-peritoneal-dialysis. Accessed September 26, 2022.
- Velan E, Sheller B. Oral Health in children with chronic kidney disease. Pediatr Nephrol. 2021;36:3067–3075.
- National Institute of Diabetes and Digestive and Kidney Diseases. Growth Failure in Children with Chronic Kidney Disease. Available at: niddk.nih.gov/health-information/kidney-disease/children/caring-child-kidney-disease/growth-failure-chronic-kidney-disease. Accessed September 26, 2022.
- Brockmann W, Badr M. Chronic kidney disease: pharmacological considerations for the dentist. J Am Dent Assoc. 2010;141:1330–1339.
- Whelton A. Nephrotoxicity of nonsteroidal anti-inflammatory drugs: physiologic foundations and clinical implications. Am J Med. 1999;106:13S–24S.
- Patton LL, Glick M, eds. The ADA Practical Guide to Patients with Medical Conditions. Hoboken, New Jersey: John Wiley & Sons Inc; 2015.
- Miller CS, Little JW, Falace DA. Supplemental corticosteroids for dental patients with adrenal insufficiency. J Am Dent Assoc. 2001;132:1570–1579.
- Kho HS, Lee SW, Chung SC, et al. Oral Manifestations and salivary flow rate, pH, and buffer capacity in patients with end renal disease undergoing hemodialyis. Oral Surg Oral Med Oral Pathol Ora Radiol Endod. 1999;88:316–319.
- Parsegian K, Randall D, Curtis M, Ioannidou E. Association between periodontitis and chronic kidney disease. Periodontol 2000. 2022;89:114–124.
- Rodrigues RPCB, Vidigal MTC, Vieira WA, et al. Salivary changes in chronic kidney disease and in patients undergoing hemodialysis: a systematic review and meta-analysis. J Nephrol. 2002;35:1339–1367.
- Soroye MO, Ayanbadejo PO. Oral conditions, periodontal status and periodontal treatment need of chronic kidney disease patients. Journal of Oral Research and Review. 2016;8(2):53.
From Dimensions of Dental Hygiene. October 2022; 20(10)38-41.



