Increase Your Cultural Competence
How to improve communication with a culturally diverse patient population.
This course was published in the November 2011 issue and November 2014. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define cultural competence.
- Discuss barriers faced by minority populations in accessing care.
- Identify strategies to improve patient-provider communication.
- Explain the importance of cultural competence.
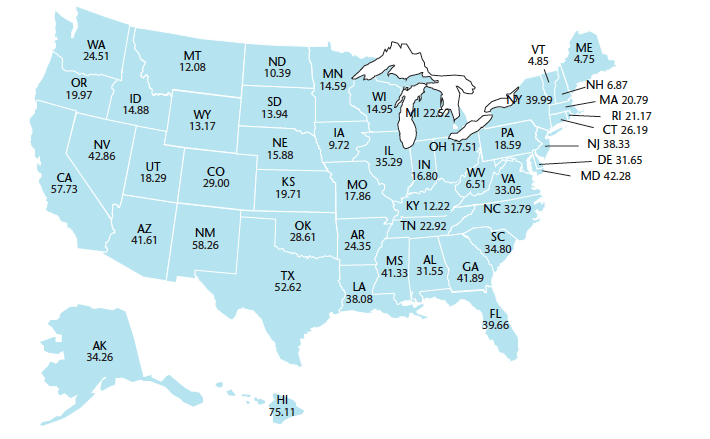
The United States is growing more diverse—more than one-third of the country’s total population is now part of a minority group, with Hispanics comprising the fastest growing segment (Figure 1).1 By the year 2050, ethnic groups will make up 48% of the US population.2 This diversity requires health care providers, including dental professionals, to become more culturally competent in order to effectively treat the patients of today and tomorrow. Dental professionals must be prepared to handle issues involving patient and provider communication, in addition to the different beliefs and attitudes about oral health held by people of other cultures.3
According to Garcia et al, cultural competence is defined as “an understanding of the importance of social and cultural influences on patients’ health beliefs and behaviors; considering how these factors interact at multiple levels of the health care delivery system; and, finally, devising interventions that take these issues into account to assure quality health care delivery to diverse patient populations.”3 Oral health care providers can increase their cultural competence by becoming more knowledgeable about the cultural preferences of their patients while resisting stereotypes. Patients’ behaviors are often intertwined with their cultural beliefs and experiences, yet each person is an individual and should be treated as such.4
Barriers to Oral Health Care Faced by Minority Populations
Minority patients, including African Americans, Hispanics, and American Indians/Alaska natives, often experience barriers to receiving oral health care (Table 1). Little or no access to professional oral health care services can have dire consequences, including: increased risk of edentulism, higher incidence of systemic disease, reduced life expectancy, lower quality of life, and limited access to economic opportunity.4 A recent survey of the oral health of Native Americans living on the isolated Pine Ridge Indian Reservation, where most of its 40,000 residents have no access to dental care, found that almost the entire population surveyed had some degree of tooth decay, 68% had signs of periodontal disease, and four out of 10 children were at risk of systemic health complications due to oral disease.5
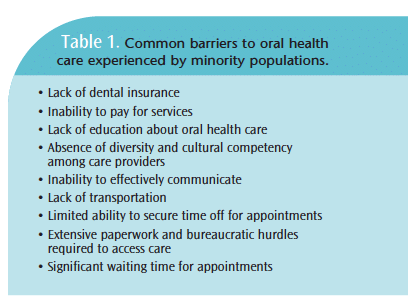 People of different cultures may not fully understand the importance of preventive oral health measures or they may not be confident in current practices or providers of care.6 Oral health care providers must be aware of these barriers so they can be overcome.7 For patients of different ethnicities, access to oral health care may be geographically close, but culturally distant. Different racial and/or ethnic groups have their own beliefs and behaviors, which can lead to varying levels of oral health among populations. Such multicultural differences are often associated with demographic and religious characteristics.
People of different cultures may not fully understand the importance of preventive oral health measures or they may not be confident in current practices or providers of care.6 Oral health care providers must be aware of these barriers so they can be overcome.7 For patients of different ethnicities, access to oral health care may be geographically close, but culturally distant. Different racial and/or ethnic groups have their own beliefs and behaviors, which can lead to varying levels of oral health among populations. Such multicultural differences are often associated with demographic and religious characteristics.
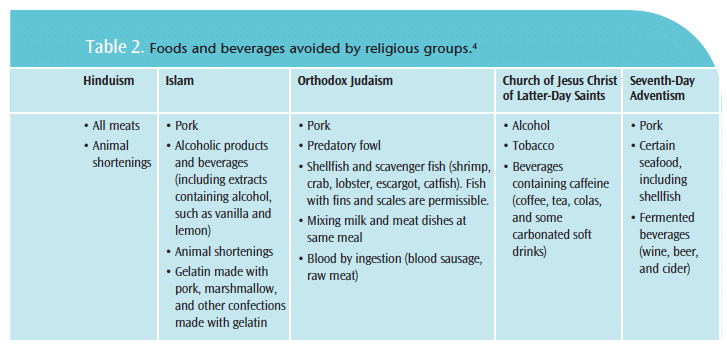
Patients with religious beliefs that do not coincide with standard oral health care could result in a strain on the patient provider relationship. For example, patients of the Islamic faith avoid gelatin, an ingredient in many dental products. A patient may be offended if an oral health care provider unknowingly tries to use a product containing gelatin. Cultural religious beliefs can become barriers to oral health assessment, treatment planning, and overall health of the patient. It is unrealistic to expect oral health care providers to be proficient in all cultures; however, knowledge of religious beliefs may help facilitate care (Table 2).4,8
Cultural conflicts between patients and providers may manifest as inconsistent behavior and compliance issues. Dental professionals who are unskilled in cultural competence may inadvertently create a feeling of distrust between provider and patient.
![]() Patient-Provider Communication
Patient-Provider Communication
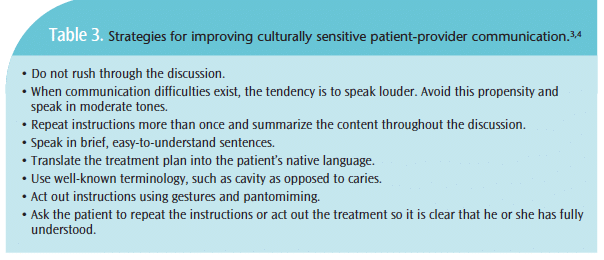
Oral health care providers need to educate patients in a culturally suitable manner that addresses patient needs, capabilities, and willingness to comply. Communication is a broad term and includes the way clinicians interact through written or oral language, gestures, facial expressions, body language, space, or other symbols.9
Patients from different cultures may present with language and communication barriers that inhibit the development of effective treatment plans. Language barriers can cause a great deal of anxiety for patients who are apprehensive about oral health care, making the provision of appropriate care difficult. Even when a translator is available, subtle differences in the meaning of words can be lost, causing misunderstandings. This is particularly true among Hispanic populations, because more than 50 distinct dialects exist under the broad umbrella of Spanish.9
Oral health care providers must try to understand the patient’s viewpoint, treating him or her as an individual in order to accurately diagnose the condition and ensure compliance with treatment. Building trust with a culturally diverse patient population is essential to a successful provider-patient relationship. Culturally competent care providers take the time to gather all relevant information from patients, discuss diagnosis and treatment plans, respect their point of view, and come to mutual agreement on additional treatment.10
Language and communication barriers can have serious effects, such as the provision of ineffective treatment, misdiagnosis, incorrect drug prescription dosages, and reduced patient compliance. Failing to consider the cultural restraints of a particular ethnic group, to interface in a culturally sensitive manner, or to appropriately communicate with any patient increases the risk of these problems.11
Additional Strategies for Increasing Cultural Competency
Awareness of and sensitivity to patients’ cultural differences, ethnic backgrounds, and religious beliefs will benefit dental professionals in their mission to provide the most effective care, as well as encourage patients to follow treatment plans and return for continued oral health maintenance. Western societies have their own cultural beliefs that are exhibited during the provision of health care. For example, in Western cultures, eye contact is a sign of attentiveness and self-confidence. In other cultures, such as Hispanic, Asian, Middle Eastern, and Native American, eye contact may be considered rude. Women may refrain from making eye contact with male providers because their culture views it as a sign of sexual interest.12
Western societies are typically very tactile, but touch may have different meanings among other cultures. Some cultures view touch as healing (Native American), while others may forbid the touching of certain parts of the body. For example, many Southeast Asians believe that the head houses the soul, thus the innocuous pat of a child’s head may be viewed as an insult.13
Personal space requirements are influenced by culture and specific to individuals. People in Western countries tend to prefer a certain amount of personal space while people of other ethnicities, such as Hispanics, may view close proximity as a sign of friendliness.14 Clinicians need to be attuned to patients’ signals, such as averting eye contact or trying to recoil, that signal a need for additional space.
IMPORTANCE OF CULTURALLY COMPETENT CARE
Cultural competence is necessary to provide sensitive, empathetic, and humanistic care that is respectful of patients and responds to patients’ psychosocial needs.15 Oral health care providers must adapt frameworks to improve the provision of care to all patients.16
Recognizing that quality patient care depends on the provider’s ability to meet the cultural needs of diverse patient populations is the first step toward cultural competence. Patients will value the patient-provider relationship if they feel their cultural needs are appreciated and respected. Oral health care providers need to identify the patient’s physical, mental, and cultural needs within the context of their cultural environment. Patient perceptions have become increasingly accepted as important and valid measures of health care quality.17 A patient who is satisfied with the care provided is more likely to comply with treatment.
Pioneering oral health care settings have found that diversity and cultural competence initiatives can improve the quality of care.18 When multiculturalism and diversity are handled efficiently and successfully, the patient provider relationship is strengthened. Oral health care providers must effectively incorporate the cultural diversity of patients into the assessment of their treatment plan and care. Cross-cultural oral health care recognizes and encompasses the social, political, ethnic, religious, and economic realities that shape the experiences and environments of the patient population. These factors must be recognized and integrated into professional care if preventive and therapeutic goals are to be achieved.19
Research has shown that successful patient-provider communication is associated with patient satisfaction, adherence to oral health instructions, and positive health outcomes. Oral health care providers should become well versed in patient-centered care and cultural competence in order to improve quality and eliminate cultural disparities in oral health care.20
Patient demographics, satisfaction, and quality care are important components of a successful oral health care strategy.18 All individuals have their own expectations, backgrounds, values, and preferences that may affect the way they interact with health care professionals. Oral health care providers who are sensitive to cultural differences are on the right track to increasing patient satisfaction, improving processes and outcomes of care, and minimizing conflict between oral health practices and diverse patient cultures.18
CONCLUSION
The cultural identity of each patient should not be overlooked or disregarded, but rather preserved and respected. Oral health care providers educated in cultural competence can increase patient compliance with treatment plans, improve overall results, and enhance patient-provider relationships.
REFERENCES
- US Census Bureau. 2010 Census Briefs. Available at: www.census.gov/population/www/cen2010/democen2010.html. Accessed October 18, 2011.
- US Census Bureau. US Population Projections. Available at: www.census.gov/population/www/projections/ppl47.html. Accessed October 18, 2011.
- Garcia RI, Cadoret C, Henshaw M. Multicultural issues in oral health. Dent Clin North Am. 2008;52:319–326.
- Understanding transcultural nursing. Nursing. 2005;35 Suppl:14–18.
- Batliner T. An assessment of oral health on the Pine Ridge Reservation. Paper presented at: 68th Annual National Congress of American Indians; Portland, Ore: October 30, 2011.
- Sherer J. Crossing cultures: Hospitals begin breaking down the barriers to care. Hospitals. 1993;67(10):29–31.
- Azevedo D. A group dedicated to ethnic health care. Med Econ. 1995;72:87–91.
- Angelucci P. Cultural diversity: health belief system. Nurs Manage. 1995;26:72.
- Davidhizar R, Bechtel G, Giger J. A model to enhance culturally competent care. Hosp Top. 1998;76:22–26.
- Chesanow N. The versatile doctor’s guide to ethnic diversity. Med Econ. 1998;7:135–143.
- The changing face of health care consumers: multicultural marketing in an evolving world. Mark Health Serv. 2001;21:4–10.
- Vermont Department of health. Cultural differences in nonverbal communication. Available at: http://healthvermont.gov/family/toolkit/tools%5CF-6%20Cultural%20Differences%20in%20Nonverbal%20Communic.pdf. Accessed November 3, 2011.
- Jenko M, Moffitt SR. Transcultural nursing principles. J Hosp Palliat Nurs. 2006;8:172–180.
- Giger JN, Davidhizar RE. Transcultural Nursing: Assessment and Intervention. 4th ed. St Louis: Mosby; 2004.
- Fox R. Cultural competence and the culture of medicine. N Engl J Med. 2005;353:1316–1320.
- Mitchell D, Lassiter S. Addressing health care disparities and increasing workforce diversity: The next step for the dental, medical and public health professions. Am J Public Health. 2006;96:2093–2097.
- Blendon R, Buhr T, Cassidy E, et al. Disparities in health: perspectives of a multi-ethnic, multiracial America. Health Aff. 2007;26:1437–1447.
- Dreachslin J, Myers V. A systems approach to culturally and linguistically competent care. J Healthc Manag. 2007;52:220–226.
- Darby M, Walsh M. Dental Hygiene: Theory and Practice. 3rd ed. St. Louis: Saunders Elsevier; 2010:1276.
- Betancourt J, Green A, Carrillo J, Park E. Cultural competence and health care disparities: key perspectives and trends. Health Affairs. 2005;24:499–505.
From Dimensions of Dental Hygiene. November 2011; 9(11): 78-81.


 Patient-Provider Communication
Patient-Provider Communication
