 EDWARDOLIVE/ISTOCK/GETTY IMAGES PLUS
EDWARDOLIVE/ISTOCK/GETTY IMAGES PLUS
Improving the Safety of Dental Unit Waterlines
Treating the dental unit water, flushing the air/waterlines between patients, regular testing of water quality, and following all manufacturer instructions will help dental practices effectively maintain their dental unit waterlines.
Adhering to proper infection control protocols is critical to the safe practice of oral health care. The goal of infection control in dentistry is to minimize or eliminate exposure of patients, oral health professionals, and community members to any potentially harmful microorganisms. The maintenance of dental unit waterlines, including the quality of the water provided during dental treatment, is an integral aspect of infection control.
Ensuring the safety of dental unit waterlines is just as important as wearing gloves when providing treatment or sterilizing instruments. When dental unit waterlines are not appropriately maintained, disastrous consequences can occur.1–4 For example, 20 children who received pulpotomy treatments in the same Georgia dental clinic required hospitalization due to Mycobacterium abscessus infections in 2015.4 Untreated dental unit waterlines were the source of the bacterial contamination. In 2016, more than 50 children who received pulpotomy procedures were exposed to M. abscessus via the dental unit water in a pediatric dental clinic in Anaheim, California, causing severe infections that required hospitalization.3 As a result, new legislation was signed into law in 2017 by California’s Governor, Jerry Brown, that mandates the Dental Board of California to revise the minimum standards for infection control.5 Now, the water used for dental irrigation must be sterile or encompass disinfecting/antibacterial properties when administered during procedures that expose dental pulp.
While both of these examples are related to pulpotomies, every dental practice—regardless of the types of procedures performed—needs to ensure it is following best practices for maintaining dental unit waterlines.
WHAT’S IN THE WATER?
All untreated dental unit waterlines contain biofilm—an adhesive film of microorganisms that adhere to a variety of surfaces. During dental procedures, the low flows and the small tubing increase the likelihood that biofilm will flourish. These biofilm may contain such dangerous bacteria as Legionella pneumophila, Pseudomonas aeruginosa, and nontuberculous Mycobacterium.6 Due to the risks associated with dental unit waterline biofilm, dental practices must ensure the safety of dental unit waterline water by treating the unit water, flushing the air/waterlines between patients, regular testing of water quality, and following all manufacturer instructions.
Due to the high risk of biofilm formation in dental unit waterlines, the United States Centers for Disease Control and Prevention (CDC) recommends that dental unit water used in nonsurgical procedures adhere to the same standards released by the US Environmental Protection Agency (EPA) for drinking water, which is ≤ 500 colony forming units (CFU)/ml.7 A CFU is the measurement used to ascertain the number of viable bacteria, molds, and fungi in a liquid substance.8 Unfortunately, microbial counts in dental unit waterlines can rise quickly, easily reaching 200,000 CFU/ml and higher.9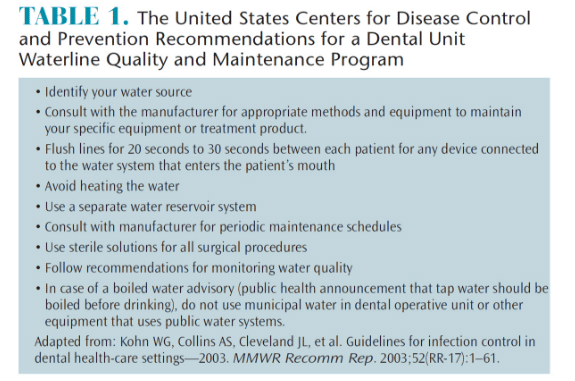
STRATEGIES TO ENSURE SAFETY
The EPA, American Public Health Association, and American Water Works Association all set standards to ensure safe drinking water.10,11 As stated previously, this standard is set at ≤ 500 CFU/ml. This same standard applies to water used as a coolant/irrigant in the dental setting for nonsurgical procedures. To deliver water of the recommended quality, dental practices need to employ systems or products that ensure the output water meets drinking water standards. Systems must also be regularly maintained and monitored, following all manufacturer instructions.7
A variety of options are available to dental practices to maintain water quality. Self-contained water reservoirs that are treated with chemical products either periodically or continuously are designed to maintain an acceptable water quality level and control the formation of biofilm. Point-of-use systems at the chair or full-practice systems filter source water and use a chemical disinfectant to control biofilm. A combination of both types of systems may be helpful.7 Independent water bottle systems alone are not enough to ensure water meets safe drinking water standards, nor is the use of distilled or sterile water in the water-output system. The use of chemicals or filters to remove or kill bacteria is necessary.7
Systems are either based on treatment cartridges that output disinfection chemicals or filters that eliminate particles found in the water. Affixed to the dental unit’s water bottle pickup tube, treatment cartridges must be replaced regularly according to manufacturer instructions, in order to maintain effectiveness. Typically installed on waterlines near the device (eg, handpiece or air/water syringe), filter systems remove microorganisms from the water before they pass into the dental instrument. In order to maintain efficacy, filters must be replaced at regular intervals according to manufacturer instructions. Some filter systems also incorporate a chemical disinfectant to protect against the formation of biofilm.11
Before beginning a chemical regimen, dental unit waterlines may need a shock treatment. Some systems may also require shock treatments at specific intervals. The treatment may be either continuous or intermittent, depending on the manufacturer instructions.11–13 Manufacturers are important allies in ensuring safe water. They can provide myriad information on the best systems to treat water in dental unit waterlines based on individual practice parameters. Only systems or products that are regulated by the EPA or the US Food and Drug Administration for dental unit waterline treatment should be used.11–13
The water used in dental units is not the only source of contamination. Microbes can enter the waterlines from patients’ mouths during treatment. Oral health professionals need to review manufacturer instructions to ensure that either their dental units prevent retraction of fluid or whether an anti-retraction valve is used, which would require regular maintenance to be effective.7 Flushing the water and air from devices—such as handpieces, ultrasonic units, and air/water syringes—for 20 seconds to 30 seconds after patient treatment is prudent to reduce the liklihood that patient material—such as blood or saliva—will enter the dental unit waterline.7 While mechanical flushing does little to reduce biofilms in dental unit waterlines, it may reduce the number of microbes temporarily and is valuable for removing free-floating contaminants in the water.6 Some treatment products that use continuous treatment do not require flushing. Table 1 provides a list of CDC recommendations for ensuring safe water.7
IMPORTANCE OF MONITORING
The only way to ensure a quality program is to test the water coming out of the unit. A well-designed water quality indicator should accurately detect a wide concentration range and type of aerobic mesophilic heterotrophic waterborne bacteria within a reasonable incubation time at room temperature. In addition to in-office testing kits, laboratories across the US also offer mail-in testing services. Oral health professionals should consult with the manufacturer of their water treatment systems to determine accurate testing modalities and appropriate intervals for testing.7
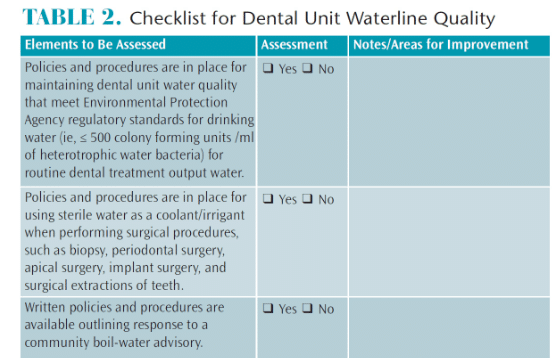
In addition, oral health professionals need to be well trained in water quality, biofilm formation, methods available to treat water, and appropriate maintenance protocols for the water system used in their specific office or clinic. Table 2 features the CDC’s checklist for ensuring safe dental unit waterline water.12
CONCLUSION
A comprehensive water treatment protocol for the office or clinic is imperative to proper infection control. Ongoing training and monitoring are key to ensuring safe water and minimizing risks to patients, clinicians, and equipment.
REFERENCES
- Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit waterline. Lancet. 2012;379:684.
- Peralta G, Tobin-D’Angelo M, Parham A, et al. Notes from the field. Mycobacterium abscessus infections among patients of a pediatric dentistry practice—Georgia, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:355–356.
- Rocha V. Orange County children’s dental clinic closed after bacteria found in new water system. Los Angeles Times.December 17, 2016.
- Peralta G, Tobin-D’Angelo M, Parham A, et al. Mycobacterium abscessus infections among patients of a pediatric dentistry practice—Georgia, 2015. MMWR Recomm Rep. 2016;65:355–356.
- California Dental Association. Infection control standards updated in new law. Available at: cda.org/news-events/infection-control-standards-updated-in-new-law. Accessed May 17, 2018.
- American Dental Association. Dental Unit Waterlines. Available at: ada.org/en/member-center/oral-health-topics/dental-unit-waterlines. Accessed May 17, 2018.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR-17):1–61.
- Goldman E, Green LH. Practical Handbook of Microbiology. 2nd ed. New York: Taylor and Francis; 2008.
- Barbeau J, Tanguay R, Faucher E, et al. Multiparametric analysis of waterline contamination in dental units. Appl Environ Microbiol. 1996;62:3954–3959.
- US Environmental Protection Agency. National Primary Drinking Water Regulations, 1999: List of Contaminants. Available at: epa.gov/safewater/mcl.html. Accessed May 17, 2018.
- Cuny EJ, Eklund KJ. Ensure the safety of dental treatment water. Dimensions of Dental Hygiene. 2017;15(3):37-42.
- Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Atlanta: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2016.
- United States Centers for Disease Control and Prevention. Dental Unit Water Quality. Available at: cdc.gov/oralhealth/infectioncontrol/questions/dental-unit-water-quality.html. Accessed May 17, 2018.
From Dimensions of Dental Hygiene. June 2018;16(6):18,20-21.

