 PURERADIANCEPHOTO/ISTOCK EDITORIAL/GETTY IMAGES PLUS
PURERADIANCEPHOTO/ISTOCK EDITORIAL/GETTY IMAGES PLUS
Addressing Prescription Opioid Misuse
Improving communication between providers, increasing use of alternative pain control mechanisms, and creating evidence-based prescribing guidelines will reduce the unintended distribution of prescription opioids.
This course was published in the June 2018 issue and expires June 30, 2021. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the risks of opioid prescribing, and the reasons opioid misuse is considered a public health emergency.
- List dental procedures that commonly result in opioid prescriptions, and alternative strategies for pain management.
- Describe at-risk groups and behaviors associated with opioid abuse and addiction.
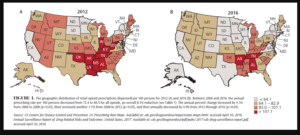
Although opioid abuse is a global concern,3 US health professionals write the largest number of opioid prescriptions worldwide (Table 1). In 2012, more than 255 million prescriptions were written, which is enough to give every American adult his or her own bottle of opioids4 (Figure 1, page 32). While there are many contributing factors, the US health care system enables the overprescription of opioids. Fragmented care with a hyper-specialized network of providers, poor communication (including a dearth of interoperable electronic health records), variable prescription regulations between states, a lack of nationally accepted prescription guidelines, and the influence of large pharmaceutical companies are driving factors in prescription abuse.5
As a result, the US drug-related mortality rate is the highest in the world, with an estimated 52,400 deaths in 2016—half of which can be attributed solely to prescription opioid overdose.6 Without a systemic intervention, the US Centers for Disease Control and Prevention projects more than 500,000 opioid-related deaths over the next 10 years.7 Not only is opioid abuse dangerous, it provides a segue that leads to the abuse of more common illicit drugs that are easier to obtain. Examining national general population heroin data, nearly 80% of heroin users reported using prescription opioids prior to heroin.8,9
Opioid abuse poses a significant economic burden on the US health care system, as well as the individuals involved. In 2011, 366,181 (or 29%) of emergency department visits involving nonmedical pharmaceutical usage were due to the use of narcotic pain relievers.10 On average, opioid abusers paid in excess of $10,000 more in annual health care costs than their matched controls.2 According to estimates by the Council of Economic Advisors, the direct and indirect societal cost of prescription opioid abuse was $504 billion in 2015.11
RELEVANCE TO ORAL HEALTH PROFESSIONALS
Many opioid prescriptions are not fully used by the patient, with one dental study finding that 54% of opioids went unused after oral surgery.12 This excess medication is a potential source for those who are seeking to experiment or abuse medications, or for accidental exposure.1
Among health professions, oral health care is unique inasmuch that approximately 85% of dentists own their practices.13 As business owners, they face the conflict of limiting pain prescriptions, while keeping patients pain free as a means of maintaining and growing their practice.14 Oral health professionals play an important role as gatekeepers in the escalation of prescription opioid abuse and can help with substance abuse screening. Within dentistry, surgical, root canal, and implant procedures generate the highest rates of opioid prescriptions.1
Patients exhibiting drug-seeking behaviors may present to the dental office for the specific purpose of obtaining opioid prescriptions, and may avoid treatment or otherwise attempt to manipulate providers in order to get prescriptions from different dentists and physicians. Adopting vigilant and judicious practices for all prescribing can help health care professionals, including oral health professionals, fight drug abuse and addiction.

SUGGESTED PRESCRIPTION PRACTICES
1. The goal of the oral health professional-patient interaction should be to deliver direct care. Oral health professionals should be suspicious of patients who avoid direct care as a means of requesting pain control. Private dental offices should partner with community health centers and other low- or no-cost dental providers. Through these partnerships, oral health professionals can directly refer patients without the ability to pay and avoid the need for a prescription to “hold them over.”
2. Current research identifies several at-risk groups for opioid addiction and misuse. These include individuals with psychiatric comorbidities and previous hospital inpatient stays,7 past or current substance abuse, and alcohol or tobacco use.15 By reviewing a thorough health history, dental providers may be able to identify individuals from these high-risk groups for whom an opioid prescription may not be prudent.
3. In pain management, oral health professionals are advised to consider nonpharmacological therapies, such as acupuncture, mindfulness, and meditation techniques.16 Some patients will be more open to these solutions than others, and may prefer a nonpharmacological approach.
4. Oral health professionals should consider nonopioid therapies before opioids. For many patients, a prescription for nonsteroidal anti-inflammatory medication, combined with education on the benefits of scheduling, is one of the best strategies for managing pain. Recent research has shown that the combination of 400 mg of ibuprofen with 1,000 mg of acetaminophen provided more effective pain relief than any opioid-containing medication or medication combination included in the study.17 This drug scheduling protocol is recommended by the Agency for Healthcare Research and Quality.18
5. If an opioid must be prescribed, the oral health professional should limit the amount to what is needed for the duration of exceptional pain. The US Food and Drug Administration is looking to influence how manufacturers package opioids, with the goal of developing single-use packaging to limit the risk of addiction.19
6. In addition, oral health professionals are advised to consult the prescription drug monitoring programs (PDMP) available in their state to avoid overprescribing. Less than half of dental professionals perform drug screening or consult a PDMP before prescribing; that noted, laws are changing and this is becoming mandatory across the US.20
7. Research supports the notion that effective pain relief requires a multidisciplinary approach.21 Although access to a pharmacist to facilitate multidisciplinary discussion may not always be convenient, collaborating with a dental hygienist will almost always be convenient and is recommended. In one study, practitioners who collaborated with other health care professionals were five times less likely to prescribe opioids and instead develop other treatment options.16
8. Oral health professionals should educate patients about the safe use and disposal of prescription medications, especially opioids. The dental hygienist is the key patient educator in any practice and often has the closer relationship with patients than the dentist. This skill set should be leveraged to help communicate messages pertaining to safe opioid storage, disposal, and utilization. Most patients do not know how to safely dispose of unused prescription drugs.1 Oral health professionals should also be prescribing for outcome not convenience. When hydrocodone was reclassified as a Schedule II from a Schedule III drug, prescriptions plummeted as clinicians found other solutions for pain management.22 In other words, the prescription should suit the situation and needs of the patient.
Once all other alternatives have been ruled out, opioids should be prescribed in specific instances—and with careful patient screening and follow-up—to ensure successful treatment.
CONCLUSION
Oral health professionals receive extensive training on how to diagnose and treat orofacial pain. The use of prescription analgesics is rarely necessary. Completing a thorough medical and social history will enable oral health professionals to understand a patient’s sociocultural viewpoint on pain and pain management. This will enable the provision of customized management of intraoperative and post-operative pain.
As individuals live longer and present with complex medication regimens and chronic illness, there will be a growing need for oral health professionals to communicate with other health professionals in delivering optimal care. An interdisciplinary effort to improve communication between providers, increase utilization of alternative pain control mechanisms, and create evidence-based prescribing guidelines will reduce the unintended distribution of prescription opioids and, in turn, help mitigate the global opioid crisis.
REFERENCES
- Denisco R, Kenna G, O‘Neil M, et al. Prevention of prescription opioid abuse: the role of the dentist. J Am Dent Assoc.2011;142:800–810.
- Rice J, Kirson N, Shei A, et al. Estimating the costs of opioid abuse and dependence from an employer perspective: a retrospective analysis using administrative claims data. Appl Health Econ Health Policy. 2014;12:435–446.
- 3.United Nations Office on Drug and Crime. World Drug Report 2012. Available at: unodc.org/unodc/en/data-and-analysis/WDR-2012.html. Accessed April 10, 2018.
- U.S. Centers for Disease Control and Prevention. Opioid Painkiller Prescribing, Where You Live Makes a Difference. Available at: cdc.gov/vitalsigns/opioid-prescribing/. Accessed April 10, 2018.
- U.S. Department of Health and Human Services. About the U.S. Opioid Epidemic. Available at: hhs.gov/opioids/about-the-epidemic/. Accessed April 10, 2018.
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Available at: samhsa.gov/data/sites/default/files/NSDUHresults2012/NSDUHresults2012.pdf. Accessed April 10, 2018.
- Shei A, Rice J, Kirson N, et al. Characteristics of high-cost patients diagnosed with opioid abuse. J Manag Care Spec Pharm. 2015;21:902–912.
- Substance Abuse and Mental Health Services Administration. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. Available at: samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm. Accessed April 10, 2018.
- Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers — United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132:95–100.
- Crane EH. Emergency Department Visits Involving Narcotic Pain Relievers. Available at: samhsa.gov/data/sites/default/files/report_2083/ShortReport-2083.html. Accessed April 10, 2018.
- The Council of Economic Advisors. The Underestimated Cost of the Opioid Crisis. Available at: whitehouse.gov/sites/whitehouse.gov/files/images/The%20Underestimated%20Cost%20of%20the%20Opioid%20Crisis.pdf. Accessed April 10, 2018.
- Maughan B, Hersh E, Shofer F, et al. Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug Alcohol Depend. 2016;168:328–334.
- Vujicic M. Practice ownership is declining. J Am Dent Assoc. 2017;148:690–692.
- Steinmetz C, Zheng C, Okunseri E, Szabo A, Okunseri C. Opioid analgesic prescribing practices of dental professionals in the United States. JDR Clin Trans Res. 2017;2:241–248.
- Webster LR. Risk Factors for opioid-use disorder and overdose. Anesth Analg. 2017;125:1741–1748.
- Stewart A, Zborovancik K, Stiely K. The impact of pharmacy services on opioid prescribing in dental practice. J Am Pharm Assoc. 2017;57(2S):S78–S82.
- Moore PA, Ziegler KM, Lipman RD, Aminoshariae A, Carrasco-Labra A, Mariotti A. Benefits and harms associated with analgesic medications used in the management of acute dental pain: An overview of systematic reviews. J Am Dent Assoc. 2018;149:256–265.
- Agency for Healthcare Research and Quality. Pain: assessment, non-opioid treatment approaches and opioid management. Available at: guideline.gov/summaries/summary/50568. Accessed April 10, 2018.
- American Dental Association. FDA explores single-dose packaging to reduce opioids abuse. Available at: ada.org/en/publications/ada-news/2018-archive/january/fda-recommends-single-dose-packaging-to-reduce-opioids-addiction. Accessed April 10, 2018.
- McCauley J, Leite R, Melvin C, Fillingim R, Brady K. Dental opioid prescribing practices and risk mitigation strategy implementation: Identification of potential targets for provider-level intervention. Subst Abus. 2015;37:9–14.
- Jukiewicz DA, Alhofaian A, Thompson Z, Gary FA. Reviewing opioid use, monitoring, and legislature. Int J Nursing Sci.2017;4:430–436.
- Chacko J, Greenstein J, Ardolic B, Berwald N. Effect of an emergency department opioid prescription policy on prescribing patterns. Am J Emerg Med. 2017;35:1327–1329.
From Dimensions of Dental Hygiene. June 2018;16(6):30-32,35.



