 WARDOLINE/ISTOCK/GETTY IMAGES PLUS
WARDOLINE/ISTOCK/GETTY IMAGES PLUS
Importance of Implant Maintenance
Dental hygienists lead the way in ensuring the health, function, and maintenance of dental implants.
According to the American Academy of Implant Dentistry, 3 million people in the United States have implants with that number growing by 500,000 each year.1 Dental hygienists are charged with determining which instruments to use, instituting appropriate maintenance regimens, recognizing dental implant health or disease, and establishing an overall treatment plan for implant sustainability and longevity.
Dental hygienists need to understand the role dental implant fixtures play in the overall health and quality of life for patients. Endosseous, or endosteal, dental implants are screw-shaped, placed into the maxilla or mandible, and function as a tooth root to be restored with a crown, achieving the look and feel of natural tooth replacement. In addition to replacement of one or more teeth, dental implants also provide support for fixed or removable prostheses, with restorations that can be screw retained, cement retained, or a combination of both.2 The risk of bone loss in the mandible increases with the amount of time a tooth is missing, therefore, dental implants are also important for alveolar ridge preservation.1 Dental implant placement is an important consideration for daily function, proper occlusion, speech, mastication, nutrition, facial shape, quality of life, and overall health and well-being.
The clinical assessment is multifaceted before, during, and post-implant placement. Pathogenic biofilm accumulation related to poor oral hygiene or impaired host response will set oral rehabilitation up for failure. Bruxism, smoking, uncontrolled diabetes, and periodontal diseases are all risk factors for infection surrounding dental implants. Complications can also arise from insufficient clinical skills; poor assessment, treatment planning, and prosthetic design; and patient-specific host factors.3,4
MAINTENANCE PROTOCOL
Dental hygienists play an integral role in the early detection of dental implant diseases and providing individualized patient care in the maintenance protocol. Despite the high survival rate for dental implants—96.33%—the risk for complications remains possible.4–7 Dental hygienists must be equipped to provide treatment in all aspects of dental implant placement including the healing phase, surgical, prosthetic, and maintenance periods. Research suggests that ongoing dental hygiene care, both professional and patient-driven, is essential in efforts to prevent implant failure and irreversible destruction.6–9
In maintenance therapy, the goal is to prevent peri-implant mucositis, the early stage of peri-implant disease.10,11 Preventive maintenance appointments can vary from 1-month to 6-month intervals, depending on the patient and cleansability of the implant restoration.12,13 Recare intervals of up to 3 months are suggested, especially for patients with a history of periodontal diseases, to ensure bacterial load reduction with professional treatment and reinforcement of at-home techniques. Both professional clinical care and patient care must be revised as needed.
Professional dental hygiene care includes the removal of biofilm and calculus at each maintenance visit, while avoiding implant abutment damage as much as possible. In an effort to reduce such bacterial load, studies have suggested that the hardness of the scaler tip may prove to be more detrimental than the actual application method itself.11 It is widely accepted that local debridement of implants be performed with instruments that are softer than titanium.10,14 However, a study by Huang et al9 tested the abilities of instruments to alter both titanium and zirconia implant abutment surfaces and then looked at bacterial adhesion. They concluded that the use of a titanium curet led to deep linear carving marks in titanium abutments, allowing for significant surface changes, increased abutment roughness, and higher optical density of adhered bacteria. The authors suggested that titanium curets be used with care on titanium abutments. Conventional metal, such as stainless steel, remains contraindicated for use with implants, as more surface damage creates ideal niches for biofilm accumulation and bacterial adhesion.9,15–17 Studies suggest these instruments allow for contamination of the titanium implant surface with other metal ions over time, therefore, are contraindicated for regular therapeutic use.9 Plastic scalers, although safe on implant surfaces, have poor cleaning properties and may leave fragments. Plastic instruments reinforced with graphite and gold-plated curets have been suggested, however, they may breakdown.12
Ultrasonic scaling may create scratches on smooth surfaces. Chun et al11 studied ultrasonic scaler tips and found that the use of copper and bronze scaler tips showed minimal surface damage as compared to stainless steel, but were less efficient at removal. However, the limitations of this study involved various factors including material, design, frequency-generating vibration, water flow rate, power, angling, and load.6 Minimal damage to the abutment surface in efforts to disrupt and remove submucosal biofilm accumulation may be carefully achieved using ultrasonic scaler tips that are soft (nonmetal) or made of copper alloy.14 More research is necessary to determine the best instruments for ultrasonic use in implant maintenance therapy.
Some patients with dental implants have soft tissue recession, dental implant fixture exposure, and heavy calculus deposits, which may require treatment revisions to remove surface irregularities in an effort to facilitate hygiene care. Research indicates a metal scaling tip, titanium curet, titanium brush, or diamond bur may be necessary in these scenarios to promote a healthier environment for the dental implant.15,16
Dental hygienists should also think outside of the instrument treatment cassette. In addition to scaling to remove hard and soft deposits, incorporating the use of oral hygiene aids as adjunctive therapies have been researched. Rubber cup polishing with a nonabrasive paste, rubber tip stimulators and interdental brushes, preferably with coated wire to prevent scratching of the implant abutment surface, can aid in biofilm removal.
Floss or gauze dipped in chlorhexidine 0.12% can be used carefully to reduce the bacterial load.10 However, some research studies show that Porphyromonas gingivalis cells within biofilms are resistant to antimicrobials.18 Dental hygienists need to proceed with caution as some of these adjunctive aids can breakdown, causing foreign materials to linger around implant surfaces.
Recent studies have looked at air polishing with glycine powder for biofilm removal surrounding dental implants. Glycine powder is less abrasive than sodium bicarbonate and is effective in removing significant amounts of biofilm; however, it is still accompanied by minimal surface roughness.14,19,20 More research is necessary as some studies report air polishing can damage porcelain or composite materials, create random pitting surface irregularities on the titanium, and harm the soft tissue connection by detaching it from the implant; while rare, this can increase the risk of subcutaneous emphysema.12,21
Periodontal probing is an assessment tool for evaluating peri-implant tissues; however, current studies suggest that less force exertion must be exercised. Gulati et al12 found that junctional epithelial attachment zones differ in their strength attachment to the implant as compared to a natural tooth. Periodontal probing—using a metal or plastic probe—may be helpful in peri-implant assessment and should be performed at maintenance appointments using light pressure; however, Gulati et al12 suggest it should be avoided during the first 3 months after abutment connection to assure proper healing and establishment of the soft tissue seal. Research concludes that progressively deepening probing depths and bleeding on probing may be more significant than solely using probing depth values of ≥ 4 mm or 5 mm. As such, documentation is fundamental from baseline (when possible) through each maintenance visit.12,22
Keeping with the “as low as reasonably achievable” concept, radiographs are suggested at 1 month, 2 months, 6 months, and 1 year following a dental implant placement, and annually thereafter with visual and radiographic evaluation.3 Alveolar crestal bone from periapical and vertical bitewings should be compared with the baseline to assess any changes.12,23 If changes occur after the first year of loading, Gulati et al13 suggest that radiographs be taken every 6 months to 8 months until dental implant stability is achieved following occlusal stress reduction. If there are no changes in the alveolar crestal bone following the first year and clinical signs are favorable, radiographic evaluation may take place every 3 years.12 Dental hygienists should obtain past clinical records and radiographs if a new patient presents with an implant-supported prosthesis in order to accurately assess any changes in bone levels. However, if previous radiographs are not available, bone levels ≥ 3 mm apical to the most coronal portion of the implant, combined with bleeding on probing, are consistent with the peri-implantitis diagnosis.23,24
Dental hygienists may use an intraoral camera to educate patients or to check the effectiveness of their self-care routine. Patients can isolate any redness, inflammation, or other signs of disease around the dental implant so preventive measures can be taken to avoid dental implant failure.12
PATHOGENESIS OF COMPLICATIONS AND FAILURE
P. gingivalis is the biggest culprit in the development of periodontal diseases, including peri-implant diseases. When pathogenic biofilm interferes with hard and soft tissues surrounding dental implants, it can lead to implant failure when left untreated.18 While the oral environment and soft tissue surrounding a natural tooth is similar to that of an implant, the peri-implant keratinized tissue has a higher risk of infection due to its vulnerability from decreased vascularity and lack of true connective attachment.25–27 Controversy exists regarding long-term peri-implant tissue health and the necessity of keratinized tissue surrounding implants. However, studies have indicated that the presence of keratinized gingiva is preferable due to the ease of maintaining oral hygiene compared to the inflammatory risks of mobile, nonkeratinized mucosa, and in regards to patient comfort.8,23,25
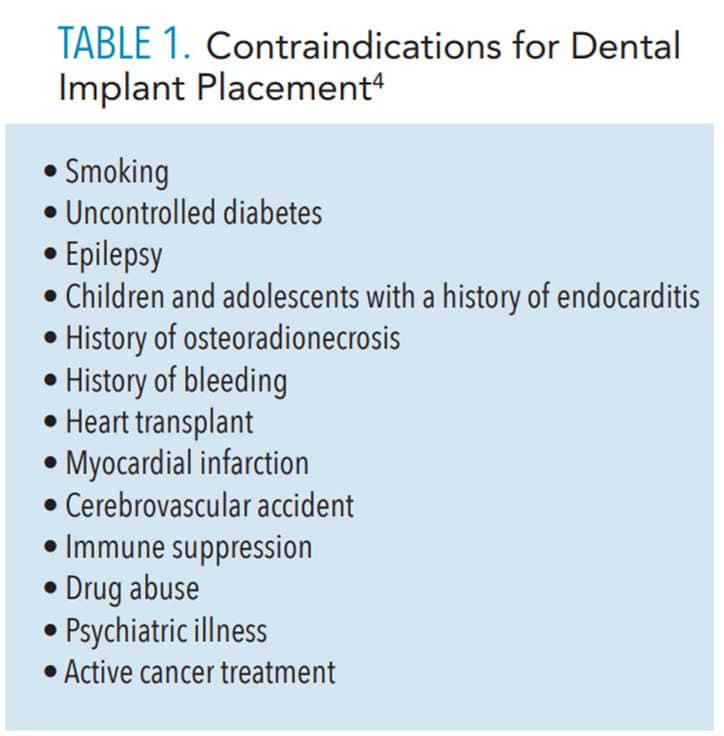
Bleeding from the dental implant site, infection, and pain are the common signs of early disease and complications.3 Dental implant complications and failure can result from biological processes, mechanical inadequacies, or patient adaptation.28 Table 1 lists contraindications for dental implant placement.4
Dental implant failure has two stages: early and late. Early failure occurs within the first few weeks to months, consisting of bone necrosis, bacterial infection, initial inadequate stabilization, surgical trauma, early occlusal load, and properties within the host tissue. Late failure occurs subsequently and can arise due to functional loading and infection resulting from pathological processes.4,28 Even after a dental implant has osseointegrated, a number of variables can contribute to implant failure. A break in osseointegration can result from an etiological factor and lead to a late failure.28 A severe inflammatory reaction can occur rapidly in the presence of a foreign body invasion, like that of excess residual cement from placement of the prosthetic crown. Exploration and radiographic surveys can aid in the detection of excess residual cement, although only certain types of cements are visible radiographically.29
ROLE OF THE DENTAL HYGIENIST
Routine assessment of peri-implant tissue changes and mechanical biofilm removal with the use of appropriate armamentarium that will avoid damage to abutment surfaces are key to implant health.3,9 Reinforcing proper oral hygiene instruction and self-care regimens are essential. Continual reinforcement of tobacco cessation must be included in patient education as smoking weakens bone structure and inhibits the initial healing process.30 Clinical assessment of bleeding, inflammation, mobility, probing comparisons, and inquiry regarding pain or daily complications will help the assessment process, as well as radiographic assessment.
Oral hygiene instruction should include interproximal brushes and cleaners, end-tufted brushes, water flossers, soft manual toothbrushes and gentle power brushes, floss, and threader floss. Some of these aids may leave behind residue, therefore, careful mechanical demonstration and instruction are crucial.
The use of a rubber tip stimulator can aid in mechanical biofilm removal. During implant healing stages, chemotherapeutic agents, such as chlorhexidine 0.12%, have been recommended as a mouthrinse or carefully applied to the area with a cotton tip applicator when mechanical removal is temporarily contraindicated.12
UPDATED PERIODONTAL CLASSIFICATIONS
The American Academy of Periodontology (AAP) and the European Federation of Periodontology have added peri-implant diseases and conditions to the Classification of Periodontal and Peri-implant Diseases and Conditions.31 The AAP has defined peri‐implant mucositis as inflammation of the soft tissues surrounding a dental implant, without additional bone loss after the initial bone remodeling that may occur during post-implant placement healing.32 The diagnosis of peri‐implant mucositis should be based on clinical signs of gingival inflammation during routine clinical examinations. Additionally, radiographic images should be evaluated to exclude bone level changes consistent with peri‐implantitis.
Peri-implantitis presents with the same clinical features as periodontitis with inflammation of mucosal tissue and subsequent bone loss around the dental implant. It has been defined as an inflammatory lesion of the mucosa surrounding an endosseous implant and with progressive loss of supporting peri‐implant bone.32 Following implant installation and initial loading, some crestal bone height is lost (between 0.5 mm and 2 mm) in the healing process.33,34 Any additional radiographic evidence of bone loss suggests peri‐implant disease. The progression of periodontitis is episodic with periods of activity and remission, which can be the same for peri‐implantitis. Based on this knowledge and in attempting to extrapolate it to peri‐implantitis, any bone loss greater than 2 mm is indicative of peri‐implantitis.35
The diagnosis of peri‐implantitis requires bleeding on probing in addition to the presence of pathological bone loss. Following initial healing, additional bone loss of 0.5 mm to 5 mm as assessed from radiographs is a necessary criterion for the diagnosis of peri‐implantitis.24 The pathological bone loss for implants initiating peri‐implantitis is:
- Peri–implantitis lesions present with the same clinical signs of inflammation as peri‐implant mucositis.
- The distinctive difference between a diagnosis of peri‐implant mucositis and peri‐implantitis is the presence of bone loss in peri‐implantitis, as identified from dental radiographs.36
The same principles used to assess the pathological bone loss regarding peri‐implant mucositis and peri‐implantitis in clinical practice should be applied at each periodontal maintenance visit. However, radiographic and clinical information from the time when the dental implant was placed may not be available. Under such circumstances, a distance from the implant platform to bone contact ≥ 3 mm, and in conjunction with bleeding on probing would be required for the diagnosis of peri‐implantitis.24
According to Renvert et al,24 the diagnosis of peri‐implantitis requires:
- Evidence of visual inflammatory changes in the peri‐implant soft tissues combined with bleeding on probing and/or suppuration.
- Increasing probing pocket depths as compared to measurements obtained at placement of the supra‐structure.
- Progressive bone loss in relation to the radiographic bone level assessment at 1 year following the delivery of the implant‐supported prosthetics reconstruction.
- In the absence of initial radiographs and probing depths, radiographic evidence of bone level ≥ 3 mm and/or probing depths ≥ 6 mm in conjunction with profuse bleeding.
CONCLUSION
Dental implant maintenance and patient self-care are essential to preventing peri-implant diseases. Dental hygienists need to be prepared to recognize the clinical characteristics regarding peri-implant diseases and conditions and refer patients to a periodontist in order to sustain peri-implant health. Dental hygiene care is key to preventing peri-implant diseases, which is fundamental to dental implant health, maintenance, and function.
REFERENCES
- American Academy of Implant Dentistry. About Dental Implants. Available at: aaid.c/m/about/Pre_s_Room/History_and_Background.html. Accessed March 25, 2020.
- Thalji G, Bryington M, De Kok IJ, Cooper LF. Prosthodontic management of implant therapy. Dent Clin North Am. 2014;58:207–225.
- Egilmez F, Ergun G, Cekic-Nagas I, Bozkaya S. Implant-supported hybrid prosthesis: conventional treatment method for borderline cases. EuJ J Dent. 2015;9:442–448.
- Raikar S, Talukdar P, Kumari S, Panda SK, Oommen VM, Prasad A. Factors affecting the survival rate of dental implants: a retrospective study. J Int Soc Prev Community Dent. 2017;7:351–355.
- Jang HW, Kang JK, Lee K, Lee YS, Park PK. A retrospective study on related factors affecting the survival rate of dental implants. J Adv Prosthodont. 2011;3:204–215.
- Kandasamy B, Samson EP, Yaqoob A, Pandey P, Deenadayalan S, Das I. Evaluation of clinical parameters in implant maintenance phase for prevention of peri-implantitis. J Int Soc Prev Community Dent. 2018;8:361–364.
- Ogata Y, Nakayama Y, Tatsumi J, et al. Prevalence and risk factors for peri-implant diseases in Japanese adult dental patients. J Oral Sci. 2017;59:1–11.
- Monje A, Insua A, Wang HL. Understanding Peri-implantitis as a plaque-associated and site-specific entity: on the local predisposing factors. J Clin Med. 2019;8:279.
- Huang YS, Hung CY, Huang HH. Surface changes and bacterial adhesion on implant abutment materials after various clinical cleaning procedures. J Chin Med Assoc. 2019;82:643–650.
- Prathapachandran J, Suresh N. Management of peri-implantitis. Dent Res J (Isfahan). 2012;9:516–521.
- Chun KA, Kum KY, Lee WC, Baek SH, Choi HW, Shon WJ. Evaluation of the safety and efficiency of novel metallic implant scaler tips manufactured by the powder injection molding technique. BMC Oral Health. 2017;17:110.
- Gulati M, Govila V, Anand V, Anand B. Implant maintenance: a clinical update. Int Sch Res Notices. 2014;2014:908534.
- Monje A, Aranda L, Diaz KT, et al. Impact of maintenance therapy for the prevention of peri-implant diseases: a systematic review and meta-analysis. J Dent Res. 2016;95:372–379.
- Armitage GC, Xenoudi P. Post‐treatment supportive care for the natural dentition and dental implants. Periodontol 2000. 2016;71:164–184.
- Mann M, Parmar D, Walmsley AD, Lea SC. Effect of plastic covered ultrasonic scalers on titanium implant surfaces. Clin Oral Impl Res. 2012;23:76–82.
- Park JB, Lee SH, Kim N, et al. Instrumentation with ultrasonic scalers facilitates cleaning of the sandblasted and acid-etched titanium implants. J Oral Implantol. 2015;41:419–428
- Duarte PM, Reis AF, de Freitas PM, Ota-Tsuzuki C. Bacterial adhesion on smooth and rough titanium surfaces after treatment with different instruments. J Periodontol. 2009;80:1824–3182.
- Gerits E, Verstraeten N, Michiels J. New approaches to combat Porphyromonas gingivalis biofilms. J Oral Microbiol. 2017;9:1300366.
- Bennani V, Hwang L, Tawse-Smith A, Dias GJ, Cannon RD. Effect of air-polishing on titanium surfaces, biofilm removal, and biocompatibility: a pilot study. Biomed Res Int. 2015;2015:491047.
- Lupi SM, Granati M, Butera A, Collesano V, Rodriguez Y, Baena R. Air‐abrasive debridement with glycine powder versus manual debridement and chlorhexidine administration for the maintenance of peri‐implant health status: a six‐month randomized clinical trial. Int J Dent Hygiene. 2016;15:287–294.
- Lee ST, Subu MG, Kwon TG. Emphysema following air-powder abrasive treatment for peri-implantitis. Maxillofac Plast Reconstr Surg. 2018;40:12.
- Lang NP, Berglundh T. Periimplant diseases: where are we now? Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011;38:178–181.
- Berglundh T, Armitage G, Araujo MG, et al. Peri‐implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Clin Periodontol. 2018;45(Suppl 20):S286– S291.
- Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri‐implant health, peri‐implant mucositis, and peri‐implantitis: Case definitions and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S304–S312.
- Sison SG. Implant maintenance and the dental hygienist. Available at: kiezenoftrekken.nl/downloads/supimplant.pdf. Accessed March 25, 2020.
- Sahayata V. Zone of keratinized tissue around implants really matters? J Dent Oral Health. 2017;3:1–2.
- Narayan SJ, Singh PK, Mohammed S, Patel RK. Enhancing the zone of keratinized tissue around implants. J Indian Prosthodont Soc. 2015;15:183–186.
- Tonetti MS, Schmid J. Pathogenesis of implant failures. Periodontol 2000. 1994;4:127–138.
- Tatullo M, Marrelli M, Mastrangelo F, Gherlone E. Bone inflammation, bone infection and dental implants failure: histological and cytological aspects related to cement excess. J Bone Jt Infect. 2017;2:84–89.
- Kasat V, Ladda R. Smoking and dental implants. J Int Soc Prev Community Dent. 2012;2:38–41.
- American Academy of Periodontology. AAP releases proceedings from the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. American Academy of Periodontology. Available at: perio.org/consumer/2017-workshop-proceedings. Accessed March 25, 2020.
- Peri‐implant mucositis and peri‐implantitis: a current understanding of their diagnoses and clinical implications. J Periodontol. 2013;84:436–443.
- Lindquist LW, Carlsson GE, Jemt T. A prospective 15‐year follow‐up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clin Oral Implants Res. 1996;7:329–336.
- Cochran DL, Nummikoski PV, Schoolfield JD, Jones AA, Oates TW. A prospective multicenter 5‐year radiographic evaluation of crestal bone levels over time in 596 dental implants placed in 192 patients. J Periodontol. 2009;80:725–733.
- Sanz M, Chapple IL. Clinical research on peri‐implant diseases: consensus report of working group 4. J Clin Periodontol. 2012;39(Suppl 12):202–206.
- Schwarz F, Derks J, Monje A, Wang H‐L. Peri‐implantitis. J Periodontol. 2018;89(Suppl 1):S267–S290.
From Dimensions of Dental Hygiene. April 2020;18(4):16-18,21.

