 JUHY13/E+/GETTY IMAGES PLUS
JUHY13/E+/GETTY IMAGES PLUS
Implant Care in Patients With Diabetes
While implant therapy is a feasible option in patients with this metabolic disorder, oral health professionals need to consider a variety of factors before moving forward.
This course was published in the October 2019 issue and expires October 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the risks caused by tooth loss.
- Discuss the bidirectional relationship between diabetes and periodontal diseases.
- List the factors that influence implant therapy success and failure.
- Explain protective strategies that both clinicians and patients can use to improve implant health.
Replacing missing teeth with dental implants has become more common than ever before in adults. The American Academy of Implant Dentistry estimates that more than 3 million Americans have dental implants, and the number continues to grow each year.1 The option of dental implants as a means to replace missing teeth may allow for increased function for many individuals, giving them the ability to speak with ease, increase their confidence and self-esteem, enjoy foods that were once difficult to bite and chew, and improve the overall ability to complete oral hygiene care. Dental implants are a long-term investment, and the longevity and overall stability of a dental implant depends on factors such as the patient’s overall systemic health and level of oral hygiene and whether he or she receives regular professional dental care.2
DIABETES MELLITUS
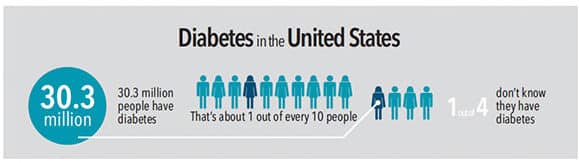
Diabetes mellitus (DM)—both type 1 and type 2—is a chronic metabolic disease that impairs the body’s ability to produce or use insulin, resulting in increased levels of glucose in the blood. It affects nearly 10% of the United States population (Figure 1).3 Individuals with DM require both regular self-monitoring of their blood glucose and periodic assessment of their average plasma glucose concentration in their blood, as measured by glycated hemoglobin level (HbA1c). HbA1c is measured roughly every 3 months and provides a picture of disease control and stability. In the past, dental implants may have been contraindicated for patients with DM because of the bidirectional relationship that exists between diabetes and periodontal diseases.4 Both of these chronic diseases increase the risk for dental implant failure due to reasons such as delayed wound healing, unstable osseointegration of the implant post, and post-operative infections or infections of the surrounding soft tissues.4,5
RISKS OF TOOTH LOSS
Dental implants are increasingly recommended for patients with DM.4 Recent systematic reviews suggest the multiple benefits of dental implants replacing missing teeth for individuals with DM.4,6 This is a welcome change as tooth loss and overall edentulism can lead to nutritional deficiencies and comorbidities—including uncontrolled DM—due to the difficulty of chewing a variety of nutritious foods. Research suggests that edentulous individuals may be more prone to a diet lacking in proper nutrition. Likewise, individuals with type 1 DM may experience a decrease in salivary flow, which may, in turn, lead to consuming foods that are easier to chew and swallow.6 These foods tend to be high in fat and sugar. Poor food choices can ultimately lead to higher HbA1c levels and more poorly controlled DM.7
Replacing missing teeth with implants for patients with DM can help improve their ability to thoroughly chew and enjoy healthier foods, provide for more nutritious and sustaining options, and support effective blood sugar control.4 Marchand et al5 state that the ability to maintain ideal HbA1c levels that read less than 7% is a primary factor to consider when discussing dental implant therapy as a treatment option for missing teeth.
WEIGHING THE BENEFITS VS RISKS
In the past, an increased risk of dental implant failure was seen as a contraindication for placing dental implants in patients with DM. However, there is no clear evidence suggesting this concern to be true for this patient population.8 Patients presenting with DM and HbA1c levels greater than 8% are at an increased risk for delayed wound healing and insufficient osseointegration of the implant itself, thus resulting in implant failure.9,10 The decision on whether implant placement is an appropriate choice needs to consider patients’ abilities to effectively manage their DM.
The replacement of missing teeth is not an emergency procedure that must be done in a specific time frame. Thus, oral health professionals should help patients research their options, discuss the risks associated with their choice, and encourage them to maintain overall systemic health.4 Patients with DM benefit from thorough discussions about how to maintain the health and integrity of their implant(s), and the importance of maintaining stabilized blood glucose levels through a healthy lifestyle. Proper preparation and education of patients are key components of successful implant retention in patients with DM. Additionally, oral health professionals are encouraged to collaborate with their patient’s primary care medical providers in order to strategize best outcomes for the patient and the success of the dental implant.4 Oates et al8 note that it is in the best interest of patients with DM to consider dental implants for missing teeth, but it is the duty of oral health professionals to weigh the benefits and risks of this treatment.
BIDIRECTIONAL RELATIONSHIP
Periodontitis is one of the most prevalent oral complications in patients with type 2 diabetes,11 and individuals with uncontrolled DM are at an increased risk for severe periodontal diseases when poor oral hygiene is exhibited.12,13 Periodontal conditions should be assessed when creating individualized treatment plans for patients with DM prior to implant therapy. Dental hygienists should also assess patients’ oral hygiene and reinforce positive oral hygiene care to increase successful outcomes.
Assessment of a patient’s periodontal and peri-implant status and oral hygiene care are critical parts of prevention and maintenance in patients with DM who have one or more dental implants. Dental hygienists must be aware of and account for the anatomical and biological differences from natural dentition when assessing the health of dental implants, particularly when DM is present. Oral health professionals must be alert to the health and vitality of the surrounding peri-implant tissue in order to protect the integrity of the dental implant and surrounding tooth structures, as well as the bone support necessary to maintain these structures.
Research suggests that dental implants and natural teeth have significant similarities and differences in anatomical features that can potentially put peri-implant health at risk.14 The gingiva surrounding natural teeth and the peri-implant mucosa provides a cuff-like sealing barrier, and while it offers protection against the external environment, it is also susceptible to bacterial infiltration.15 Microscopically, dental implants are lacking the connective fibers that surround natural teeth, resulting in a more delicate barrier. This susceptibility can be detrimental to the integrity and longevity of dental implants, especially in patients with DM.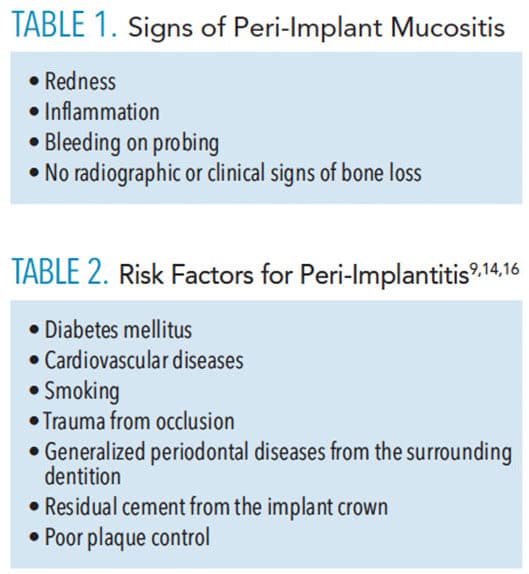
IMPLANT COMPLICATIONS
Like periodontitis, peri-implant mucositis and peri-implantitis can affect the bone and soft tissues of the periodontium surrounding the dental implant and, ultimately, lead to implant failure.14 Peri-implant mucositis is similar to gingivitis, in that it is a reversible inflammatory process of the soft tissue surrounding the dental implant that presents with similar signs and symptoms as gingivitis. Table 1 lists the symptoms of peri-implant mucositis. Peri-implant mucositis will develop into peri-implantitis if left untreated.
Peri-implantitis is the irreversible progression of peri-implant mucositis that causes bone resorption around the implant, leading to increased probing depths and infection of the surrounding soft tissue.14 Table 2 lists the risk factors for peri-implantitis.9,14,16
ORAL HEALTH EVALUATION
Dental hygienists should know what to look for when assessing the health and stability of implants. Individuals with diabetes may have an increased risk of peri-implant diseases due to the constant inflammatory responses caused by biofilm.9 The surrounding soft tissue should be evaluated by examining the color and texture of the tissue, evaluating the response of the tissue when probing around the dental implant, and examining radiographs by assessing any changes to the surrounding bone and level of the bone in order to identify the validity of a peri-implantitis diagnosis of that specific dental implant.
Lang et al17 recommend establishing baseline records at the time of the implant placement and frequently thereafter in order to assess true changes in the surrounding bone levels and increase the recognizability of peri-implant disease. The proper collection of baseline data and frequent analysis of the clinical parameters surrounding the dental implant can be vital to the longevity of dental implants.
DENTAL IMPLANT FAILURE AND SUCCESS
A number of factors play a role in implant failure. Michaeli et al18 suggest there are two major considerations when assessing the suitability of dental implants in individuals with DM: systemic and rehabilitative factors. Studies have demonstrated that dental implants in individuals with type 2 DM have a comparable rate of success when compared with healthy individuals.19–21 Other studies suggest that most failed implants in patients with DM occur during osseointegration due to the multiple processes undergone by cell structures during this period.18,20 However, predicting the likelihood of an implant’s success or failure based solely on the presence of DM is not practical. The success of implant therapy in patients with DM involves the clinician’s ability to identify patients who are most eligible and suitable for treatment by assessing multiple factors.4
A suitable patient exhibits the following characteristics:
- Well-controlled HbA1c levels between 4.0% and 7.5%
- Compliance with oral hygiene care
- Willing to adhere to strict periodontal maintenance appointments based on his or her dental provider’s recommendation for optimal oral hygiene control.10
Evidence suggests that periodontal treatments and good oral hygiene can aid in decreasing HbA1c levels in patients with DM and reduce the risk of peri-implant inflammatory parameters.16,21 Properly administered peri-implant therapies aid in establishing an environment that is manageable by both the patient and the oral health professional.16
PROTECTIVE STRATEGIES
Dental hygienists play important roles in nonsurgical periodontal therapy and preventive maintenance to support the health and stability of dental implants in patients with DM. The primary goal of recare appointments is to decrease the bacterial load around the implant and surrounding soft tissues, thereby preventing disease that can cause attachment and bone loss.16,22,23 Evidence suggests that the frequency and consistency of a periodontal maintenance appointment may increase the long-term success of an implant and prevent soft tissue pathologies such as inflammation, bleeding on probing, presence of exudate, and increased probing depths.22
The recommendation for periodontal maintenance intervals is usually every 3 months to 4 months, but clinicians should consider the patient’s oral hygiene status and his or her current periodontal condition when determining interval frequencies.16,23 Interval frequencies may be altered according to the clinical findings of the patient’s oral cavity and thus may require more frequent intervals, such as every 8 weeks. Regardless, clinicians must recognize that the primary, therapeutic goal of preventing and treating peri-implant disease is to prevent continued destruction of the periodontium and prevent or decrease the risk of tooth or implant loss through cause-related therapy.16
Oral health professionals should recommend alternative at-home oral hygiene aids and suggest strategies to improve patient compliance.24 Interproximal brushes, super floss, and water flossers, which all allow patients to effectively disrupt and remove any biofilm accumulation, may be helpful for implant patients with DM. Oral health professionals should also discuss avoiding those oral hygiene aids that may harm dental implant surfaces, such as wire-centered interdental brushes.
Successful oral hygiene is crucial for disease prevention and implant maintenance, which is emphasized by the fact that peri-implant mucositis currently affects 80% of people with dental implants.10,24 In order to decrease the progression of peri-implant diseases, patients must be educated on the importance of meticulous oral hygiene care, maintaining consistent periodontal maintenance appointments, and, in the case of patients with DM, controlling HbA1c levels through treatment compliance and healthy lifestyle behaviors.25
CONCLUSION
Considerations must be made when providing oral health care to individuals with systemic conditions that may affect treatment outcomes. The bidirectional relationship between DM and periodontal diseases is significant and must be discussed prior to determining a patient’s suitability for implant therapy. Because of the increased risk factors facing patients with DM, oral health professionals play a vital role in patient education, disease prevention, maintenance of dental implants, and the health of the surrounding soft and hard tissues.
REFERENCES
- American Academy of Implant Dentistry. About Dental Implants. Available at: aaid.com/about/Press_Room/History_and_Background.html. Accessed September 18, 2019.
- Todescan S, Lavigne S, Kelekis-Cholakis A. Guidance for the maintenance care of dental implants: clinical review. J Can Dent Assoc. 2012;78:c107.
- United States Centers for Disease Control and Prevention. Statistics About Diabetes. Available at: cdc.gov/diabetes/data/statistics/statistics-report.html. Accessed September 18, 2019.
- Naujokat H, Kunzendorf B, Wiltfang J. Dental implants and diabetes mellitus- a systematic review. Int J Implant Dent. 2016;2:5.
- Marchand F, Raskin A, Dionnes-Hornes A, et al. Dental implants and diabetes: conditions for success. Diabetes Metab. 2012;38:14–19.
- Felton DA. Edentulism and comorbid factors. J Prosthodont. 2009;18:88–96.
- Bascones-Martinez A, Gonzalez-Febles J, Sanz-Esporrin J. Diabetes and periodontal disease. Review of the literature. Am J Dent. 2014;27:63–67.
- Oates TW, Huynh-Ba G, Vargas A, et al. A critical review of diabetes, glycemic control, and dental implant therapy. Clin Oral Implants Res. 2013;24:117–127.
- Monje A, Catena A, Borgnakke WS. Association between diabetes mellitus/hyperglycaemia and peri-implant diseases: systematic review and meta-analysis. J Clin Periodontol. 2017;44:636–648.
- Donos N, Calciolari E. Dental implants in patients affected by systemic disease. Br Dent J. 2014;217:425–430.
- Stanko P, Izakovicova Holla L. Bidirectional association between diabetes mellitus and inflammatory periodontal disease. A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158:35–38.
- Mauri-Obradors E, Merlos A, Estrugo-Devesa A, et al. Benefits of non-surgical periodontal treatment in patients with type 2 diabetes mellitus and chronic periodontitis: a randomized controlled trial. J Clin Periodontol. 2017 Dec 19. [Epub ahead of print].
- Tanwir F, Tariq A. Effect of glycemic control on periodontal status. J Coll Physicians Surg Pak. 2012;22:37–44.
- Smeets R, Henningsen A, Jung O, et al. Definition, etiology, prevention and treatment of peri-implantitis- a review. Head Face Med. 2014;10:34.
- Berglundh T, Lindhe J, Ericsson I, et al. The soft tissue barrier at implants and teeth. Clin Oral Impl Res. 1991:2:81–90.
- McClain PK. Maintenance: the key to successful periodontal and implant therapy. Compend Contin Educ Dent. 2014;35(3 Suppl):4–10.
- Lang NP, Berglundh T. Periimiplant diseases: where are we now? Counsensus of the seventh European workshop on periodontology. J Clin Periodontol. 2011;38(Suppl. 11):178–181.
- Michaeli E, Weinberg I. Dental implants in the diabetic patient: systemic and rehabilitative considerations. Quintessence Int. 2009;40:639–645.
- Morris HF, Ochi S, Winkler S. Implant survival in patients with type 2 diabetes: placement to 36 months. Ann Periodontol. 2000;5:157–165.
- Annibali S, Pranno N, Cristalli MP, et al. Survival analysis of implant in patients with diabetes mellitus: a systematic review. Implant Dent. 2016;25:663–674.
- Al Amri MD, Kellesarian SV, Al-Kheraif AA, Malmstrom H, Javed F, Romanos GE. Effect of oral hygiene maintenance on HbA1c levels and peri-implant parameters around immediately-loaded dental implants placed in type-2 diabetic patients: 2 years follow-up. Clin Oral Implants Res. 2016;27:1439–1443.
- Hoerler SB, Nietz SK, Zook VL, et al. Consistency of dental hygiene therapy utilizing various dental hygiene instrumentation and its effect on peri-implant health and survival of dental implants: a retrospective study. Int J Oral Maxillofac Implants. 2017;32:1371–1376.
- Shumaker ND, Metcalf BT, Toscano NT, et al. Periodontal and periimplant maintenance: a critical factor in long-term treatment success. Compend Contin Educ Dent. 2009;30:388–390.
- Lyle DM. Implant maintenance: is there an ideal approach? Compend Contin Educ Dent. 2013;34:386–390.
- Sanz M, Solonko M, Luengo F. Key factors in prevention of peri-implant diseases. Compend Contin Educ Dent. 2017;38(8 Suppl):6–12.
From Dimensions of Dental Hygiene. October 2019;17(9):36—39.



