 PHOTO CREDIT: RICKY HARRELL, DMD, MA
PHOTO CREDIT: RICKY HARRELL, DMD, MA
Identifying and Addressing Ankyloglossia
Dental hygienists should be prepared to recognize tongue-tie and provide education and referrals to improve oral function.
This course was published in the September 2019 issue and expires September 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Recognize patients with ankyloglossia.
- Describe the adverse effects associated with untreated tongue-ties.
- Explain the three different treatment procedures for lingual correction.
- Discuss the role of the dental hygienist in identifying patients with ankyloglossia.
Dental hygienists see a variety of patients on a daily basis, ranging from infants to older adults. A thorough intraoral exam should always be completed, but often significant anomalies are not identified and/or addressed. One of these anomalies is a short lingual frenum attachment, or ankyloglossia (AG).
AG, or tongue-tie, is a congenital condition characterized by an abnormally short, thickened, or tight lingual frenum that restricts tongue mobility.1 While no standard definition exists due to varying diagnostic criteria, consequences of anomalous lingual frena can include limited forward protrusion of the tongue or reduced lateral mobility. These restrictions can result in several adverse effects both orally and systemically.2 An emerging term, tethered oral tissues,3 encompasses all buccal-ties and tongue-ties. This article, however, will primarily discuss the implications associated with AG.
PREVALENCE AND EPIDEMIOLOGY
There is much debate regarding the definition, clinical significance, need for surgical intervention, and timing of treatment for patients exhibiting signs of AG.4 The prevalence of AG is believed to be between 4% and 11%, but there is neither an accepted criterion standard nor clinically practical criteria for diagnosing the condition. One variable for the high prevalence is due to age-related differences with some cases resolving spontaneously on their own.5 Though it appears there is no racial predilection, AG appears to be more common in males than females.2,6 The condition can occur solely or in association with other craniofacial abnormalities. The rare syndromes associated include X-linked cleft palate syndrome, Opitz syndrome, Van Der Woude syndrome, and Beckwith-Wiedemann syndrome.7
ADVERSE EFFECTS
The degree of frenum attachment in the oral cavity for individuals with AG affects oral, systemic and psychological health—from difficulty breastfeeding to unsatisfactory oral hygiene to pronunciation disorders.8 If the frenum area is attached too proximal to the tip of the tongue, limitations exist in common activities such as licking the lips, playing a wind musical instrument, kissing, and eating certain foods such as ice cream.1,4,6 Tight frenum attachments can also lead to improper brushing or use of oral hygiene aids. One way to determine if patients are at increased risk of calculus or caries due to tight frenum attachments is to observe if they are able to lateralize the tongue and clean the buccal vestibules.5 The tight attachment is conducive to plaque accumulation, ultimately affecting patients’ gingival and periodontal health.9
Breastfeeding. Breastfeeding may be difficult for infants with AG due to the restrictive tongue movement that prevents them from extending their tongue over the lower gumline to form a proper seal.4,10 Infants with AG need to strain to keep the breast in their mouth or experience an unsustained latch and will fall asleep while feeding without being satisfied.11
Between 12.8% and 44% of infants reportedly experience breastfeeding problems, yet the clinical significance of AG remains controversial.12 A common finding among pediatricians and otolaryngologists is that no treatment is recommended, while other specialties strongly encourage frenotomies. Frenotomies have been shown to reduce mothers’ nipple pain in the short term, however there has not been a consistent positive effect on breastfeeding in general.7 Ultimately, any condition that may affect successful breastfeeding is considered a public health issue and should be addressed.2
Speech. Although scientific evidence demonstrating a relationship between speech disorders and AG is lacking, AG can interfere with articulation in later years, while not necessarily causing a delay in speech development.4 Adults and children with AG may be self-conscious while speaking, altering the opening of their mouths. These individuals tend to speak with a small opening, slowly, softly, or loudly in order to pronounce specific consonants. While dentists lack knowledge in phonetic analysis, they need to be able to judge articulatory production.3 The vocalization of consonants and sounds like “S,” “T,” “Th,” “N,” “L,” and “D” are prominently affected, while it is especially difficult to roll an “R.”4,6,13,14 If making these sounds is difficult, a speech pathologist should intervene to correct these problems. Occasionally, parents/caregivers will demand surgical correction in the hope that normal speech and language will result.4
Sleep Apnea. A common condition that occurs when the upper airway becomes blocked repeatedly during sleep, sleep apnea reduces or completely stops airflow. It can be caused by an individual’s physical structure, including a short lingual frenum that modifies the tongue position.15 When the tongue rests in the airway, there is reduced flow of oxygen to the brain, interfering with normal neurological growth and development.16,17 After full tongue-tie release, children and adults have been found to sleep more deeply, snore less, exhibit fewer movements, and feel more refreshed in the morning.17 There is also a secondary association of tongue-tie with anterior and posterior crossbite, disproportionate growth of the mandible, and abnormal growth of the maxilla.15 AG may contribute to open mouth breathing or altered swallowing patterns that, in turn, promote elongation of the soft palate.18
Gingival Recession. Recession can be caused by many factors including improper toothbrushing, malalignment, plaque-induced inflammatory lesions, or periodontal diseases. While more studies are needed, it has been shown that the location of the frenal insertion may cause minimal to severe localized recession, typically on the lingual aspects of teeth 24 and 25.6,9,19 The frenal pull may also result in diastema formation of the mandibular incisors.20 Patients with adequate self-care and minimal inflammation have been shown to control the severity of the recession.6
Malocclusion. The position of the tongue affects the development of the upper and lower jaws, position of the teeth in the arch, and the shape of the face and upper airway passage. Facial skeletal growth is nearly complete by age 12 with some minor changes occurring thereafter.13 If the tongue rests and remains in a low, forward position, the entire body will begin to accommodate for the possible imbalance in postural development.13 A protrusive chin may be noted as a result of the low tongue position, favoring either mandibular hyper development or maxillary hypodevelopment.14 While there is still limited evidence that tongue-tie plays a role in malocclusion—especially Class III malocclusion—evidence does show that irregular maxillary tooth alignment and a narrow, underdeveloped palate are associated.8 If noticed in adolescence, swallowing can result in an open-bite deformity due to the tongue contacting the anterior portion of the mandible with exaggerated anterior thrusts.21 More studies are needed to establish a clear correlation between malocclusion and AG.22
DIAGNOSTIC TOOLS
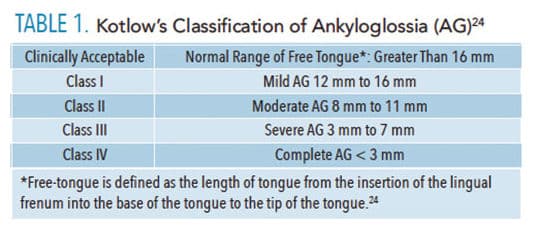
The prevalence of AG has been reported in several studies, but there is neither an accepted criterion nor clinically practical criteria for diagnosing the condition.10 More than 20 diagnostic tools are available; Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLLF), Bristol Tongue Assessment Tool (BTAT), and Lawrence Kotlow’s Classification of Ankyloglossia are the most commonly used. The assessment tools vary in length and specificity, and are utilized in different settings. For example, the HATLFF has a high reliability but is often difficult in an infant due to the amount of data that have to be gathered, while the BTAT is much simpler but lacks specificity.21,23 Table 1 includes Kotlow’s classification of AG.24
Initial evaluation for AG should occur at the time of infant delivery with properly trained personnel, but this does not commonly occur.13 With a simple finger sweep under the infant’s tongue across the floor of the mouth, mothers could be informed of potential latch difficulties and symptoms associated with an inadequate latch while feeding.11
When a professional is evaluating patients for tongue-tie, a normal range of motion of the tongue is indicated by determining whether the tip of the tongue is able to protrude outside the mouth without clefting. The clinically acceptable, normal range of free tongue is greater than 16 mm.22 To measure this, individuals are instructed to “touch the tongue to the back of the front two teeth and open your mouth.” The length of the frenum is measured by recording the distance between the insertion of the lingual frenum into the floor and the tip of the tongue.25 The tip of the tongue should be able to sweep upper and lower lips easily without straining; when the tongue is protruded the tip of the tongue will be rounded; and the lingual frenum should not create a diastema between the mandibular central incisors.8
In order to make a proper diagnosis of AG, individuals must exhibit adverse symptoms, as anatomical appearance alone is inadequate.19 Though other factors—such as socioeconomic status, region, first-time motherhood, and infant birth weight—may affect diagnosis of an infant, it is typically reliant on the practitioner’s assessment of tongue movement.19

TREATMENT
Diagnosis and surgical treatment of AG have increased over the past few decades, even without a widely accepted diagnostic criterion.19 Some providers are recognizing AG in the first few days of life and performing procedures prior to going home. If AG is noted past infancy, the treatment options involve observation and language articulation therapy.8,26 Alternative and complementary medicine treatments, such as craniosacral therapy, naturopathy, and orofacial myofunctional therapy, also may be helpful.19
Before treatment is considered, questions should be asked to determine the need for a procedure. Does the tongue-tie need to be surgically removed for function that is more adequate? Is there a more conservative approach that can be taken? If both answers lead toward the need for a procedure, several different approaches can be taken. Figure 1 to Figure 5 show a patient’s attachment pre-procedure, directly after diode laser treatment, 1 week post-op, and 1-month post-op. The primary treatment in infants is frenotomy, which involves simply cutting the frenulum. Frenectomy is defined as complete excision of the frenulum; and frenuloplasty involves various methods to release the tongue-tie and correct its anatomy.6,8,26 Pediatric dentists, oral surgeons, family dentists, pediatricians, and ear, nose, and throat physicians most commonly perform the procedure.11

There is not sufficient evidence to demonstrate which of the three main surgical techniques is the most effective.6 Infants with AG routinely have a frenotomy without local anesthesia, although topical anesthetic or a sucrose solution is highly recommended for pain control and to alleviate any parental concerns. Very little bleeding has been noted after the procedure. One study suggests all post-operative bleeding was controlled with 1 minute of pressure on the wound, and there was no delayed hemorrhage.2,6 For infants, breastfeeding helps with hemostasis and acts as an analgesic and antiseptic.10

Technique for performing a frenotomy includes the parent or an assistant holding the child in a supine position. The tongue is lifted with sterile gauze and stabilized exposing the frenum. The frenum is then divided with small sterile scissors at its thinnest point.5 Diode lasers can also be used and offer the following advantages: excellent precision, less discomfort, shorter working time, and minimal to no bleeding.27,28
For patients with a thick and vascular frenum, a frenectomy is preferred. The procedure is similar to a frenotomy where the first incision cuts the upper aspect of the frenum and the second incision cuts the lower aspect close to the floor of the mouth.28 The more rarely used procedure is a frenulectomy, or frenuloplasty, which requires general anesthesia in infants and incorporates flap elevations or z-plasties.19


Complications after frenotomy, frenectomy, and frenuloplasty are rare.6,20,27 In rare cases, hemorrhage can occur from severance of the lingual artery, recurrence of tie, lip injury, injury to Wharton’s duct, or the airway may be compromised from asphyxia caused by the released tongue falling back into the airway.10,20,27
Patients can be prescribed antibiotics, analgesics, and warm saline rinses to facilitate faster healing. Post-operative exercises for the tongue are key to establishing improvements in speech.1
IMPLICATIONS FOR THE DENTAL HYGIENIST
Inspection of the tongue should be a routine part of treatment for all patients. Regardless of age, noticeable physical characteristics—such as V-shaped notch at the tip of the tongue, inability to stick out the tongue past the lower incisors, rolling under of the tongue on protrusion, inability to touch the roof of the mouth, inability to touch the maxillary molars with the tongue, inability to lateralize the tongue/move from side to side with ease, frenum that blanches on elevation of the tongue, cupping of lateral tongue borders, and central clefting or dimpling of the tongue—should be evaluated.19
The role of the dental hygienist includes informing parents about the importance of their own oral health as well as the health of their infant. Questions can be asked regarding the infant’s or toddler’s eating habits, sleeping habits, and overall comfort. The answers to these questions provide insight to possible oral anomalies. Upon notification of any of these findings, referrals should be made for further evaluation and treatment. Pediatric dentists are capable of diagnosing and treating children presenting with oral problems.6 In older patients, periodontists can perform surgical treatments, as tongue-ties are frequent findings in patients due to the associated recession.
Untreated AG affects speech, occlusion, mandibular incisor positioning, gingival recession, mandibular growth, and tongue mobility in older children.19 With early recognition of a tight frenum, possible complications can be avoided through referral and early intervention.
CONCLUSION
The tongue is one of the most important oral structures needed for mastication and speech. AG presents as an abnormally short or tight lingual frenum, and can be identified through various diagnostic tools and criteria. While it is one of the most misdiagnosed and overlooked congenital abnormalities in the newborn population, its significance should not be underestimated.27 Individuals can experience several consequences ranging from nutritional insufficiency to impairment of mandibular growth.8 Treatment options depend on the training and philosophy of the specialist treating the condition, patient age, and degree of attachment. Dental hygienists should be prepared to recognize the condition and provide education as well as referrals to improve the patient’s oral function.
REFERENCES
- Madhusudhan KS. Untying the tongue-tie: a case report. Journal of International Medicine and Dentistry. 2017;4:72–75.
- Muldoon K, Gallagher L, McGuinness D, Smith V. Effect of frenotomy on breastfeeding variables in infants with ankyloglossia (tongue-tie): a prospective before and after cohort study. Biomed Chromatogr. 2017;17:373.
- Kotlow, L. TOTS- Tethered oral tissues: the assessment and diagnosis of the tongue and upper lip ties in breastfeeding. Oral Health. 2015;105:64.
- Kupietzky A, Botzer E. Ankyloglossia in the infant and young child: clinical suggestions for diagnosis and management. Pediatr Dent. 2004;27:40–46.
- Krol, D, Keels M. Oral Conditions. Pediatr Rev. 2007;28:15–22.
- Suter V, Bornstein M. Ankyloglossia: Facts and myths in diagnosis and treatment. J Periodontol. 2009;80:1204–1219.
- O’Shea JE, Foster JP, O’Donnell CP, et al. Frenotomy for tongue-tie in newborn infants. Cochrane Database Syst Rev. 2017;11:1–37.
- Belmehdi A, El Harti K, El Wady W. Ankyloglossia as an oral functional problem as its surgical management. Dental and Medical Problems. 2018;55:213–216.
- Salah KB. Localized severe chronic periodontitis with frenal pull and ankyloglossia: a case report. Clinical Dentistry. 2013;7:44–51.
- Segal L, Stephenson R, Dawes M, Feldman P. Prevalence, diagnosis, and treatment of ankyloglossia. Can Fam Physicians. 2007;53:1027–1033.
- Kotlow LA. Oral diagnosis of abnormal frenum attachments in neonates and infants: evaluation and treatment of the maxillary and lingual frenum using the erbium: YAG laser. J Pediatr Dent. 2004;10:11–14.
- Geddes DT, Langton DB, Gollow I, Jacobs LA, Hartmann PE, Simmer K. Frenulotomy for breastfeeding infants with ankyloglossia: Effect on milk removal and sucking mechanism as imaged by ultrasound. Pediatrics. 2008;122:188–194.
- Macaluso M, Hockenbury D. Lingual, labial frenums: early detection can prevent health effects associated with tongue-tie. Available at: rdhmag.com/articles/print/volume-35/issue-12/content/lingual-and-labial-frenums.html. Accessed August 23, 2019.
- Tsaousoglou P, Topouzelis N, Vouros I, et al. Diagnosis and treatment of ankyloglossia: A narrative review and a report of three cases. Quintessence Int. 2016;47:523–534.
- Huang Y, Quo S, Berkowski JA, Guilleminault C. Short lingual frenulum and obstructive sleep apnea in children. Int J Pediatr Res. 2015;1:1.
- Kotlow LA. TOTS- tethered oral tissues the assessment and diagnosis of the tongue and upper lip ties in breastfeeding. Available at: oralhealthgroup.com/features/tots-tethered-oral-tissues-the-assessment-and-diagnosis-of-the-tongue-and-upper-lip-ties-in/. Accessed August 23, 2019.
- Baxter R. Tongue-ties and sleep issues (and more!). Available at: lightscalpel.com/publications/tongue-ties-and-sleep-issues/. Accessed August 23, 2019.
- Yoon A, Zaghi S, Ha S, et al. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional- morphological study. Orthod Craniofac Res. 2017;20:237–244.
- Walsh J, Tunkel D. Diagnosis and treatment of ankyloglossia in newborns and infants. JAMA. 2017;143:1032–1039.
- Salah, K. Localized severe chronic periodontitis with frenal pull and ankyloglossia: a case report. Clin Dent. 2013;7:44–51.
- Bahadure RN, Jain E, Singh P, Pandey R, Chuk R. Labial ankyloglossia: a rare case report. Contemp Clin Dent. 2016;7:555–557.
- Chaubal T, Dixit MB. Ankyloglossia and its management. J Indian Soc Periodontol. 2011;15:270–272.
- Dixon B, Gray J, Elliot N, Shand B, Lynn A. A multifaceted programme to reduce the rate of tongue-tie release surgery in newborn infants: observational study. Int J Pediatr Otorhinolaryngol. 2018;113:156–163.
- Kotlow, LA. Ankyloglossia tongue-tie: a diagnostic and treatment quandary. Pediatr Dent. 1999;30:259–262.
- Yoon A, Zaghi S, Weitzman, et al. Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017:21:767–775.
- Manfro ARG, Manfro R, Bortoluzzi MC. Surgical treatment of ankyloglossia in babies–case report. Int J Oral Maxillofaci Surg. 2010;39:1130–1144.
- Barot V, Vishnoi S, Chandran S, Bakutra G. Laser: The torch of freedom for ankyloglossia. Indian J Plast Surg. 2014:47:418–422.
- Junqueira M, Cunha N, Silva L, et al. Surgical techniques for the treatment of ankyloglossia in children: a case series. J Appl Oral Sci. 2014;22:241–248.
From Dimensions of Dental Hygiene. September 2019;17(8):40–43.



