Furthering the Use of Topical Fluoride
From kids to grown-ups, topical fluoride is an effective weapon in the fight against tooth decay.
Despite their many possible uses, topical fluorides are used primarily in children. They are most often applied when the premolars erupt, with subsequent treatments declining thereafter. Although topical fluorides can be useful in other patient populations, the focus has remained on children because of topical fluorides’ obvious benefits in preventing caries in newly erupted teeth. The fact that periodontitis is the most promoted oral health problem in the adult patient population may also affect topical fluorides low usage rate in adults. Additionally, insurance reimbursement can be low or nonexistant for topical fluoride once patients pass adolescence.
The strong focus on fighting periodontitis in adults is working. National Health and Nutrition Examination Survey data show a decrease in the prevalence of periodontal diseases between 1988 (7.3%) and 2000 (4.2%).1 Data from a similar period also show a decrease in tooth decay among all adults except for those 60 and older.2
Unfortunately, the data on the rate of caries in those over 60 are not so positive. A review of five studies that looked at caries incidence among those over 50 found that older people are a caries-active group with a rate of decay as high as that found in adolescents.3 Surprisingly, coronal caries was a greater contributing factor than root caries.3 The National Report Card on Healthy Aging for adults 65+ years reports that 30% of adults in this age group with their natural teeth have untreated dental caries, whereas 25% have lost tooth-supporting structure due to advanced periodontal disease. Edentulism has declined substantially from greater than 50% of 65+ year olds in the United States in the 1950s to less than 25% in 2002.4
Dental professionals definitely need a refresher on the workings and attributes of topical fluoride application. In a Canadian study of dentists, 84% lacked a basic knowledge of topical fluoride use and the appropriate intervals for treatment.5 Similarly, a national survey of dental hygienists in the United States revealed that less than 50% recognized that dental caries is a chronic infectious disease that is more effectively treated by fluoride than by plaque removal procedures for patients of all ages.6 Most of the dental hygienists in the study were aware that adults can benefit from topical fluoride but less than 35% provided topical fluoride applications to adult patients.6 In both studies, dental professionals were not aware of fluoride’s most important mechanism of action—the remineralization of enamel, especially in early, incipient lesions. The American Dental Association (ADA) recently confirmed the need to more widely disseminate basic knowledge about the needs-based use of topical fluorides throughout the life span.7
MECHANISM OF ACTION
Topical fluorides provide effective control and protection against tooth decay. However, studies show that many dental professionals still think that fluoride’s primary effect is systemic, with ingested fluoride being deposited in the developing teeth.6 Although systemic fluoride has a pre-eruptive effect, more recent research demonstrates that its most important caries-preventive mechanisms of action are post-eruptive and topical.8
Very small amounts of fluoride in the liquid phase of plaque can, under low pH conditions, block or reduce demineralization.9 The amount of time that the fluoride remains in contact with the tooth is crucial to its effectiveness. Topical fluorides also promote remineralization. Fluoride ions in the presence of calcium and phosphate in teeth enamel readily incorporate into the enamel lattice. This precipitation and growth process is known as remineralization. Furthermore, because of their small size and the electronegative character of fluoride ions, they strongly bind to the enamel lattice and strengthen its stability.9 Thus, the attraction of fluoride to tooth enamel not only promotes remineralization but it also provides a potent protective mechanism against acids, which act to dissolve the enamel lattice (demineralization).
Finally, topical fluoride adheres to but does not directly enter tooth enamel’s crystalline structure, rather, it forms complexes of calcium fluoride (CaF2) that are loosely bound to the enamel surface. These complexes serve as a fluoride reservoir, slowly releasing the ions for the remineralization process.10 This promotion of remineralization and prevention of demineralization can arrest the progression of carious lesions, making topical fluoride an effective preventive and treatment agent for caries.
Fluoride also inhibits the action of plaque bacteria by interfering with the bacteria’s ability to produce the polysaccharides that allow them to stick to teeth, thus forming plaque biofilm. Additionally, fluoride interferes with the way cariogenic bacteria metabolize carbohydrates and produce acid.11 In laboratory studies when a low concentration of fluoride is constantly present, Streptococcus mutans produce less acid.12
CLINICAL EFFECTIVENESS
Numerous studies show that fluoride varnish and gel are effective in reducing tooth decay. In a summary by the United States Preventive Services Task Force, researchers reviewed six fluoride varnish studies and found statistically significant reductions in the number of tooth surfaces with cavitated lesions and a range of reduction in caries from 30% to 63%.13 A review of studies comparing fluoride varnish and acidulated phosphate fluoride (APF) gel concluded that the varnish was equally or more effective than the APF gel.14 Recently published ADA recommendations suggest using fluoride varnish as many as four times per year among high-risk children (under the age of 6) to achieve maximum effect and either fluoride gel or varnish four times per year for high risk individuals over 6 years of age.7 Fluoride varnish is especially recommended for the treatment of smooth surface noncavitated carious lesions8 and is endorsed by the ADA for caries prevention. However, this use is considered off-label because the Food and Drug Administration has only approved fluoride varnishes for the treatment of dentin hypersensitivity and as cavity varnish.
DENTIN HYPERSENSITIVITY
Dentin hypersensitivity is most likely caused by exposed dentinal tubules. The dentinal tubules are often exposed in cases of gingival recession; cervical wear; erosion from diet or conditions such as bulimia; or following periodontal or restorative procedures. The movement of tubule fluid most likely causes dentinal sensitivity. Topical fluorides are among several dental products that occlude and/or create a protective layer over the tubules, preventing movement of the tubule fluid.15 Fluoride applications have a dual effect on sensitive teeth because the protective layer of calcium fluoride is effective in tooth decay prevention and in eliminating tooth pain. In cases of sensitive teeth, topical fluoride gel can be gently burnished into the sensitive tooth surfaces before scaling and root planing to reduce treatment pain.16
THE RECIPIENTS
When used for caries prevention in children, the topical fluoride application is usually full mouth. In adults, lesion specific treatment is most common, with the intent to keep an existing lesion from progressing. The ADA Council on Scientific Affairs recently published guidelines for fluoride application.7 The guidelines are based on classifying patients into groups by their risk of developing caries (low, moderate, high) and their age.7 Low risk patients of any age living in fluoridated communities and using a fluoride dentifrice may not benefit from topical fluoride applications. Instead, these therapies should be targeted to patients of any age in the moderate or high risk categories with frequency of treatment depending on the level of risk. Presently, standard risk assessment tools are not available to practitioners. Assessment is based on clinical indicators that are predictive of future caries experience. These factors include whether or not the patient has experienced any incipient or cavitated lesion in the past 3 years combined with other factors such as xerostomia, high levels of cariogenic bacteria, poor oral hygiene, poor family dental health, eating disorders, drug or alcohol abuse, active orthodontic treatment, or physical or mental disabilities affecting the performance of oral care. These risks require reassessment periodically as they change over time and treatments should be adapted accordingly. The ADA Council also notes that research is lacking on the best regimen to follow in arresting caries.
SAFETY
Topical fluorides have been used for several decades and are safe when used appropriately. There is no evidence that professionally applied fluorides are a risk factor for enamel fluorosis in children. A study found no toxic effect on fluoride plasma levels or renal function in preschool or school-aged children treated with fluoride varnish.17 Additionally, the low plasma fluoride level following the application of fluoride varnish was comparable to plasma fluoride levels experienced after toothbrushing with a fluoridated dentifrice. The ADA recommends using fluoride varnish on children under 6 years due to the smaller amount of fluoride contained in varnishes.7
PRODUCTS AND APPLICATION
Three main topical fluoride vehicles are available for professional application: gel, foam, and varnish. The fluoride in gels and foams is either 1.23% APF containing 12,300 ppm fluoride ion or 2% sodium fluoride with 9,050 ppm fluoride ion. The active ingredient in fluoride varnish is 0.1% difluorsilane fluoride, which equals 1,000 ppm, or 5% sodium fluoride containing 22,600 ppm fluoride ion, which is more common.7
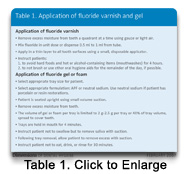
Fluoride gels are more common in the United States. In Europe, fluoride varnishes are preferred.18 Fluoride varnish is slowly growing in popularity in the United States.7 A study that examined the preferences of dental hygienists and patients in using fluoride varnish vs fluoride gel found that the dental hygienists preferred the fluoride varnish to gels for overall ease of application (see Table 1).19 Patients rated fluoride varnish preferable for comfort, time, and taste. Only half of the patients were bothered by the temporary discoloration of their teeth that accompanies the application of topical fluoride. Recently, a fluoride varnish has become available that is white in color and fruit flavored.
Fluoride foam is similar to fluoride gels and requires a smaller dose of application, thus minimizing the risk of ingestion. However, the ADA Council has not extended its recommendations for topical fluoride use to foams because only two clinical trials have been done that assess the effectiveness of fluoride foams. The clinical trials that looked at the efficacy of fluoride gel in reducing caries used a 4-minute application so, at this time, 1-minute applications are not recommended.7,18 The ADA recommendations do not make a distinction between APF and sodium fluoride gels because evidence does not indicate which one is more efficacious than the other. The two-part (APF and stannous fluoride) in-office rinses are not recommended because of the low fluoride concentration and lack of clinical trials establishing effectiveness.18
A number of trials show a 38% reduction in caries incidence with the use of fluoride varnish, predominately using a semi-annual application, in children.18 In a clinical trial directly comparing fluoride gels and varnishes, no difference in caries incidence between the varnish and APF gel was seen.18 The ADA Council recommendations are for the use of fluoride varnish in children under 6 years old.7 Ease of application in this population means a smaller dose is used and greatly lowers the likelihood of ingestion.
The Washington State Access to Baby and Child Dentistry program uses semi-annual applications of fluoride varnish for preschool children from birth to 5 years. For children too young to sit in a dental chair, a novel “knee to knee” technique can be used. Seated, the parent holds the child facing him or her and lays the child back on the knees. The clinician sits knee to knee facing the parent and leans over the child to perform an examination and applies the fluoride varnish.
Prophylaxis is not necessary prior to the application of topical fluoride and may actually be harmful. The procedure removes the outer, fluoride rich layer of enamel and results in less fluoride uptake from the topical application.5,18 Children and adolescents without calculus buildup should remove plaque by supervised brushing and flossing prior to topical fluoride application.
 A fourth type of topical fluoride for caries control—diammine silver fluoride (44,800 ppm)—is not available in the United States but has been used in several clinical trials in Asia. These studies show that it is effective at arresting caries.20 Esthetics are an issue as the demineralized dentin is darkened, however, it may have significant applications for treating root caries in the posterior dentition of geriatric patients and may be available in the United States in the future.
A fourth type of topical fluoride for caries control—diammine silver fluoride (44,800 ppm)—is not available in the United States but has been used in several clinical trials in Asia. These studies show that it is effective at arresting caries.20 Esthetics are an issue as the demineralized dentin is darkened, however, it may have significant applications for treating root caries in the posterior dentition of geriatric patients and may be available in the United States in the future.
XEROSTOMIA AND CARIES
Approximately 30% of those over the age of 65 have xerostomia.21 As longevity continues to increase, more seniors will experience salivary gland hypofunction. Although aging itself is not the cause of low saliva secretion, many medications and health conditions that occur in the elderly create xerostomia, thus increasing the risk for dental caries. Dental professionals are likely the first health professionals to detect the signs of xerostomia-induced caries and to provide appropriate treatment.
Topical fluoride application, fluoride mouthrinses, and chlorhexidine rinses are effective in reducing xerostomia-induced caries and oral infections in long-term care facilities for seniors. Currently, fluoride applications for seniors who do not reside in a facility are underused, yet xerostomia and tooth decay are prevalent in this group.21 Historically, the dental community has taken a reactive approach to salivary gland dysfunction. A proactive approach is necessary to maximize the prevention of caries and oral infections caused by xerostomia.
When nutrition is balanced and saliva secretions are normal, oral health is well-maintained and saliva flow is adequate to protect the teeth. However, individuals with medical conditions that reduce saliva production are at an increased risk for caries. People affected by Sjogren’s syndrome or radiation-induced xerostomia typically require the use of artificial saliva and topical fluoride treatments. Special needs patients often have minimal oral home care and may be taking multiple medications contributing to dry mouth syndrome. Other health conditions can cause some degree of xerostomia such as poorly controlled diabetes, medications, depression, urinary dysfunction therapies, cystic fibrosis, and obstruction or tumors of the salivary gland. Imbalances in oral health may also be caused by eating disorders, such as bulimia; gastrointestinal esophageal reflux disease (GERD); and poor nutrition. Health histories may be helpful in uncovering potential oral imbalances before damage to the oral tissues can result.22
Topical fluorides are highly underused in the United States especially in older people. Given that topical fluoride can not only prevent demineralization and promote remineralization of enamel but also reduce sensitivity, its use as a preventive and treatment measure should be widely promoted.
REFERENCES
- Borrell LN, Burt BA, Taylor GW. Prevalence and trends in periodontitis in the USA: the NHANES, 1988 to 2000. J Dent Res. 2005;84:924-930.
- Beltran-Aguilar ED, Barker LK, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis—United States, 1988-1994 and 1999-2002. MMWR Surveill Summ. 2005;54:1-43.
- Thomson WM. Dental caries experience in older people over time: what can the large cohort studies tell us? Br Dent J. 2004;196:89-92; discussion 87.
- Merck. Merck Institute of Aging and Health and the Centers for Disease Control and Prevention: The state of aging and health in America 2004. Available at www.cdc.gov/aging/pdf/State_of_Aging_and_Health_in_America_2004.pdf.
- Main PA, Lewis DW, Hawkins RJ. A survey of general dentists in Ontario, Part II: Knowledge and use of topical fluoride and dental prophylaxis practices. J Can Dent Assoc. 1997;63:607, 610-617.
- Forrest JL, Horowitz AM, Shmuely Y. Caries preventive knowledge and practices among dental hygienists. J Dent Hyg. 2000;74:183-195.
- Professionally applied topical fluoride: evidence-based clinical recommendations. J Am Dent Assoc. 2006;137:1151-1159.
- Newbrun E. Topical fluorides in caries prevention and management: a North American perspective. J Dent Educ. 2001;65:1078-1083
- Ten Cate JM, van Loveren C. Fluoride mechanisms. Dent Clin North Am. 1999;43:713-742.
- Featherstone JD. Prevention and reversal of dental caries: role of low level fluoride. Community Dent Oral Epidemiol. 1999;27:31-40.
- Hamilton IR. Biochemical effects of fluoride on oral bacteria. J Dent Res. 1990;69 Spec No:660-7; discussion 682-683.
- Marquis RE. Diminished acid tolerance of plaque bacteria caused by fluoride. J Dent Res. 1990;69 Spec No:672-675; discussion 682-683.
- Bader JD, Rozier RG, Lohr KN, Frame PS. Physicians’ roles in preventing dental caries in preschool children: a summary of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med. 2004;26:315-325.
- Seppa L. Fluoride varnishes in caries prevention. Med Princ Pract. 2004;13:307-311.
- Thrash WJ, Jones DL, Dodds WJ. Effect of a fluoride solution on dentinal hypersensitivity. Am J Dent. 1992;5:299-302.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 9th ed. Philadelphia: Lippincott Williams & Wilkins, 2004.
- Ekstrand J, Koch G, Petersson LG. Plasma fluoride concentration and urinary fluoride excretion in children following application of the fluoride-containing varnish Duraphat. Caries Res. 1980;14:185-189.
- Hawkins R, Locker D, Noble J, Kay EJ. Prevention. Part 7: professionally applied topical fluorides for caries prevention. Br Dent J. 2003;195:313-317.
- Warren DP, Henson HA, Chan JT. Dental hygienist and patient comparisons of fluoride varnishes to fluoride gels. J Dent Hyg. 2000;74:94-101.
- Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81:767-770.
- Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33:81-92.
- Navazesh M. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134:613-620.
From Dimensions of Dental Hygiene. February 2007;5(2): 16-19.

