 ZLIKOVEC / ISTOCK / THINKSTOCK
ZLIKOVEC / ISTOCK / THINKSTOCK
Facing the Challenge
Dental hygienists must be prepared to achieve positive outcomes in periodontal maintenance patients.
Periodontal maintenance is among the most challenging tasks faced by dental hygienists. From learning to critically evaluate the periodontal tissues, to discovering continuing periodontal attachment loss, to detecting residual calculus and performing often-blind scaling and root planing, periodontal maintenance requires dental hygienists to make maximal use of their skills.
Patients typically enter into periodontal maintenance after scaling and root planing (as definitive therapy), implant placement, or following periodontal surgery for chronic periodontitis. In every circumstance, dental hygienists must never lose sight of the fact that because some risk factors can’t be changed, periodontitis is rarely cured but, at best, may be merely controlled.1
Research has suggested that the progression of chronic periodontitis may be continuous or episodic.1 Thus,remaining vigilant for the early signs of renewed periodontal destruction is an important part of each maintenance appointment. When a patient’s periodontal status seems to be worsening, the dental hygienist must be prepared to take more aggressive steps to control the disease.
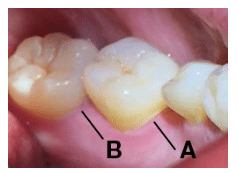
The first step in assessing periodontal status is accurately evaluating the gingival tissue for the presence of gingivitis. Gingival color changes are visible indicators of failing periodontal health, although such changes alone may not reflect ongoing periodontal attachment loss. In most patients, healthy gingiva has a coral pink color.2 Reddened or darker-than-normal gingival color may indicate chronic inflammation.2 Wilson et al3 evaluated root surfaces with the aid of a dental endoscope and discovered that in more than 60% of the areas that exhibited gingival color changes, the inflammation was associated with the presence of biofilm over subgingival calculus deposits that had been previously overlooked. The shape and tone of the tissue should also be used to identify areas where ongoing attachment loss may be present. The gingiva should be dried so the tissue texture can be evaluated. If the gingiva is shiny, enlarged, and spongy, the tissue is swollen. This may signal the likelihood of retained subgingival calculus as well as the possibility of continuing attachment loss (Figure 1).4
PERIODONTAL PROBING
Probing provides key information about health or disease. In nonsmokers, the repeated absence of bleeding on probing strongly suggests site stability. As such, attaining a consistent lack of bleeding on probing is an important therapeutic goal.5 However, the presence of bleeding on probing (or gingivitis) at a site that has previously lost attachment is not a reliable indicator of ongoing attachment loss. It may suggest gingivitis or retained subgingival calculus far coronal to the periodontal attachment apparatus. Charting of periodontal probings represents a moment in time. Therefore, at each periodontal maintenance appointment, updated measurements should be compared with previous readings to determine if a site appears to be experiencing additional attachment loss.
LINKING DISEASE WITH RESIDUAL CALCULUS
An important part of assessment is evaluating the pockets for residual calculus. Badersten et al6 reported that 44% of root surfaces in deep pockets exhibit residual calculus. Firm, moderate pressure should be used with up-and-down strokes when exploring the root surface. The first 1 mm to 2 mm of the explorer tip should be used to ensure proper adaptation to the root. Burnished calculus may be missed if only horizontal exploring strokes are used. The cementoenamel junction (CEJ) is particularly prone to retaining calculus. More apically, an up-and-down stroke may reveal burnished sheets of calculus that may be best detected on the downward or insertion stroke.7 Explorer selection is also important. A curved extended 11/12 explorer may be perfect for soft, spongy tissue but switching to the straight 3A explorer may be needed if the patient presents with firm tissue and deep pockets. Careful examination of furcations and grooves can reveal sheets of residual calculus. If these deposits are discovered during the assessment phase, action must be taken to remove them.
TECHNIQUE AND INSTRUMENT SELECTION
Once detected, residual calculus may be difficult to remove due to limited access or tooth anatomy that impededs instrumentation. Even when access is possible, circumstances are made more difficult when clinicians use worn ultrasonic inserts/tips or do not have appropriate instruments available in their armamentariums. Selecting the best instrument for the task at hand, as well as implementing the appropriate techniques are integral to the effectiveness and efficiency of periodontal maintenance appointments. Prior to instrumentation, the need for pain control should be assessed. The use of intrapocket topical anesthesia or injected local anesthetic should be used when indicated.
The armamentarium for effective periodontal maintenance should include the following: rigid Gracey curets to remove more tenacious sheets of burnished calculus and extended-shank Gracey curets to reach the base of deep periodontal pockets (typically 5 mm or greater).8–10 Clinicians may also elect to use mini-bladed Gracey curets to improve adaptation to root contours, deep proximal concavities, narrow convexities, depressions on multirooted teeth, and furcations. Micro-mini Gracey curets can be used to access the narrowest of root contours and furcations. A recent addition to the instrumentation armamentarium—periodontal maintenance Gracey curets—may be used to remove biofilm or soft calculus on teeth with tight tissue, recession, or residual pocket depths. Periodontal maintenance Gracey curets have rigid shanks so they can withstand the firm pressure required when removing residual calculus. The shank length is 2 mm—longer than the standard Gracey curet but 1 mm shorter than the extended-shank Gracey curet. This is to improve access to molar areas with attachment loss while still enabling ease of use in the anterior areas where a longer shank is seldom necessary.
Tight tissue with narrow deep pockets are challenging to effectively instrument. Proper instrumentation techniques are required to thoroughly remove all calculus found on the roots of periodontal maintenance patients. Extended-shank instruments are useful for reaching deep pockets with moderate to severe recession. However, when the tissue is tight and insertion is difficult, periodontal maintenance Gracey curets may allow better access to the base of the pocket. The shank angle of the periodontal maintenance Gracey 11/12 is between the regular Gracey 11/12 and the Gracey 15/16. The shank angle of the Gracey 13/14 is between the regular Gracey 13/14 and the Gracey 17/18. Standard mini-bladed Gracey curets are useful on lingual and facial surfaces, particularly on the anterior teeth due to their short, thin blades.2 Rigid mini-bladed Gracey curets are sometimes too thick to insert subgingivally under tight tissue. If this is a problem, choose standard mini-bladed Gracey curets, micro-mini bladed Gracey curets, or periodontal maintenance Gracey curets. For deep mesial or distal pockets, if a mini or micro-mini Gracey curet blade feels too short to effectively reach across the proximal surface, select a periodontal maintenance Gracey 11/12 or 13/14 and activate vertical or oblique strokes. The three-quarter length blade will extend further across the surface, and the tip of the modified Gracey 13/14 is specially curved to enhance adaptation to distal concavities.
Mini-bladed Gracey curets are best suited to replace conventional Gracey curets in areas that are difficult to access, such as furcations, line angles, and deep, tight, narrow pockets—especially on facial and palatal surfaces. They can be positioned with the toe directed mesially or distally for vertical strokes on buccal or lingual surfaces. Mini-bladed Gracey curets are generally used with straight vertical strokes. They may also be implemented with oblique or horizontal strokes but due to the shortness of the blade, these strokes might not extend far enough subgingivally unless the tissue is easily retracted. Horizontal strokes with mini-bladed Gracey curets are most effective when limited to use along the CEJ or in root depressions just below gingival margins.1 Rigid mini-bladed Gracey curets are best used for initial therapy procedures when strong lateral pressure must be applied during debridement.11 All instruments should be of medium or fine thickness for adequate access into the pocket. Also, correct sharpening technique is necessary to ensure instruments are sharp enough to remove calculus.
Ultrasonic instrumentation may be helpful in removing residual calculus. Some thin inserts are designed to slip under tight tissue into narrow pockets. Beveled thin tips can also reach to the base of narrow pockets to pulverize residual calculus. When using ultrasonic instrumentation, clinicians must be aware that using worn inserts/tips will prevent them from effectively removing calculus.12
CONCLUSION
Periodontal maintenance appointments are opportunities to assess patients’ gingival and periodontal conditions. Adequate time—at least an hour—is needed to perform a thorough evaluation and instrumentation. Knowing when to refer is also important. If a periodontal site is deteriorating, the patient should be referred to a periodontist. Carranza suggests patients should be referred when pocket depth is increasing, if there are areas that are difficult for both the clinician and patient to keep clean, or unresolved gingival inflammation is present.1 A wide range of instrument designs, as well as improved assessment skills will aid clinicians in their quest to achieve successful treatment outcomes for periodontal maintenance patients.
References
- Carranza F. The periodontal pocket. In: Carranza’s Clinical Periodontology. 12th ed. St. Louis: Saunders: 2015.
- Carranza F. Phase 1 periodontal therapy. In: Carranza’s Clinical Periodontology. 12th ed. St. Louis: Saunders; 2015.
- Wilson TG, Harrel SK, Nunn ME, Francis B, Webb K. The relationship between the presence of tooth-borne subgingival deposits and inflammation found with a dental endoscope. J Periodontol. 2008;79:2029–2035.
- Wilkins EM. Instruments and principles for instrumentation. In: Clinical Practice of the Dental Hygienist. 11th ed. Philadelphia: Lippincott Williams and Wilkins; 2013.
- Lang NP, Joss A, Orsanic T, Gusberti FA, Siegrist BE. Bleeding on probing. A predictor for the progression of periodontal disease? J Clin Periodontol. 1986;13:590–596.
- Badersten A, Nilvéus R, Egelberg J. Scores of plaque, bleeding, suppuration and probing depth to predict probing attachment loss. 5 years of observation following nonsurgical periodontal therapy. J Clin Periodontol. 1990;17:102–107.
- Hodges MK. A close-up look at explorers. Dimensions of Dental Hygiene. 2013:11(9):34–38.
- Pattison AM, Pattison GL. Periodontal Instrumentation. 2nd ed. Upper Saddle River: New Jersey: Pearson Prentice Hall; 1992.
- Nguyen M. A closer look at the 13/14 Gracey curet. Dimensions of Dental Hygiene. 2015;13(9):24–30.
- Pattison AM. The use of hand instruments in supportive periodontal treatment. Periodontol 2000. 1996;12:71.
- Matsuda S. Instrumenting biofilm. Dimensions of Dental Hygiene. 2003;1(1):26–30.
- Hodges MK. The power of selection. Dimensions of Dental Hygiene. 2013:11(1):42–46.
From Dimensions of Dental Hygiene. May 2016;14(05):24,26,28.

