 SANTYPAN/ISTOCK/GETTY IMAGES PLUS
SANTYPAN/ISTOCK/GETTY IMAGES PLUS
Extend Your Reach During Nonsurgical Periodontal Therapy
Focusing on deep periodontal pocket topography can aid dental hygienists in selecting appropriate hand instruments and providing effective treatment.
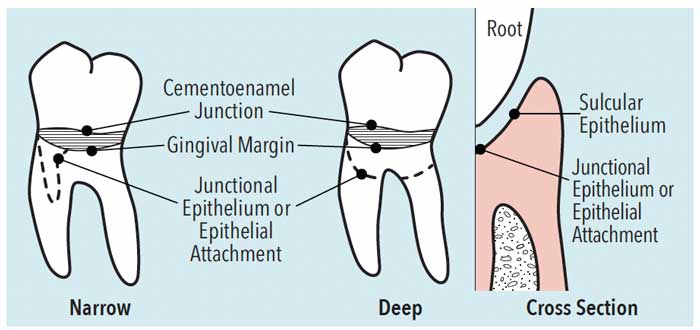
Extended shank instruments are indicated for deep periodontal pocket depths greater than 5 mm as measured with a periodontal probe. Deep periodontal pocket depth can be complex in regard to shape; however, for simplification, deep periodontal pockets can be thought of as narrow or wide topography, ie, shape and surface area (Figure 1). The topography of the periodontal pocket includes its circumference defined by the tooth surface (root), sulcular epithelium of the free gingiva, and the junctional epithelium (Figure 1). Critically thinking about periodontal pocket depth topography helps the clinician choose the appropriate hand-activated instruments and techniques.
Instrument Selection
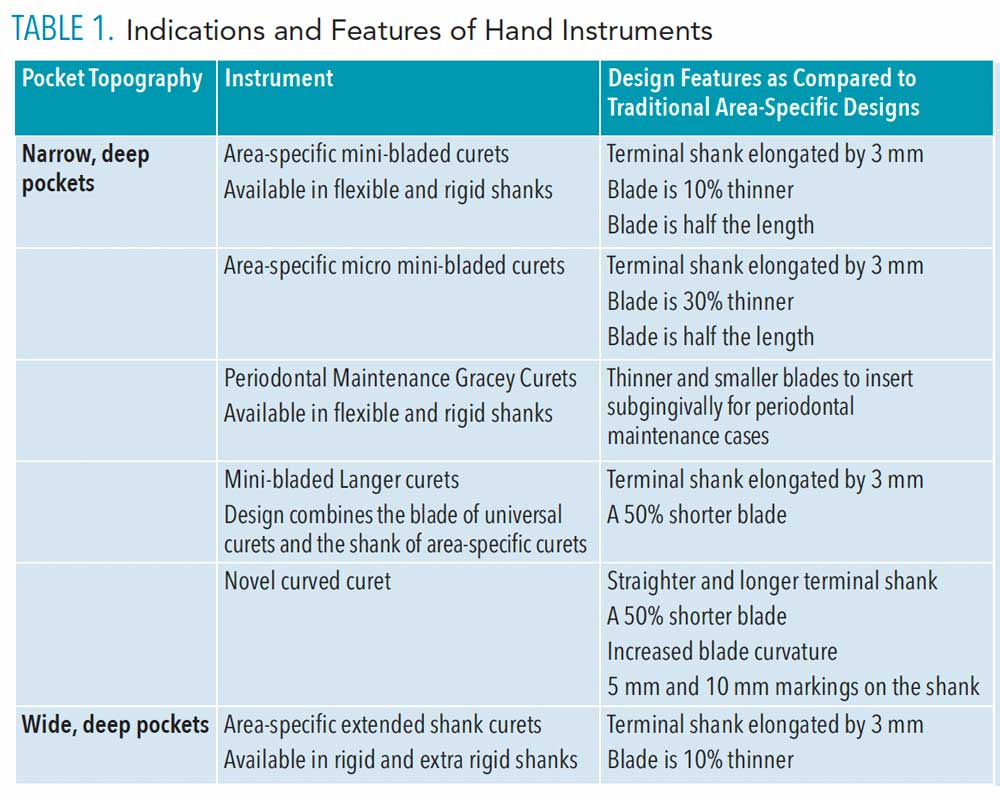
Narrow, deep periodontal pockets. Instruments with long shanks and narrow, short working ends are indicated for narrow, deep periodontal pockets. These include area-specific mini-bladed curets (Figure 2), area-specific micro mini-bladed curets, area-specific periodontal maintenance curets, mini-bladed Langer curets, and novel curved curet (Table 1).

Interestingly, Proveli et al1 found that manual instrumentation with mini-bladed curets resulted in a more homogeneous post-operative root surface with fewer root alterations when compared to power instruments. Also noted were the similar effects of mini-bladed curets and slim piezoelectric tips on calculus removal.1 A systematic review revealed that when periodontal pocket depths were 6 mm or greater, manual subgingival scaling was superior to ultrasonic instrumentation in regard to periodontal pocket depths and reductions in clinical attachment loss.2 These studies demonstrate the value of using hand-activated instruments to finish root surfaces, and of following ultrasonic instrumentation with hand-activated curets during nonsurgical periodontal therapy.
Traditional, standard curet designs might not be the best choices for narrow, deep periodontal pockets. Traditional instruments include the Columbia 13/14 and 4R/4L, Barnhardt 1/2 and 5/6, and McCall 13/14 or 17/18 universal designs and the Gracey curet area-specific designs (1/2 though 17/18). The correct adaptation and activation of these designs are challenging in narrow, deep periodontal pockets because it is difficult to extend the working end subgingivally 5 mm or more due to the shorter shank length than extended shank instruments. Also, the long and wide working end of universal and area-specific curets would be difficult to adapt and activate subgingivally when pocket space is limited.
 While the patient may be anesthetized, using a blade that is too long and wide increases the likelihood that the cutting edge or toe will impinge on tissue within the pocket wall. This impingement (ie, trauma) could translate into unnecessary sensitive gingival tissue post-instrumentation.
While the patient may be anesthetized, using a blade that is too long and wide increases the likelihood that the cutting edge or toe will impinge on tissue within the pocket wall. This impingement (ie, trauma) could translate into unnecessary sensitive gingival tissue post-instrumentation.

Wide, deep periodontal pocket depths. When working in wide, deep periodontal pocket depths, instruments with long shanks and long and wide working ends should be used to extend to the epithelial attachment (Figure 2). These types of curets include extended-shank curet designs with a longer shank and thinner blade than most traditional universal and area-specific curets (Figure 3). Also, Langer curets feature a 3 mm extension of the terminal shank and a thinned blade that allows for easy insertion. Although mini- and micro mini-bladed curets can be used to reach the most apical portions in wide-shaped pockets, selecting a longer shank with a wider, longer blade might be more efficient in scaling and root planing (Figure 4).
Use of only mini- and micro mini-bladed instruments in wide-shaped pocket depths will be less efficient due to the short cutting edges that adapt to a very small area of the root. However, if a clinician is adapting to specific root anatomy within wide, deep periodontal pockets, such as concavities or grooves, mini-bladed curets, micro mini-bladed curets, periodontal maintenance curets, and novel curved curets are ideal choices. Therefore, clinicians need an array of instrument designs to meet patient needs in nonsurgical periodontal therapy and periodontal maintenance care.
Instrument Adaptation and Activation
Narrow, deep periodontal pockets. Consider that instrumentation within this topography will be limited due to the narrow width, from side to side, of the pocket. For this reason and because of the deep pocket depth, mini-bladed curets, micro mini-bladed curets, periodontal maintenance curets, Langer mini curets, and novel curved curets will adapt best. These instruments will be inserted into the pocket in a vertical fashion to extend to the epithelial attachment. In other words, the terminal shank will be adapted to the long axis of the root (Figure 5). Also, because the blade is short, most of it will be adapted to the root surface. Therefore, about a millimeter of the cutting edge will be activated at a time within a sequence of working strokes.

To activate appropriately, a vertical or slightly oblique stroke is usually used at a 70° to 80° blade angle to the root. Not much space is available to vary stroke direction; therefore, it is unlikely that oblique or horizontal strokes will be effective in this situation. Reassessment with the curet will occur often with short overlapping strokes. Also, an extended shank explorer (11/12 design) with a 3-mm longer terminal shank and a short working end is an ideal choice for deep, narrow periodontal pocket depths (Figure 6). A traditional explorer might not permit extension to the epithelial attachment, resulting in calculus on the root surface in the deepest portion of the pocket to be undetected. Although deep, narrow periodontal pockets might occur on any surface, common locations are at line angles, on the facial or lingual of a single root, proximally, adjacent to furcation involvement, or on the lingual of maxillary anterior teeth.
Wide, deep periodontal pocket depth. With this wide topography, space between the pocket walls is greater than the narrow pocket; however, it is still restricted. The extended shank area-specific curet in wide, deep periodontal pockets is adapted by placing the terminal shank vertical to the long axis of the root (Figure 7). However, space may be available to permit the working end to be adapted vertically to the long axis of the root to activate a horizontal stroke (Figure 8). This manner of adapting the curet optimizes crosshatching (overlapping) of strokes.3 In this case, caution is used to avoid adapting the toe against sulcular epithelium or into the epithelial attachment, which could cause trauma and discomfort. Adapting the curet in this manner is advantageous for deposit removal adjacent to the cementoenamel junction and in the subgingival developmental depressions on the root.4 In deep periodontal pockets, reaching the epithelial attachment with this approach is not possible; however, the working end can be extended subgingivally as far as the blade’s length (Figure 8).

The terminal 1 mm to 2 mm of the blade will be adapted and channeling of the surface will occur. Channeling is the removal of deposits via short 1 mm to 2 mm incremental and overlapping strokes.5–7 These strokes travel across each small section of the root surface in oblique, vertical, and horizontal directions to channel calculus until an entire deposit is removed. Therefore, the activation across the root surface can be somewhat time consuming if the entire root is to be instrumented. Use of too much of the blade during a working stroke can result in ineffective deposit removal, especially in grooves, on concave surfaces, and around convex surfaces.
Reassessing the root surface is constantly achieved by using the curet with an exploratory stroke that is light and slightly longer than the channeling working strokes. Reassessing the root surface after debridement and root planing will also occur with an extended shank explorer to determine the endpoint. Wide, periodontal pockets can occur on any surface of a single or multirooted tooth.
Additional Strategies in Deep Periodontal Pockets
Additional strategies for instrumentation in deep periodontal pockets include the use of alternative fulcrums, measurement of the instrument’s shank, reassessing shank strength, and the application of files. When fulcruming for stability, consider adapting the instrument to the depth of the epithelial attachment first, and then moving the instrument grasp on the handle to obtain a fulcrum on hard tissue or soft tissue if need be. Often the fulcrum will be placed on the opposite arch to gain access to the deepest portions of the periodontal pocket and to maintain stability during an effective working stroke for calculus removal (Figure 5 and Figure 6).

If in doubt about the length of the instrument shank and its ability to adapt to the depth of a periodontal pocket, measure the shank of the curet or explorer with a periodontal probe. The length can then be compared to the periodontal probe readings charted during assessment. Novel curved curets provide measurements on the shank of the instrument in order to apply this principle.
The strength or rigidity of the shank is also a consideration in both narrow and wide deep periodontal pockets. A rigid shank might be needed because the calculus is tenacious, whereas a flexible shank is indicated for light to medium nontenacious deposits and plaque biofilm removal. Another option for removal of tenacious calculus is a Hirschfeld file with a small, narrow, flat head. The 3/7 is indicated for buccal and lingual surfaces and the 5/11 is indicated for mesial and distal surfaces.
The effectiveness of various hand-activated instruments is difficult to assess by research due to the many variables that affect instrumentation results. There is, however, some research about extended shank instruments. A novel curved curet was found to remove more of the subgingival tooth material from an incisor than a conventional curet.8 The instrument exhibited superior material removal on all root surfaces with 4 mm to 6 mm clinical attachment levels while causing a rougher surface than a conventional curet.9 The novel curved curet also produced furcation root surfaces with significantly less residual deposits than ultrasonic inserts/tips, indicating the potential value of small-bladed curets in debriding involved furcations.10

Another study evaluated the effectiveness of subgingival scaling and root planing with longer shank, thinner blade, rigid curets compared to the standard rigid Gracey curet, and found no significant difference between the two. The mesial surfaces had the least remaining calculus and best curet efficiency.11

Conclusions
While deep periodontal pocket depth can be complex and challenging to instrument, thinking about deep periodontal pockets as either narrow or wide for simplicity in selection, adaptation, and activation of manual instrumentation may be helpful. Access to root surfaces and effectiveness of hand-activated instruments in deep periodontal pockets depend on many factors such as gingival inflammation, pain management, area of the mouth, tooth surface, root anatomy, and single vs multirooted teeth. However, concentrating on deep periodontal pocket topography can aid the clinician in selecting appropriate instruments and providing efficacious nonsurgical periodontal therapy and periodontal maintenance. Use of inappropriate instruments for a clinical situation might result in incomplete deposit removal that interferes with healing despite a patient’s adequate self-care.
References
- Profili F, Sparabombe S, Tawse Smith A, D’Isidoro O, Quaranta A. The effect of miniaturized manual versus mechanical instruments on calculus removal and root surface characteristics: an in vitro light microscopic study. Clin Exp Dent Res. 2019;5:519–527.
- Zhang X, Hu Z, ZHU X, et al. Treating periodontitis-a systematic review and meta-analysis comparing ultrasonic and manual subgingival scaling at different probing pocket depths. BMC Oral Health. 2020;20:176.
- Hodges KO. Maximize the working stroke. Dimensions of Dental Hygiene. 2015;13(7):32–36.
- Beleno Sanchez J, Nguyen M. Improve nonsurgical periodontal therapy with appropriate instrument choice. Dimensions of Dental Hygiene. 2021;19(2):16–21.
- Pattison G, Pattison AM. Periodontal Instrumentation: A Clinical Manual. Reston, Virginia: Reston Publishing Co; 1979:91.
- Hodges KO. Channeling for success, part 1. Dimensions of Dental Hygiene. 2013;11(5):34–37.
- Hodges KO. Incorporating channeling into instrumentation. Dimensions of Dental Hygiene. 2013;11(7):36–38.
- Singer Dl, Long BA, Lozanoff S, Senthilselvan A. Evaluation of a new periodontal curet: an in vitro studyJ J Clin Perio. 1992;19:549–552.
- Landry C, Long B, Singer D, Senthilselvan A. Comparison between a short and a conventional blade periodontal curet: an in vitro study. J Clin Periodontol. 1999;26:548–551.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular first molar furcations. II. Furcation area. J Periodontol. 1997;68:1098–1011.
- Nagy RJ, Otomo-Corgel J, Stambaugh R. The effectiveness of scaling and root planing with curets designed for deep pockets. J Periodontol. 1992;63:954–959.
From Dimensions of Dental Hygiene. October 2021;19(10)22-25.

