Ensuring Safe Practice In Dental Radiology
Minimizing radiation exposure and adhering to appropriate infection control procedures are integral to the safe use of dental radiography.
Dental professionals are responsible for ensuring minimal radiation exposure through adopting the principles of “as low as reasonably achievable,” or ALARA. Individuals who operate dental X-ray equipment need to understand the associated health risks of radiation, as well as the rules and regulations of radiation safety. Abiding by equipment guidelines and adhering to infection control standards to prevent the spread of disease are also important in the safe capture of radiographs.
Following the ALARA principal begins with adhering to the selection criteria for prescribing dental radiographs. These provide intervals for type and frequency of radiographs tailored to a patient’s disease status and history.1 Selection criteria also consider radiation exposure history when determining the appropriate number and frequency of dental radiographs. To minimize unnecessary exposures, dental professionals should use their judgment and the United States Food and Drug Administration (FDA)/American Dental Association (ADA) selection criteria guidelines, which call for a comprehensive examination, complete health history, oral disease risk assessment, and review of recent oral radiographs.1 Research has found a 43% decrease in dental radiographic exposures when implementing the selection criteria guidelines into practice.1 While the prescription of X-rays ultimately rests with the dentist of record, dental hygienists need to be familiar with the guidelines as they are typically responsible for exposing oral radiographs.1
Radiation safety necessitates the use of precautions to ensure adequate protection for all individuals. This is because X-rays are a form of ionizing radiation that can disrupt the basic building blocks of human cells.1 Commitment to the ALARA standard for all radiographic exposures is important because the long-term effects of low-dose radiation are unknown. Clinicians should keep a distance of 6 feet and maintain a 45° angle from the source of radiation at all times unless an appropriate barrier is in place.2 They also need to provide patients with thyroid shielding before taking intraoral radiographs because small amounts of X-ray radiation can be deflected or reflected from any encountered mass.3 Such deflection and reflection, or scatter permits X-ray radiation to reach other radiosensitive organs. Lead aprons with thyroid collars largely prevent scatter-based exposure of most radiosensitive tissues, including those found in the reproductive glands, thyroid gland, and bone marrow. The amount of radiation used in typical dental radiography, however, is small.
While the use of lead aprons with thyroid collars is not required when optimal rectangular collimation is implemented, according to the National Council on Radiation Protection & Measurements (NCRP) and the ADA,3 dental professionals still may want to consider standard usage, especially when film is used. A rectangular collimator can be placed on the X-ray unit’s position indication device (PID) to reduce scatter radiation exposure up to five times compared with a circular collimator. The use of an image receptor holding device is recommended to avoid cone cut, as there is minimal room for centering errors with a rectangular collimator.1
Digital imaging techniques require less radiation than conventional E/F speed film-based methods.1 Shielding patients remains prudent, however, when digital radiography is used. Thyroid collars are required at all times except when they interfere with extraoral imaging or additional collimation is implemented.3 Lead-free aprons and lightweight options are now available that may offer improved comfort than previous designs. Zuguchi et al4 found that the protection offered by lead and nonlead shielding was comparable. However, potentially higher radiation transmission levels were noted when lead-equivalent aprons were compared to pure lead aprons.5 Dental professionals should ensure that the shielding method protects at the tube voltages used for dental X-rays—typically 60 kilovoltages to 70 kilovoltages.
Other measures to reduce radiation exposure include the use of control panel exposure charts and long PIDs. Exposure charts can be created by referencing the X-ray device’s manual for tube potential, current, and time (or impulses), and anatomical location. Less radiation is necessary for low-density areas (anterior teeth and jaws), and more radiation is needed to penetrate high-density locations (posterior teeth and jaws). Exposures can be preset by location on the control panel or listed on a reference chart by the X-ray control panel for easy access.1 Long PIDs can reduce radiation exposure by 10% to 25% when compared to short PIDs. In addition, maintaining safe dental X-ray machines requires periodic inspection and may necessitate repeated recertification by relevant governmental authorities. This helps ensure equipment is properly functioning and all safety controls are working.
Dental professionals exposing radiographic images must consider their accumulated occupational exposure over time. Personal dosimeters—devices that measure accumulated amounts of ionizing radiation—are required for operators whose yearly dose is expected to exceed 1 mSv and women who are pregnant.1 Oral radiographers should never hold image receptors for patients. If a patient is unable to hold an image receptor intraorally, the dental professional should ask the parent/guardian or accompanying adult to help. This assistant must wear an operator shield throughout the radiographic examination.
HANDHELD X-RAY UNITS
Portable, handheld X-ray devices increase convenience due to their mobility, and they are compatible with film, indirect (photostimulable phosphor plates, or PSP), and direct digital imaging procedures.6–8 Studies have not found that handheld devices emit more radiation than wall-mounted units.1 The external backscatter shield on handheld devices protects the operator from backscatter radiation when used with the operator positioned directly behind the shield with both hands on the portable X-ray device.1,3 When increased or decreased angulations are needed to expose periapical and occlusal intraoral images, the protection provided by the backscatter shield may not be adequate. A backscatter shields must be permanently affixed and the device should not be used if the shield is broken or dislodged. Interestingly, the NCRP does not recommend using portable X-ray devices when wall-mounted units are available and patient conditions allow for proper utilization.3 This recommendation may be based on the frequent need to capture radiographs in atypical positions. Dental professionals may want to consider wearing protective shielding and personal dosimeter badges if the handheld X-ray device is used atypically. Clinicians should ensure that the handheld X-ray device is cleared by the FDA by checking for certification and warning labels on the device itself.9 Portable X-ray equipment must be kept in locked cabinets, storage rooms, or work areas with the batteries removed when not in use.1
INFECTION CONTROL
Maintaining adequate infection control during dental radiology is critical to safe patient care. Infection control protocols must consider all equipment and exposed surfaces that may become contaminated during the exposure of intra- and extraoral radiographs. The risk of cross-contamination is high if proper aseptic techniques are not implemented. This is because of contaminated gloves and the possibility of splatter from saliva or other fluids onto the many high-touch areas used when performing dental radiography. Oral microorganisms can remain viable on radiology equipment for up to 48 hours. The Centers for Disease Control and Prevention recommends that personal protective equipment be worn when dental professionals expose oral radiographic images to prevent self- and cross-contamination. In addition, an Environmental Protection Agency (EPA)-registered disinfectant of low- to intermediate-level activity must be used to clean and disinfect surfaces that may become contaminated by bodily fluids during the radiographic examination. Radiology equipment or devices that come into contact with mucous membranes are considered semicritical items and include direct and indirect digital image receptors and external aiming devices and accessories. Semicritical items should be heat sterilized. High-level disinfection is required for heat-sensitive items.10
Asepsis must be maintained with computer equipment associated with the radiologic process. Liquid-proof keyboards and mice allow for liquid disinfection between patients. Disinfecting wipes can also be safely used on many keyboards. Covering the keyboard and mouse with a barrier shield so a gloved clinician does not cross-contaminate the equipment is ideal. Barrier sheathing is required for keyboards that cannot be subjected to disinfectants. The entire tube head, exposure controls, chair and chair controls, work area, lead apron, and thyroid collar should be cleaned and disinfected between patients. To prevent lead apron contamination, it should be placed and removed with clean, ungloved hands before the patient is touched. Foot pedal controls may also help minimize contamination risk.
Digital image receptors should be cleaned, disinfected, and heat-sterilized between patients. Manufacturers should be consulted regarding appropriate disinfection/sterilization procedures for direct digital sensors. Recommendations for digital image receptors generally include the proper use of FDA-cleared barrier-sheaths before intraoral placement and utilization of high-level chemical disinfectant after intraoral placements. Unless wireless sensors are used, protective sheaths need to cover both the sensor and wire connectors.
Hokett et al11 conducted a cross-contamination study on direct digital sensors and barrier-sheath leakage with and without an additional protective layer using a water pressure test. Results indicated a 44% to 51% leakage rate in the barrier-sheaths after one-time intraoral placement; only 6% of the direct digital sensors with additional protection leaked after single intraoral placement. Dental professionals exposing intraoral radiographs during highly invasive dental procedures should consider using a double-barrier system to better prevent cross-contamination. The study also emphasized the need to clean and disinfect image receptors with EPA-registered hospital disinfectant after removal of the barrier sheath between patients.11
CONCLUSION
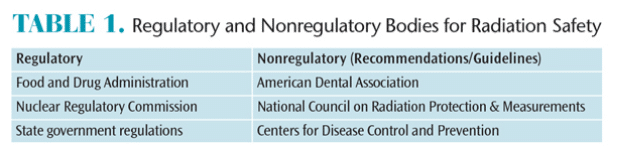
Government regulations and nonregulatory recommendations should be considered and implemented to ensure optimal radiation safety is being practiced.1 Table 1 provides a summary of agencies for further reference regarding radiation safety practices. The effects of radiation accumulate from various sources;12 therefore, a risk-vs-benefit ratio must be used when determining whether dental radiographs are necessary.1 Proper infection control procedures for radiography devices must be followed to limit the risk of cross-contamination. Dental professionals should be familiar with and observe their state’s policies and procedures regarding ionizing radiation and infection control.
References
- American Dental Association Council on Scientific Affairs, United States Food and Drug Administration. Dental Radiographic Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure. Available at: ada.org/~/media/ADA/Member%20Center/FIles/Dental_Radiographic_Examinations_2012.ashx. Accessed November 19, 2015.
- NCRP Report No. 145, Radiation Protection in Dentistry. Bethesda, Maryland: National Council for Radiation Protection & Measurements; 2003.
- McDaniel T, Parashar V. Comparison of state dental radiography safety regulations. Gen Dent. 2015;63:67–72.
- Zuguchi M, Chida K, Taura M, et al. Usefulness of non-lead aprons in radiation protection for physicians performing interventional procedures. Radiat Prot Dosimetry. 2008;131:531–434.
- Christodoulou EG, Goodsitt MM, Larson SC, Darner KL, Satti J, Chan HP. Evaluation of the transmitted exposure through lead equivalent aprons used in a radiology department, including the contribution from backscatter. Med Phys. 2003;30:1033–1038.
- Newcomb T, Bruhn A, Giles B. Critical issues: mass fatality incidents and the role of the dental hygienist, are we prepared? J Dent Hyg. 2015;89:143–151.
- Pittayapat P, Thevissen P, Fieuws S, Jacobs R, Williams G. Forensic oral imaging quality of handheld dental X-ray devices: Comparison of two image receptors and two devices. Forensic Sci Int. 2010;194:20–27.
- Danforth RA, Herschaft EE, Leonowich JA. Operator exposure to scatter radiation from a portable hand-held dental radiation emitting device (aribex nomad) while making 915 intraoral dental radiographs. J Forensic Sci. 2009;54:415–421.
- Mahdian M, Pakchoian AJ, Dagdeviren D, et al. Using hand-held dental x-ray devices: ensuring safety for patients and operators. J Am Dent Assoc. 2014;145:1130–1132.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for Infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52:31.
- Hokett SD, Honey JR, Ruiz F, Baisden MK, Hoen MM. Assessing the effectiveness of direct digital radiography barrier sheaths and finger cots. J Am Dent Assoc. 2000;131:463–467.
- NCRP Report No. 160, Ionizing Radiation Exposure of the Population of the United States. Bethesda, Maryland: National Council for Radiation Protection & Measurements; 2009.
From Dimensions of Dental Hygiene. December 2015;13(12):30,32–33.