 YURI_ARCURS/ISTOCK/GETTY IMAGES PLUS
YURI_ARCURS/ISTOCK/GETTY IMAGES PLUS
Ensure Proper Fit
Implementing well-fitting loupes into clinical practice can improve both ergonomics and the quality of patient care.
Clinical practice often creates physical stress on oral health professionals whose work involves fine repetitive movements and prolonged static postures, increasing their risk for musculoskeletal disorders (MSDs).1–3 Ergonomics has become an important topic, as MSDs threaten work productivity, income, career longevity, and overall health.1 The use of dental loupes demonstrates great promise in enhancing quality of care and ergonomic wellness. An important goal of magnification is to decrease neck flexion and promote neutral body posture demonstrated by a clinician’s straight back and spine.4–7 In dental hygiene practice, it is natural to tilt the head to get a closer view of extra- and intraoral structures, forcing the clinician into non-neutral head and neck postures. As such, better visual acuity through magnification may reduce eye strain and enhance assessment of hard and soft tissues. The use of loupes may make subtle tissue changes more discernable and improve visual evaluation of supragingival calculus, the gingival margin, caries, radiographs, periodontal probe readings, and clinical attachment levels, resulting in better diagnosis and care.6,7
Today, the use of loupes has become an integral part of contemporary practice. Several varieties of frame material and colors, wired and wireless lights, and differing magnification strengths are available. Traditional front-lens-mounted (FLM) or through-the lens (TTL) loupes are most commonly worn by dental hygienists.8,9 Ensuring a proper fit for loupes is integral to their successful use. Four ergonomic factors should be considered when determining the appropriate fit for loupes: working distance, depth of field, declination angle, and co-axial alignment.10–12 These concepts will help clinicians evaluate the custom fitting process and they emphasize the importance of accurate measurements. Some types of poorly fitted FLM and TTL loupes may actually contribute to neck strain or cervical MSDs.5,9,10
WORKING DISTANCE AND DEPTH OF FIELD
Working distance is the amount of space between the clinician’s eyes and the work area.13,14 To determine optimal working distance, measure the closest and farthest distance where an object remains in focus.5 If the working distance is too short, this may force the clinician to hunch over the patient or it may result in excessive neck flexion. Optimal working distance should be measured while simulating treatment, as this gives the most accurate neutral hand placement.10,11 The patient’s mouth should be at or close to elbow level. While the arms and hands are simulating treatment, the distance from the eye to the mouth should be measured at commonly used clock positions.11
Depth of field is the range in which an object stays in focus as the clinician moves closer and farther away from the oral cavity.10,11This will vary by magnification strength with higher magnification resulting in a smaller depth of field range.11 If the depth of field is accurate, the clinician should be sitting upright and not hunching over at the neck and back.
DECLINATION ANGLE
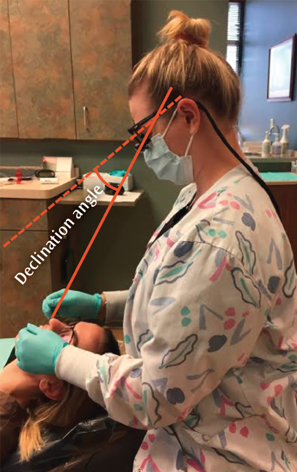
The declination angle is the angle between the physiological support line of a clinician’s spectacles-mounted system and the actual line of sight chosen by the clinician.10 In other words, from the arm of the loupes as it sits on the ear to where the loupes rest on the nose (Figure 1).10 The declination angle has become an important factor in loupes selection, as it specifically relates to neck flexion.11,15–17 Rucker et al18 first examined the declination angle using a specially designed frame that measured four parameters for precise angling of surgical telescopes. They found declination angles ranged from clinician to clinician. As such, the declination angle must be accurately measured for each clinician to ensure proper ergonomics for the neck and cervical region.9 Valachi11suggests that many of the loupes on the market are not ergonomic, placing the clinician in a forward head tilt greater than the recommended 20°.
Traditional TTL loupes have the telescopes drilled into the lens, with a prefixed declination angle. Flip-up loupes have telescopes mounted on a hinge, which may offer an ergonomic advantage, as the declination angle is steeper and can sometimes be adjusted. Peer-reviewed research, however, is needed to examine this issue.
The declination angle of custom loupes should be equal to the downward rotation angle of the eyes, which is required to see while working at an optimal hand position. While there are no clear guidelines for determining declination angle, similar methods are suggested for finding optimal declination angle.10,15 The clinician must first remove any safety or prescription glasses and sit balanced on the operating chair. To find the optimal hand position, bring the hands to a balanced and relaxed working position. Move the patient’s oral cavity to this optimal hand position for measurement purposes. Next, a balanced head position must be found by holding the head in the least strained posture. The clinician should look downward at the hand position previously determined and keep the eyes focused on this point. Then, the clinician should rock the head forward and downward until neck strain is felt. Raise the head until eye strain is felt while looking down at the hand position. While looking at the hands, tip the head forward and backward a few times through the range of motion until a balanced head position is attained. This position helps to derive the optimal line of sight and declination angle.10
Another approach is to use pictures and protractor measurements, instead of just relying on the feeling of muscular strain.15 The minimum and maximum rotation angles of the eyes can be found to determine the optimal declination angle. Appropriate declination angle lies between these two extremes.
DECLINATION ANGLE OF CURRENT LOUPES
Evaluating the declination angle of a practitioner’s current loupes may help to determine if loupes are ergonomically optimal or straining the neck and cervical region.15 Clinicians can initially find the optimal working hand position and neutral posture as previously described without wearing loupes. Next, take a neutral posture photograph demonstrating this posture. From this photo, a reference line from where the frame temple arm would sit is established, to measure the degree of head tilt. Next, with loupes on, the head is tilted until the field of view is centered on the optimal hand position and another photograph is taken to demonstrate working posture with the current loupes. Comparing this working posture photo and the neutral posture image taken earlier, measure the declination angle of the current loupes and the angle of the body posture. Finally, compute the head tilt angle using the reference line angle measured with the neutral posture photo.15
CO-AXIAL ALIGNMENT
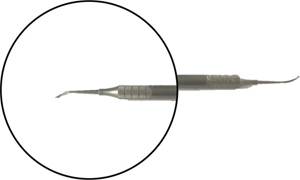
Misalignment is important when considering ergonomic fit for loupes. Co-axial alignment or more specifically co-axial misalignment is related to the magnification lens portion of the loupes.12 If the lenses are in co-axial misalignment, the magnified image viewed through the loupes will not be aligned with the unmagnified image (Figure 2). If the lenses are misaligned, when instruments enter the field of vision while working on a patient, they will appear higher or lower than their actual placement. This could result in awkward movements and postures at the neck and cervical region to locate the actual placement of the instrument. Co-axial misalignment may also cause visual aberrations that affect color and shape perception. This could also lead to visual strain as well as neck and cervical strain if improperly aligned. More research is needed to explore whether proper alignment decreases the risk for MSDs.12
CONCLUSION
While loupes may reduce neck strain and help to provide balanced musculoskeletal ergonomics, oral health professionals must be diligent about ensuring their loupes are properly fitted and adjusted, as ill-fitting loupes may actually increase the incidence of MSDs. Proper working distance, depth of field, co-axial alignment, and declination angle must be determined to ensure the neck is not being flexed beyond the optimal 20°. Many clinicians use improperly fitted loupes that may not cause pain instantly, but over time, may contribute to MSD development. More quantitative research is needed to determine both the short- and long-term ergonomic impact of different types of loupes, as well as the effects of proper and incorrect fit.
REFERENCES
- Hayes M, Osmotherly P, Taylor J, et al. The effect of loupes on neck pain and disability among dental hygienists. Work. 2016;53:755–762.
- Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009;7:159–165.
- Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002;42:248–257.
- Congdon LM, Tolle SL, Darby M. Magnification loupes in US entry–level dental hygiene programs occupational health and safety. J Dent Hyg. 2012;86:215–222.
- Sunell S, Rucker L. Surgical magnification in dental hygiene practice. Int J Dent Hyg. 2004;2:26–35.
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders in a 3 year longitudinal cohort of dental hygiene students. J Dent Hyg. 2014;88:36-41.
- Syme SE, Fried JL, Strassler HE. Enhanced visualization using magnification systems. J Dent Hyg. 1996;71:202–206.
- Michaelides P, Stambaugh R. Zooming in on magnification. Dimensions of Dental Hygiene. 2007;5(4):16–21.
- Branson B, Simmer-Beck M. Visual acuity without injury. Dimensions of Dental Hygiene. 2009;7(9):46–49.
- Rucker LM, Beattie C, McGregor C, Sunell S, Ito Y. Declination angle and its role in selecting surgical telescopes. J Am Dent Assoc. 1999;130:1096–100.
- Valachi B. Neck health: the three ergonomic criteria for loupes selection. Available at: dentaleconomics.com/articles/print/volume-98/issue-9/columns/preventing-pain-in-dentistry/neck-health-the-three-ergonomic-criteria-for-loupes-selection.html. Accessed March 24, 2017.
- Wen, WM. An investigation in the prevalence of co-axial misalignment of surgical loupes amongst BC dental professionals. Available at: open.library.ubc.ca/cIRcle/collections/ubctheses/24/items/1.0228864. Accessed March 24, 2017.
- Barresi BJ. Ocular Assessment: The Manual of Diagnosis for Office Practice. Boston: Butterworths; 1984:123–129.
- Moses RA. Adler’s Physiology of the Eye. 7th ed. St. Louis: Mosby; 1981:225–226, 319-323.
- Chang BJ. Declination angle: the key factor for custom loupes. Available at oralhealthgroup.com/features/declination-angle-the-key-factor-for-custom-loupes-b-j-chang-phd/. Accessed March 24, 2017.
- Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. J Cal Dental Assoc. 2002;30:139–148.
- Chang BJ. Ergonomic benefits of surgical telescopes: selection guidelines. J Cal Dental Assoc. 2002;30:161–169.
- Rucker L, McGregor C, Woo G, Leong YM. Effects of low-magnification surgical telescopes on preclinical operative dental performance. J Dent Educ. 1992;1:34.
From Dimensions of Dental Hygiene. April 2017;15(4):24,26.

