 SDI PRODUCTIONS/E+/GETTY IMAGES PLUS
SDI PRODUCTIONS/E+/GETTY IMAGES PLUS
Decreasing the Impact of Bias
Explicit (conscious) and implicit (unconscious) biases affect providers’ understanding, actions, communication, and treatment decisions.
This course was published in the October 2019 issue and expires October 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define explicit and implicit bias.
- Discuss the impact of implicit bias on dental hygiene patient care.
- Identify means to self-assess implicit bias.
- Recognize ways to manage implicit bias.
While dental professionals should practice with the intent of providing competent care to all patients, individual attitudes and behaviors influence the delivery of care and may contribute to health disparities. The National Healthcare Quality and Disparities Agency found that African-Americans, Asians, Pacific Islanders, and Hispanics continue to receive lower quality health care than Whites.1 The report suggests that both explicit and implicit bias may impact the quality and equity of care patients receive.1 While cultural and ethnic minorities are particularly susceptible to implicit bias, health care providers need to be aware of their personal biases that may further disadvantage vulnerable populations such as women, older adults, sexual minorities, those economically disadvantaged, and the overweight.2 Hence, awareness and understanding of both explicit and implicit bias are important in fostering a professional oral health practice environment that embraces inclusion and diversity and assures all patients are treated with dignity and respect.
Bias refers to a preference or aversion to a person or group of people compared to another and can be categorized as explicit or implicit.3 Explicit bias refers to attitudes and beliefs on a conscious level, whereas implicit bias refers to attitudes, thoughts, and feelings that affect actions and decisions about a person or group in an unconscious way.4,5 Implicit bias attitudes are difficult to consciously acknowledge and control, as they are activated involuntarily and deeply seated (Table 1).3–5 Due to the subconscious nature of these attitudes and stereotypes, they are different from known biases that individuals may choose to conceal. Both types however, affect providers’ actions, care planning, and treatment decisions.6 Implicit bias may occur unintentionally and can be triggered unknowingly by such things as a patient’s skin color, accent, weight, sexuality, or socioeconomic status.4,7,8 Studies suggest implicit bias attitudes are automatically activated, difficult to control, and may have detrimental effects on patient care in all health care settings.9,10
IMPACT OF IMPLICIT BIAS
While the causes of health care disparities are multifactorial, implicit and explicit biases have been suggested as some of many factors contributing to disparities in access to health care, the quality of care received, and health outcomes.1,5 Explicit bias attitudes are known to the individual, measurable by self-report, and often predict verbal behavior.11 In contrast, implicit biases are involuntary attitudes about race or social groups and a provider may not recognize their effect and influence on treatment decisions and behaviors.5–8 Research shows that many providers hold some level of implicit bias toward various patient groups, with most studies examining interactions between Black patients and Non-black providers.9,10,12–20 Certain combinations of physicians and patients lead to poorer interactions, specifically those in which physicians are high in implicit bias and patients are high in mistrust of the medical system and reported past discrimination.6–20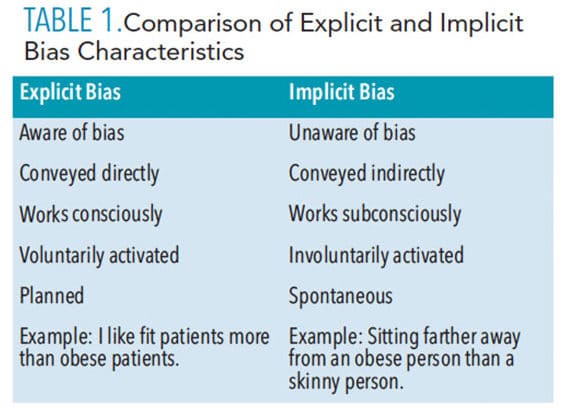
Unconscious preferences may be expressed in several ways by health care professionals: using a dominant and/or condescending tone, allocating time differently, failing to provide language interpreters, doing more or less diagnostic work, failure to treat pain aggressively, and recommending differing treatment options based on assumptions about adherence abilities.9,12 Though a health care provider may have egalitarian values and outwardly believe all patients should be treated equally, implicit bias may result in a dissociation between that value and his or her actual thoughts and actions.2 Patient perspectives on biases were examined by Gonzales et al13 with patients self-reporting varying levels of health care treatment, courtesy, respect, and how efficiently and effectively they were seen by a physician based on race, ethnicity, and language spoken. Results found that patients of ethnic minorities felt Whites were treated in a more positive way.13 Therefore, providers need to be aware of their own bias and these perceptions as they may affect their ability to provide impartial health and dental hygiene care to differing cultural and ethnic groups.
Previous literature suggests a variance in the quality of care and communication according to race and ethnicity related to implicit and explicit bias, with African-Americans and Hispanics receiving lower quality health care than Whites.14–23 Studies have found bias affecting treatment decisions based on a patient’s race. A study of 287 physicians surveyed about implicit bias found differences in treatment interventions based on race.15 The physicians participated in a simulated clinical vignette in which they were shown a picture of a White or African-American patient, asked questions regarding the likelihood of chest pain being related to a coronary issue, and whether they would prescribe thrombolysis. Results showed physicians self-reported they had no preference for White or African-American patients; however, their implicit measures revealed a preference for White patients. More importantly, as implicit bias scores increased, the likelihood of prescribing thrombolysis for African-American patients decreased.15
In another study, 210 family medicine and internal medicine primary care providers (PCPs) were surveyed.14 Two tests were administered: one related to implicit bias against Hispanics and one related to implicit bias against African-Americans. Results demonstrated the PCPs showed greater positivity toward Whites and strong bias against Hispanics and African-Americans compared with Whites. Explicit biases were found to be seemingly nonexistent among PCPs, which may be due to explicit bias being more overt.14 Research has also determined implicit bias negatively affects communication and interaction with minority groups compared with Whites.16,20,21 This can impact patient trust, perception, and communication with the potential to impact patient adherence to medical visits and treatment plans, thereby increasing health disparities. Cultural awareness training related to detecting implicit bias among health care providers has the potential to increase quality of care for ethnic minority groups in both medical and dental settings.
Research related to race and implicit and explicit bias has been extensive.9,10,13–20 While less researched, health care providers need to be aware of biases related to other susceptible populations such as obese patients, sexual minorities, older adults, and women. Implicit and explicit attitudes have been cited as affecting quality care and patient-centered communication in the obese population. For example, previous studies have found provider bias related to obese patients being less likely to adhere to treatment or self-care recommendations,22,23 spending less time educating obese patients compared with those of normal weight,24 and overattributing symptoms to obesity or failing to consider other treatment options beyond advising a patient to lose weight.22
Research has also indicated bias against the lesbian, gay, bisexual, transgender, and queer (LGBTQ) population.8 One recent study of providers found heterosexual providers had negative implicit biases toward LGBTQ people, whereas LGBTQ providers had both implicit and explicit preferences for LGBTQ people over heterosexual people.8
Related to age, bias has been reported with poor communication.25,26 For example, health care professionals may not explain as much to older adults as they would younger patients,25 and may use baby talk with elderly patients, especially women, using phrases like “sweetie” and “young lady.”26 Implicit biases against these vulnerable populations may devalue the patient, impact trust and communication, and lead to avoidance of care based on being stigmatized and treated differently.2,12
More research is needed to expand and update knowledge related to bias of these populations in an effort to provide competence and decrease disparities for more than just ethnic minorities. More important, biases toward these groups need to be examined further in dental hygiene care with increasingly diverse patient populations in terms of age, sexuality, and weight. With evidence suggesting links between oral health and systemic conditions associated with aging and obesity, dental hygienists must be conscious of the implications these biases may have on patient care.
IN THE DENTAL SETTING
While bias has been extensively researched in medical settings, there is a significant gap in the dental literature. One aspect of bias that has been researched in dentistry is color-blind racial attitudes, a contemporary type of implicit bias. Color blindness refers to a set of beliefs that racial differences or race are no longer relevant problems in modern society.27
People with color-blind tendencies believe that race does not play an important role in someone’s experiences and may harbor these ideals in an attempt to reduce racial prejudice.28 This can be outwardly perceived as denying or minimizing the impact that racism and stereotypes have on minorities and, in turn, perpetuates racial prejudice and inequality.28,29 It is measured using a validated test, with higher scores indicating greater endorsement of color-blind racial attitudes.28 A study found school counselors with lower multicultural competence training possessed high levels of color blindness in comparison with those who had received training.30 Additionally, studies reveal psychologists with higher levels of color blindness demonstrate lower levels of empathy for minorities,31 and counseling students with high levels of colorblindness display an inability to relate to their clients’ disparities.32 These studies indicate a need for multicultural awareness and competence training in order to reduce color blindness, relate to patients and their disparities, and, ultimately, reduce bias.
Two important studies exist related to color blindness in dentistry.33,34 To explore color-blind racial attitudes among dental students and faculty, Su et al34 assessed 235 dental students and 71 dental faculty and found that dental faculty and students possessed moderate levels of color-blind racial attitudes. A separate study of students in the dental field investigated curriculum interventions affecting students’ outcomes associated with ethical sensitivity, stereotypes, cultural competence, and color blindness; this study also found moderate levels of color-blind racial attitudes.33 Results of these studies suggest a need for more opportunities to assess implicit bias among dental providers and whether they are cognizant of how it might affect patient care. It is likely dental hygiene practitioners, educators, and students need opportunities to address color blindness and other types of implicit bias in order to combat oral health care disparities.
MANAGING IMPLICIT BIAS
The goal in managing implicit bias should be to increase equality in health care delivery and improve multicultural awareness and competence. Research suggests workshops, training, and continuing education for practitioners are essential to foster multicultural competence.35 Ideally, early and habitual intervention training while practitioners are still in school could potentially minimize bias that may affect their future careers.36 All health care providers—including dental hygiene practitioners—are susceptible to implicit bias that may impact competency and health care delivery.36,37 Understanding cultural differences can increase self-awareness of unconscious bias and may be an impetus for it to be overcome.
As implicit bias may not be easily recognized, practitioners should first be educated on the topics of stereotyping, prejudice, and discrimination. This can be accomplished by providing real-world examples and the differences between explicit and implicit bias.36 Once there is an understanding of the concept and relation between the two, practitioners should consider using self-assessment tools such as the Implicit Association Test (IAT) or Color-Blind Racial Attitudes Scale (CoBRAS) to recognize self-implicit biases. The IAT measures implicit bias by detecting attitudes that are automatically activated without the person’s awareness of the cause.38 Clinicians can take an online-adapted IAT at: https://projectimplicit.net for many subcategories of implicit bias such as sexuality, disability, and much more.39 The CoBRAS is a valid and reliable survey instrument for measuring a type of implicit bias: contemporary/modern day racial attitudes, and stereotyping. The CoBRAS is a 20-item instrument with three subcategories (racial privilege, institutional discrimination, blatant racial issues), scored on a six-point scale with higher scores signifying greater global and sociopolitical belief in a just world, racial and gender intolerance, and racial prejudice.28 Additionally, any training should also provide evidence of research to reinforce the point that all people exhibit differing levels of implicit bias that affect their judgement.36,37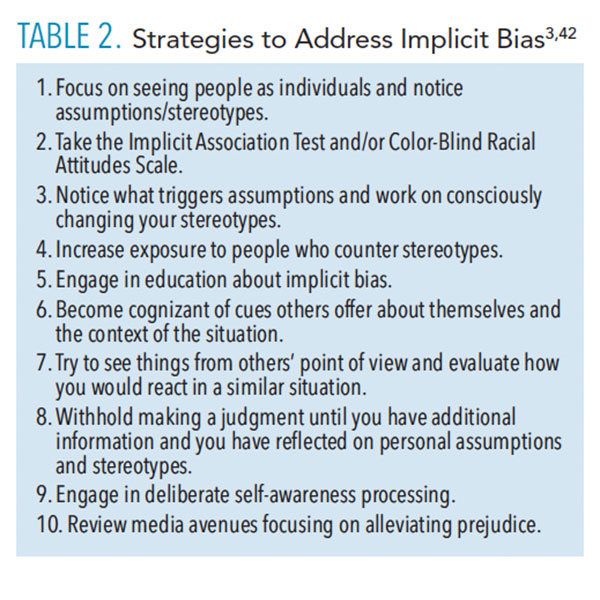 Sukhara et al37 theorized a six-point framework for integrating bias training into health care education. First, a program should create a safe and nonthreatening learning context. Second, focus on increasing knowledge by presenting evidence-based material regarding the psychological components that drive bias. Third, the program should emphasize how implicit bias influences behaviors and patient outcomes by citing existing research.37,40,41 Discussing the impact could help to teach learners how to address and mitigate their bias.37,42 In the fourth step, the goal should be to increase self-awareness of existing bias using assessment tests to provide self-reflection, discussion, and awareness. Fifth, a focus on improving conscious efforts to overcome implicit bias to encourage self-monitoring. Setting goals for self-re-evaluation or establishing benchmarks might encourage self-monitoring.37 Table 2 provides strategies for helping professionals act in a more mindful way regarding implicit biases. Sixth, researchers recommend enhancing awareness of how implicit bias influences others.3,42
Sukhara et al37 theorized a six-point framework for integrating bias training into health care education. First, a program should create a safe and nonthreatening learning context. Second, focus on increasing knowledge by presenting evidence-based material regarding the psychological components that drive bias. Third, the program should emphasize how implicit bias influences behaviors and patient outcomes by citing existing research.37,40,41 Discussing the impact could help to teach learners how to address and mitigate their bias.37,42 In the fourth step, the goal should be to increase self-awareness of existing bias using assessment tests to provide self-reflection, discussion, and awareness. Fifth, a focus on improving conscious efforts to overcome implicit bias to encourage self-monitoring. Setting goals for self-re-evaluation or establishing benchmarks might encourage self-monitoring.37 Table 2 provides strategies for helping professionals act in a more mindful way regarding implicit biases. Sixth, researchers recommend enhancing awareness of how implicit bias influences others.3,42
Shifting focus to empathy and modeling the patient-provider interaction as a collaboration can help a learner perceive a patient of a differing ethnic group or minority as equal. Role-playing, reading case studies, listening to stories of marginalization, and interacting with minority groups help enhance awareness.37,43 Using this framework, educators and practitioners alike could build curricula, strategies, goals, and evaluation methods to provide inherent bias and multicultural awareness and competence education and training. A program that follows this framework would also have far-reaching interprofessional implications, for health care professionals in an effort to increase equitable health care delivery.
CONCLUSIONS
Disparities in health care continue to be a concern, with the potential for bias to play a role in this problem. Explicit and implicit biases affect providers’ understanding, actions, communication, and treatment decisions. In order for dental hygienists to provide impartial care to all patients, clinicians must first identify that implicit bias exists and impacts decisions and treatment for patients. In order to manage bias and how it affects patient care, practitioners should determine their own implicit bias through self-assessment. This may help clinicians begin to identify and manage biases that may influence care. Finally, curricula and continuing education courses on implicit bias identification and management should be created in order to train dental hygienists about bias and how to prevent and reduce its outcomes in health care practice.
REFERENCES
- Agency for Healthcare and Research Quality. National Healthcare Quality and Disparities Report. Available at: ahrq.gov/research/findings/nhqrdr/nhqdr17/index.html. Available at September 18, 2019.
- Fitzgerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18:19.
- Sportsman S. Implicit Bias: Does It Impact Nursing Education? Available at: https://collaborativemomentum.com/2019/06/19/implicit-bias-does-it-impact-nursing-education/. Accessed September 18, 2019.
- Blair IV, Banaji MR: Automatic and controlled processes in stereotype priming. J Pers Soc Psychol. 1996;70:1142–1163.
- Devine PG. Stereotypes and prejudice: their automatic and controlled components. J Pers Soc Psychol. 1989;56:5–18.
- Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–229.
- Devine PG, Forscher PS, Austin AJ, Cox WT. Long-term reduction in implicit race bias: a prejudice habit-breaking intervention. J Exp Soc Psychol. 2012;48:1267–1278.
- Sabin JA, Riskind RG, Nosek BA. Health care providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Pub Health. 2015;105:1831–1841.
- Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Pub Health. 2015;105:e60–e76.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: a narrative review. Group Process Intergroup Relat. 2016;19:528–542.
- Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20:896–913.
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–326.
- Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, McKee MD. Patient perspectives on racial and ethnic implicit bias in clinical encounters: Implications for curriculum development. Patient Educ Couns. 2018;101:1669–1675.
- Blair IV, Havranek EP, Price DW, et al. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Pub Health. 2013;103:92.
- Green A, Carney D, Pallin D, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22:1231–1238.
- Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Pub Health. 2012;102:979.
- Haider AH, Schneider EB, Sriram N, et al. Unconscious race and class biases among registered nurses: vignette-based study using implicit association testing. J Am Coll Surg. 2015;220:1077–1086.
- Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306:942–951.
- Blair IV, Steiner JF, Fairclough DL, et al. Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Ann Fam Med. 2013;11:43–52.
- Schaa KL, Roter DL, Biesecker BB, Cooper LA, Erby LH. Genetic counselors’ implicit racial attitudes and their relationship to communication. Health Psychol. 2015;34:111–119.
- Hagiwara N, Penner LA, Gonzalez R, et al. Racial attitudes, physician–patient talk time ratio, and adherence in racially discordant medical interactions. Soc Sci Med. 2013;87:123–131.
- Persky S, Eccleston CP. Medical student bias and care recommendations for an obese versus non-obese virtual patient. Int J Obes. 2011;35:728.
- Huizinga MM, Bleich SN, Beach MC, Clark JM, Cooper LA. Disparity in physician perception of patients’ adherence to medications by obesity status. Obes Res. 2010;18:1932–1937.
- Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13:1615–1623.
- Higashi RT, Tillack AA, Steinman M, Harper M, Johnston CB. Elder care as “frustrating” and “boring:” understanding the persistence of negative attitudes toward older patients among physicians-in-training. J Aging Stud. 2012;26:476–483.
- Cruikshank M. Aging and identity politics. J Aging Stud. 2008;22:147–151.
- Neville HA, Poteat VP, Lewis JA, Spanierman LB. Changes in white college students’ color-blind racial ideology over 4 years: do diversity experiences make a difference? J Couns Psycholy. 2014;61:179–190.
- Neville HA, Lilly RL, Duran G, Lee RM, Browne L. Construction and initial validation of the color-blind racial attitudes scale (CoBRAS). J Couns Psychol. 2000;47:59–70.
- Tawa J, Ma R, Katsumoto S. “All lives matter:” the cost of colorblind racial attitudes in diverse social networks. Race Soc Probl. 2016;8:196–208.
- Chao RCL. Race/ethnicity and multicultural competence among school counselors: multicultural training, racial/ethnic identity, and color‐blind racial attitudes. J Couns Dev. 2013;91:140–151.
- Burkard AW, Knox S. Effect of therapist color-blindness on empathy and attributions in cross-cultural counseling. J Couns Psychol. 2004;51:387–397.
- Gushue GV, Constantine MG. Color-blind racial attitudes and white racial identity attitudes in psychology trainees. Prof Psychol Res Pr. 2007;38:321–328.
- Behar-Horenstein LS, Garvan CW. Relationships among the knowledge, efficacy, and practices instrument, color-blind racial attitudes scale, Deamonte Driver survey, and defining issues test 2. J Dent Educ. 2016;80:355–364.
- Su Y, Behar-Horenstein LS. Color-blind racial beliefs among dental students and faculty. J Dent Educ. 2017;81:1098.
- Gawronski B, Bodenhausen GV. Associative and propositional processes in evaluation: an integrative review of implicit and explicit attitude change. Psychol Bull. 2006;132:692–731.
- Stone J, Moskowitz GB. Non-conscious bias in medical decision making: what can be done to reduce it? Med Educ. 2011;45:768–776.
- Sukhera J, Watling C. A framework for integrating implicit bias recognition into health professions education. Acad Med. 2018;93:35–40.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74:1464–1480.
- Project Implicit. Implicit Social Cognition. Available at: https://projectimplicit.net. Accessed September 18, 2019.
- Burgess DJ, Fu SS, Van Ryn M. Why do providers contribute to disparities and what can be done about it? J Gen Intern Med. 2004;19:1154–1159.
- Czopp AM, Monteith MJ, Mark AY. Standing up for a change: reducing bias through interpersonal confrontation. J Pers Soc Psychol. 2006;90:784–803.
- Ackerman-Barger K. Understanding Unconscious Bias Can Promote Healthy Equity. Available at: https://campaignforaction.org/understanding-unconscious-bias-can-promote-health-equity/. Accessed September 18, 2019.
- Gatewood E, Broholm C, Herman J, Yingling C. Making the invisible visible: Implementing an implicit bias activity in nursing education. J Prof Nurs. In press.
From Dimensions of Dental Hygiene. October 2019;17(9):40—42,45.



