 CHOKJA/ISTOCK/GETTY IMAGES PLUS
CHOKJA/ISTOCK/GETTY IMAGES PLUS
An Inside Look at Musculoskeletal Disorders Among Dental Hygienists
Myriad factors impact oral health professionals’ risk of developing these painful and possibly career-ending injuries.
Workplace musculoskeletal disorders (MSDs) are the most common cause of limited or lost work time.1 According to the United States Bureau of Labor and Statistics, approximately 30% of work-related injuries are attributed to MSDs.2 As dental hygienists are at high risk of MSDs—impacting both career longevity and satisfaction—developing a foundation in evidence-based ergonomic principles is imperative.3
Ergonomics is the study of people at work with the goal of preventing MSDs and soft tissue damage produced by acute or chronic exposure to problematic posture, force, repetitive motion, and vibration.1 In the practice of dental hygiene, clinicians and students are likely exposed to all of the aforementioned risk factors. As awkward and static postures, pinch force, repetitive motion, and vibration contribute to the development of MSDs, oral health professionals should adhere to specific ergonomic recommendations.3–12
PREVALENCE AMONG ORAL HEALTH PROFESSIONALS
The high prevalence of MSDs among oral health professionals—including dental hygienists, dentists, dental assistants, dental laboratory technicians, and dental/dental hygiene students—is well documented in the literature.3,6,8,9,13–15 Lietz et al3 conducted a meta-analysis of MSD prevalence among oral health professionals and found a wide variance, ranging from 11% to 98%, with a pooled prevalence of 58% among all dental practitioners. Another literature review evaluated the relationship between MSDs and dental hygienists. The study authors determined 92% of oral health professionals experienced MSDs, with dental hygienists being the most affected.13
Research also suggests dental hygienists experience two times to three times more MSDs than dental assistants, and significantly higher rates of MSDs than dentists.3,13 In a self-reported survey of Australian dental hygienists, participants noted experiencing occupational MSDs in both the upper and lower extremities, causing pain that lasted more than 2 days and impacting their daily lives.14
Specific areas of the body are also more likely to experience MSDs among oral health professionals. Results of a self-reported survey found that pain was most frequently reported in the neck, back, and shoulder regions followed by the thumbs, wrists, arms, and hips.9 A small study of 12 dental hygienists showed they were at increased risk for trapezius muscle disorders, such as tension neck syndrome, trapezius myalgia, cervical syndrome, shoulder acromioclavicular syndrome, shoulder tendinitis, and biceps tendinitis.4 Medial epicondylitis, peritendonitis, ulnar nerve entrapment at the elbow, radial tunnel syndrome, carpal tunnel syndrome, overused hand syndrome, and Heberden’s arthrosis are also common among dental hygienists.4 Hayes et al5 also found that dental hygienists most often seek medical treatment for MSD pain in the wrist and hip regions.
OCCUPATIONAL RISK FACTORS
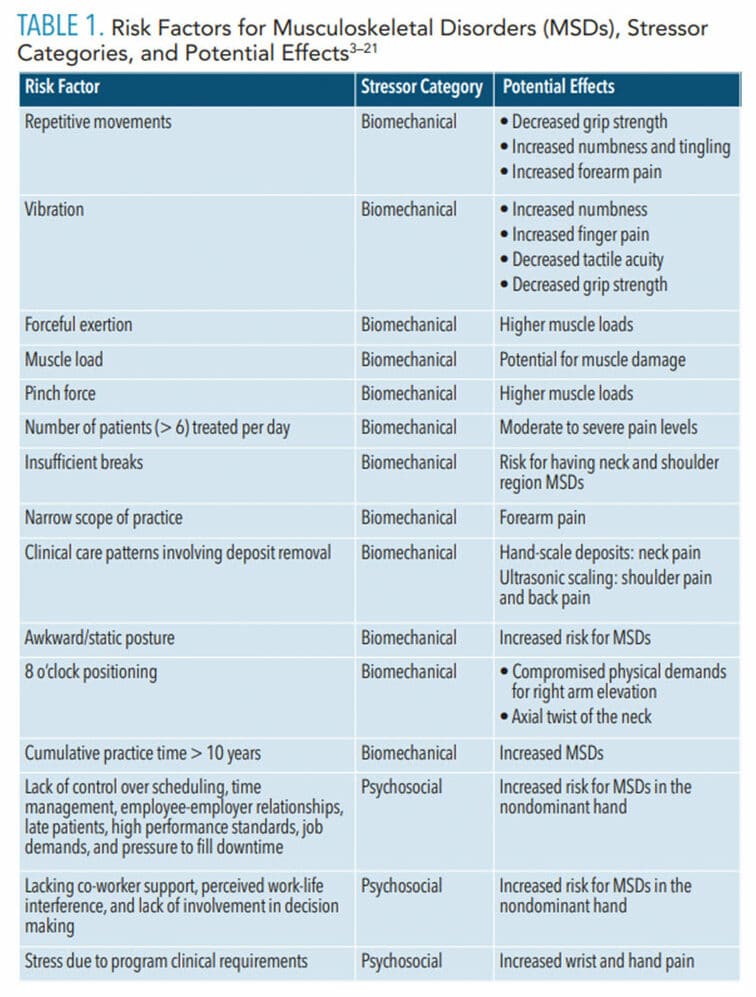
Occupational risk factors for oral health professionals are associated with both biomechanical and psychosocial stressors (Table 1).3–21 Examples of biomechanical stressors in dental hygiene include repetitive movements, vibration, forceful exertion, increased muscle load, number of patients treated per day, insufficient breaks, categories of practice, clinical care patterns involving deposit removal, and poor patient/operator positioning including posture and clock positioning.3,4,7,9,11,13,14,16,17,19 Among oral health professionals, these stressors most often appear in the neck, shoulder, upper back, lower back, spine, forearms, and wrists.5,7 Psychosocial stressors affecting MSD risk in oral health professionals include work demands, control of scheduling and equipment procurement, wage satisfaction, and colleague support.8
Biomechanical risk factors may relate to clinical care patterns among dental hygienists.9,13,13 Humann and Rowe9 found that dental hygienists who treated more than eight patients per day in addition to high numbers of patients with moderate to heavy calculus experienced significantly more moderate to severe pain levels when compared with clinicians who treated less than eight patients per day and patients with light to moderate calculus. In addition, dental hygienists with little to no pain reported using proper posture more than 50% of patient treatment time. Those with moderate or severe pain indicated using proper posture less than 50% of treatment time.9
Dental hygienists’ narrow scope of practice, with clinicians performing scaling and root debridement for more than 50% of treatment time, increases MSD risk.13 Hayes et al10 found that dental hygienists working in periodontal practices reported higher rates of forearm-associated MSDs and little task variety. In contrast, dental hygienists working in orthodontic practices had the fewest number of MSDs, which may correlate with less time spent scaling deposits and more task variety.10,13 Cumulative practice time is also associated with MSD development. Johnson and Kanji13 determined that dental hygienists who practiced more than 10 years reported more MSD pain than other practitioners.
The increased muscle load experienced by dental hygienists who go without a break between patients raises the risk of neck and shoulder MSDs.3 Research also shows some procedures are associated with pain in specific regions, such as coronal polishing and shoulder pain, manual scaling and neck pain, and ultrasonic use and shoulder pain.3
While both hand and power instrumentation can cause MSDs, manual scaling impacts right forearm muscles more than powered instrumentation. This may be due to the forceful grip and repetitive motion required by hand instrumentation.4 Both hand scaling and ultrasonic instrumentation increase numbness and decrease grip strength; however, finger pain and decreased tactile acuity are more common with the use of vibrating instruments.8 The types of instruments used also impact muscle load. For instance, the use of a corded handpiece during polishing procedures stresses the forearm muscles,16 and the use of instruments with small handle diameters (< 10 mm) and heavier weights (> 23 g) require higher amounts of muscle load and pinch force, increasing the chance of MSD development.17–19
When considering clinician positioning, research suggests the 8 o’clock position is the most ergonomically compromised due to deviations from neutral right arm elevation, axial twist of the neck, pelvis position, and spinal posture.7,11 The 11 o’clock to 1 o’clock zone is optimal to maintain neutral positioning and 12 o’clock presents ideal neutral pelvic posture.7 Horton et al20 found that dental hygienists who experienced neck flexion surpassing 35° in all working positions, trunk flexion exceeding 20°, and elbow flexion surpassing 90° had a higher risk of MSD development. In addition, the risk for developing MSDs increases with the use of awkward postures during clinical practice and remaining in static postures for greater than 40 minutes at one time.3
Psychosocial stressors such as lack of control over scheduling, time management, employee-employer relationships, late patients, high-performance standards, job demands, and pressure to fill downtime may increase MSD risk.13 Other psychosocial stressors include lack of co-worker support, perceived work-life interference, and little involvement in decision making.10 Warren8 found that MSDs in the nondominant hand may be related to workplace demands, lack of coworker support, and low autonomy. The study also noted that elevated hand and wrist pain may come from the combined biomechanical stressor of static reach/grip and the psychosocial factor of control.
INTERVENTIONS
Potential interventions for decreasing occupational MSD risk factors include loupes, equipment selections, and reducing psychosocial stressors with frequent breaks and exercise (Table 2).3,4,9,12,16–19,21–23 Dental hygienists who wear loupes report reductions in upper extremity pain and disability when compared with those who practice without loupes.10,21 Clinicians who don’t wear loupes experience more shoulder, wrist, and hand pain when compared with those who wear loupes.10,21
Research has also explored the impact of clinical care patterns on practitioners. One study found that dental hygienists who experienced moderate to severe pain may not maximize ultrasonic use when treating patients with moderate to heavy deposits.9 This may be due to the need for stronger force during hand instrumentation of moderate to heavy deposits.9 The increased use of ultrasonics on patients with heavier calculus deposits may help dental hygienists reduce their MSD risk. Ultrasonic use also reduces pressure on the forearm muscles and decreases wrist velocity.4,9
Reducing pinch force may be achieved by selecting instruments with large handle diameters and tapered cross-sectional shapes.17–19 Using instruments with padded handles weighing less than 23 g may decrease muscle activity and applied forces.17–19 The texture of instrument handles may also influence practitioner grasp and affect muscle loads.19
Frequent breaks and exercise may also decrease MSDs among dental hygienists. Research shows that hand instrumentation hinders clinicians’ ability to rest their forearm extensor muscles.4 In addition to the need for frequent breaks during work time, exercise may be an intervention for MSD development. Research indicates practicing dental hygienists and students may benefit from incorporating yoga into their daily routine, as 65% of dental hygiene students who participated in two 1-hour yoga sessions per week experienced less MSD pain and 52% experienced fewer headaches.22
![Interventions for MSDs]() CONCLUSION
CONCLUSION
Musculoskeletal disorders are a health burden for oral health professionals that can lead to shortened career longevity, need for medical attention, and lack of job satisfaction. Oral health professionals should take continuing education courses on biomechanical and psychosocial risk factors, as well as interventions to reduce the risk for MSDs in order to increase career longevity and satisfaction.
REFERENCES
- Occupational Safety and Health Administration. Ergonomics. Available at: osha.g/v/SLTC/ergonomics Accessed December 9, 2020.
- National Institute for Occupational Safety and Health. Ergonomics and Musculoskeletal Disorders. Available at: cdc.gov/niosh/topics/ergonomics/default.html. Accessed December 9, 2020.
- Lietz J, Kozak A, Nienhaus A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in western countries: a systematic literature review and meta-analysis. PLoS One. 2018;13:e0208628.
- Åkesson I, Balogh I, Hansson G. Physical workload in neck, shoulders and wrists/hands in dental hygienists during a work-day. Appl Ergon. 2012;43:803–811.
- Ng, A, Hayes M, Polster A. Musculoskeletal disorders and working posture among dental and oral health students. Healthcare (Basel). 2016;4:13.
- Hayes M, Smith D, Taylor J. Musculoskeletal disorders in a 3-year longitudinal cohort of dental hygiene students J Dent Hyg. 2014;88:36-41.
- Howarth SJ, Grondin DE, La Delfa NJ, et al. Working position influences the biomechanical demands on the lower back during dental hygiene. Ergonomics. 2016;59:545–555.
- Warren N. Causes of musculoskeletal disorders in dental hygienists and dental hygiene students: a study of combined biomechanical and psychosocial risk factors. Work. 2010;35:441–454.
- Humann P, Rowe D. Relationship of musculoskeletal disorder pain to patterns of clinical care in California dental hygienists. J Dent Hyg. 2015;89:305–312.
- Hayes M, Taylor J, Smith D. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2011;10:265–269.
- La Delfa N, Grondin D, Cox J, Povtin J, Howarth S. The biomechanical demands of manual scaling on the shoulders and neck of dental hygienists. Ergonomics. 2016;59:127–137.
- Congdon L, Tolle S, Darby M. Magnification loupes in US entry-level dental hygiene programs–occupational health and safety. J Dent Hyg 2012;86:215–222.
- Johnson C, Kanji Z. The impact of occupation-related musculoskeletal disorders on dental hygienists. Canadian Journal of Dental Hygiene. 2016;50(2):72–79.
- Hayes M, Smith D, Taylor, J. Musculoskeletal disorders and severity among Australian dental hygienists. BMC Research Notes. 2013;6:250.
- Morse T, Michalak-Turcotte C, Atwood-Sanders M, et al. A pilot study of hand and arm musculoskeletal disorders in dental hygiene students. J Dent Hyg. 2003;77:173–179.
- McCombs G, Russell D. Comparison of corded and cordless handpieces on forearm muscle activity, procedure time and ease of use during simulated tooth polishing. J Dent Hyg. 2014;88:386–393.
- Dong H, Loomer P, Barr A, Laroche C, Young E, Rempel D. The effect of tool handle shape on hand muscle load and pinch force in a simulated dental scaling task. Appl Ergon. 2007;38:525–531.
- Simmer-Beck M, Branson BG. An evidence-based review of ergonomic features of dental hygiene instruments. Work. 2010;35:477–448.
- Suedbeck J, Tolle SL, McCombs G, Walker ML, Russell DM. Effects of instrument handle design on dental hygienists’ forearm muscle activity during scaling. J Dent Hyg. 2017;91:47–54.
- Horton S, Johnstone C, Hutchinson C, Taylor P, Wade K. Clinical working postures of bachelor of oral health students. N Z Dent J. 2011;107:74–78.
- Hayes M, Osmotherly P, Taylor J, Smith D, Ho A. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int J Dent Hyg 2014;12:174–179
- Monson A, Chismark A, Cooper B, Krenik-Matejcek T. Effects of yoga on musculoskeletal pain. J Dent Hyg. 2017;91:15–22.
- Partido B. Dental hygiene students’ self-assessment of ergonomics utilizing photography. J Dent Educ. 2017;81:1194–1202.
From Dimensions of Dental Hygiene. January 2021;19(1):22-25.

 CONCLUSION
CONCLUSION