 CATALIN205/ISTOCK/GETTY IMAGES PLUS
CATALIN205/ISTOCK/GETTY IMAGES PLUS
Advances in Visual Acuity
Clinicians have a variety of options available to improve their viewing of the oral cavity.
Technological advances have improved visual acuity for clinicians, while also providing patient care benefits. Research shows that magnification coupled with illumination improves visibility, diagnostic ability, operator ergonomics, and treatment outcomes.1-6 Indeed, magnification reduces eye strain and improves visual evaluation of periodontal probe readings, soft tissue assessment, supra- and subgingival calculus evaluation and removal, assessment of radiographs, and caries detection.1,4,7–10 Notably, these technologies particularly benefit dental hygienists and their ability to provide high-quality patient care.
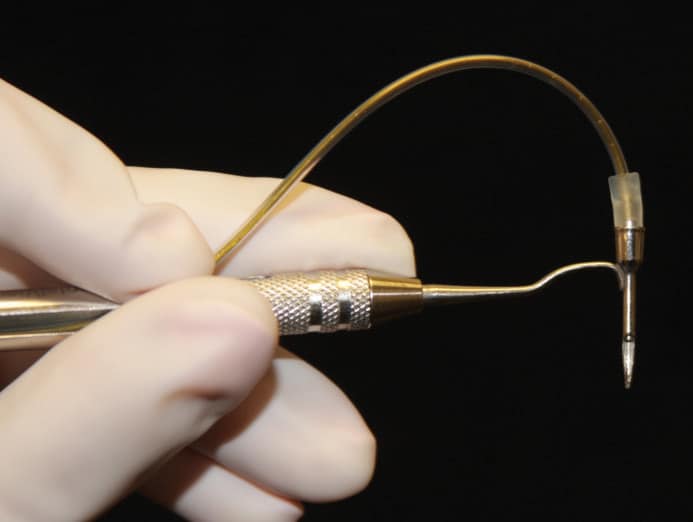
ENDOSCOPE AND VIDEOSCOPE
Endoscope technology aids periodontal diagnosis and therapy by providing indirect visualization and magnification of the soft tissues of the sulcus, as well as the tooth surface.1,4,10 The dental endoscope enables clinicians to see root calculus deposits, caries, root fractures, open restorative margins, and excess cement on implants. The dental endoscope has a subgingival probe adapted to fiber optic imaging, a sheath that provides a sterile barrier, a pump to provide irrigation to the working field, illumination, a video camera to capture images, and a flat panel video display monitor for live viewing of the working field with a magnification of 12 times to 48 times (Figure 1).1,4,10
As residual calculus and associated plaque biofilm contribute to the inflammatory response and periodontitis, the fact that the dental endoscope allows viewing of the subgingival area during instrumentation provides significant clinical benefits. Scaling and root planing is designed to thoroughly remove deposits, but this is often difficult to accomplish with traditional instrumentation.11–14Scaling and/or root planing aided by the indirect vision provided by the dental endoscope, or perioscopy, may improve periodontal therapy outcomes.1,4–6,10
Clinicians most often rely on tactile evaluation with an explorer to assess the success of calculus removal in periodontal pockets. However, Sherman et al11 found this method to be problematic. The researchers examined extracted teeth that had been identified by clinicians as “calculus free” and found that 77% still had subgingival calculus present. The presence of retained subgingival deposits, often demonstrated by bleeding on probing, inhibits periodontal healing.4,6,15
Perioscopy—the extension of traditional scaling and root planing with clinicians visualizing periodontal pockets indirectly on a monitor—is designed to improve the ability to detect and remove calculus.1,4,10Perioscopy has a supportive body of evidence behind its effectiveness. Geisinger et al5 performed scaling and root planing on periodontally involved, single-rooted teeth. The single-rooted teeth were either instrumented with the aid of the dental endoscope or instrumented without the endoscope. The teeth instrumented with the assistance of the endoscope exhibited significantly less calculus than those that were instrumented blind. Michaud et al16 performed a similar study on multi-rooted teeth. One group was treated with perioscopy, while the other received only scaling and root planing. Interproximal surfaces treated with perioscopy had less residual calculus than the blind scaling and root planing group, but no statistically significant differences were found in the amount of residual calculus at deeper probing depths or at sites with deep furcations.16
The ability to detect subgingival calculus on nonextracted teeth using the endoscope vs an explorer on patients with moderate periodontitis was also investigated by Osborn et al.17 After undergoing scaling and root planing, one quadrant from each subject was randomly assigned to tactile calculus detection with the explorer or tactile detection with the endoscope. Significantly more calculus was detected using the endoscope than the explorer. Further, the researchers found that the endoscope was most beneficial in the re-evaluation phase of periodontal therapy.17 Wilson et al18 found histological signs of chronic inflammation were absent 6 months after a single course of closed subgingival scaling and root planing with the dental endoscope. More research is needed to determine whether the endoscope is most beneficial when used at the initial or re-evaluation phase of periodontal therapy.
Excess cement on implant prostheses is problematic because the same microbes that contribute to the inflammatory response in periodontitis can remain on the excess cement. The dental endoscope can help clinicians detect cement that is inadvertently left behind. Wilson19 used the endoscope to evaluate implants exhibiting clinical and/or radiographic signs of peri-implant disease both before and after the removal of cement. After removal of excess cement, clinical and endoscopic signs of peri-implant disease were resolved in 74% of the test implants.19
Research shows that the dental endoscope can be a helpful adjunct to periodontal therapy. The downside to implementing it into practice are high cost and the need for highly skilled users.1,10 Significant training and practice are necessary in order for a clinician to become effective in using the endoscope.1,10 While the learning curve and cost may be limitations, the endoscope improves clinician visualization and magnification of the subgingival root surface and may improve patient outcomes.
An advance in visual technology is the dental videoscope, which provides a more accurate subgingival view than is provided by the dental endoscope or loupes (Figure 2). The dental videoscope creates real-time images that are magnified by 20 times to 60 times. This is possible because the device uses a camera at the end of the scope that transfers the image to a monitor. Designed to provide visualization of undetectable calculus deposits, it enables practitioners to remove calculus while directly viewing it.20,21 The dental videoscope is best suited for use on patients with deep probing depths and in cases where regeneration of lost periodontal attachment is the intended result. Cost and technique sensitivity are relative issues, just as with the dental endoscope.20,21
MAGNIFICATION
Other types of magnification are used by oral health professionals, such as dental microscopes, loupes, and intraoral cameras. Advantages of using magnification include improved visualization at the diagnostic and treatment levels. The dental microscope is most frequently used in endodontics, restorative dentistry, and periodontics, while dental hygienists more commonly utilize loupes and intraoral cameras.

The literature regarding magnification often focuses on ergonomic benefits, such as posture improvement and reduced risk for musculoskeletal disorders. Although it is well-documented that loupes can enhance patient care and provide ergonomic benefits for clinicians, Congdon et al22 found that most dental hygiene educators in the United States have not embraced the use of loupes in their institutions nor require them for student use. This hesitation may be related to experiences with ill-fitting loupes. Improperly fitted loupes may result in an increased risk of musculoskeletal disorders.2,23,24
The use of loupes combined with high-intensity coaxial lighting also improves visual acuity for clinicians.25 Lighting is important because as the level of magnification increases, the field of view becomes darker, thus making it more difficult to see into the oral cavity without straining the eyes and neck. Clinicians should also consider the field of view. Most dental hygienists may find that increasing magnification to 2 times to 2.5 times the field of view is adequate to see in the oral cavity. Using higher magnification will reduce the field of view to fewer teeth, but this may be preferred by some practitioners. Other fit considerations include: declination angle, depth of field, and comfort.15,23,24
While not a magnification tool, high-definition mouth mirrors may also improve clinicians’ visual acuity. New versions offer high-resolution viewing and anti-fog solutions to prevent the mirror from fogging up during treatment. Mirrors combined with a light source and technology that eliminates water and debris from the mirror face are additional advancements designed to help clinicians keep a clear field of view.26
INTRAORAL CAMERAS
Intraoral cameras are used routinely for visual examinations, documentation, and patient education.27 They employ high-power magnification and light-emitting diode (LED) technology to provide detailed information to both clinicians and patients. Clinicians should consider several factors before purchasing an intraoral camera. A variable focus camera offers clearer images and an extra/intraoral range of focus, but is more expensive than a fixed-focus camera that has a limited range of focus. Images of soft tissue lesions, caries, fractured teeth, ill-fitting restorations, calculus, and recession are conditions that can be captured by an intraoral camera and stored in the patient record. Most important, these images can be used in assessment, diagnosis, referral, education, and treatment planning.27
DIGITAL RADIOGRAPHY
Digital radiography provides numerous benefits to both clinicians and patients. Clinicians are able to view images instantly and enlarge or improve the quality. Direct digital sensors used for bitewing and peri-apical images can reduce patient exposure to radiation (compared to film-based images) and advancements in sensor design have improved patient comfort and decreased the need for re-exposures.9,28 Cone-beam computer tomography (CBCT) scans, which provide three-dimensional images, are also seen with increasing frequency in dental offices. CBCT imaging is useful in orthodontics, to improve treatment planning, and in evaluating other oral conditions, but it may increase patients’ exposure to radiation.9,29,30 The American Dental Association Council on Scientific Affairs states that CBCT imaging should be used “only after a review of the patient’s health and imaging history and completion of a thorough clinical examination.”31
Digital radiography benefits include the ability to measure bone height and improve image quality without retakes. Digital images can be stored, accessed easily, and enlarged for patient education, as well as transmitted electronically for patient referrals.7
SUMMARY
Advances in technology have made significant improvements in visual acuity, benefiting both clinicians and patients. Dental hygienists play an integral role in reviewing the evidence and determining which of these modalities will support them in their quest for excellent patient care.
REFERENCES
- Stambaugh RV, Myers G, Ebling W, Beckman B, Stambaugh K. Endoscopic visualization of the submarginal gingiva dental sulcus and tooth root surfaces. J Periodontol. 2002;73:374–382.
- Sunnell S, Rucker L. Surgical magnification in dental hygiene practice. Int J Dent Hygiene. 2004;2:26–35.
- Branson BG, Bray KK, Gadbury-Amyot C, et al. Effect of magnification lenses on student operator posture. J Dent Ed. 2004;68:384–389.
- Stambaugh RV. Perioscopy, the new paradigm. Dimensions of Dental Hygiene. 2003;1(2):12–16.
- Geisinger ML, Mealey BL, Schoolfield J, Mellonig JT. The effectiveness of subgingival scaling and root planing: An evaluation of therapy with and without the use of the periodontal endoscope. J Periodontol. 2007;78:22–28.
- Pattison AM, Pattison GL. Periodontal instrumentation transformed. Dimensions of Dental Hygiene. 2003;1(2):18–22.
- Greco N. Advantages of digital radiography. Dimensions of Dental Hygiene. 2014;12(12):43–46.
- Attanasi K. Digital dental imaging. Dimensions of Dental Hygiene. 2013;11(1):48–51.
- Thomson EM, Johnson ON. Essentials of Dental Radiography for Dental Assistants and Hygienists. 10th ed. Upper Saddle River, New Jersey: Pearson; 2018.
- Stambaugh RV. A clinicians’ 3-year experience with perioscopy. Compendium. 2002;23:1061–1070.
- Sherman PR, Hutchens LH Jr, Jewson LG, Moriarity JM, Greco GW, McFall WT. The effectiveness of subgingival scaling and root planning. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control II. As observed on extracted teeth. J Periodontol.1978;49:119–124.
- Rabbani GM, Ash MM, Caffesse RG. The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol. 1981;52:119–123.
- Nagy RJ, Otomo-Corgel J, Stambaugh R. The effectiveness of scaling and root planing with curets designed for deep pockets. J Periodontol. 1992;63:954–959.
- Michaelides P, Stambaugh R. Zooming in on magnification. Dimensions of Dental Hygiene. 2007;5(4):16–21.
- Michaud RM, Schoolfield J, Mellonig JT, Mealey BL. The efficacy of subgingival calculus removal with endoscopy-aided scaling and root planing: A study on multirooted teeth. J Periodontol. 2007;78:2238–2245.
- Osborn JB, Lenton PA, Lunos SA, Blue CM. Endoscopic vs tactile evaluation of subgingval calculus. J Dent Hyg. 2014;88:229–236.
- Wilson TG, Carnio J, Schenk R, Myers G. Absence of histological signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: Human biopsies—a pilot study. J Periodontol. 2008:79:2036–2041.
- Wilson TG. The positive relationship between excess cement and peri-implant disease: A prospective clinical endoscopic study. J Periodontol. 2009:80:1388–1392.
- Pope J. Improve the view. Dimensions of Dental Hygiene. 2016;14:53–56.
- Harrel SK, Abraham CM, Rivera-Hidalgo F, Sbulman J, Nunn M. Videoscope-assisted minimally invasive periodontal surgery (V-MIS). J Clin Periodontol. 2014;41:900–907.
- Congdon LM, Tolle SL, Darby M. Magnification loupes in U.S. entry-level dental hygiene programs—occupational health and safety. J Dent Hyg. 2012;86:215–222.
- Rucker, LM. Surgical Magnification: Posture maker or posture breaker? IN Murphy D. Ergonomics and the Dental Care Worker. Washington, DC: American Public Health Association; 1998:191–216.
- Ludwig EA, Tolle SL Ensure proper fit. Dimensions of Dental Hygiene. 2017;15(4):24–26.
- Holt ER, Hoebeke R. Shine a light. Dimensions of Dental Hygiene. 2012;10(9):25–27.
- Bly J, Jordre BD. Improve visibility. Dimensions of Dental Hygiene. 2015;13(1):18–23.
- Cooper B. A picture is worth a thousand words. Dimensions of Dental Hygiene. July 2015; 13(7):28,30.
- Bruhn AM, Newcomb TL, Tolle, SL. Ensuring safe practice in dental radiology. Dimensions of Dental Hygiene. 2015;13(12):30–33.
- Scarfe WC, Pinheiro LR, Farman AG. Strategies for the safe use of CBCT. Dimensions of Dental Hygiene. 2015;13(2):20–22.
- Naylor C, Christensen RT. High tech diagnostic tools. Dimensions of Dental Hygiene. 2014;12(4):16–19.
- American Dental Association Council on Scientific Affairs. The use of cone-beam tomography in dentistry. An advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902.
From Dimensions of Dental Hygiene. June 2017;15(6):28-30.

