 KSENIABAZAROVA/ISTOCK/GETTY IMAGES PLUS
KSENIABAZAROVA/ISTOCK/GETTY IMAGES PLUS
A Safe Approach to Aerosols
Reducing aerosols in the dental setting is key to proper infection control protocol.
Aerosols are generated by a variety of dental procedures. Oral health professionals have always been aware of aerosols and pathogens; however, the COVID-19 pandemic brought the issue to the forefront. Several guidance documents were published by a number of stakeholders in dentistry at the beginning of the pandemic recommending a variety of safety strategies, including pre-screening patients with questions and temperature checks, staggering of patient appointment times, decreasing the number of patients in the facility, changes to personal protective equipment (PPE), and aerosol mitigation strategies, such as high-velocity air evacuation (HVE), or high-volume evacuation.1,2
Guidance Documents
The Occupational Safety and Health Administration (OSHA) has published several standards designed to protect oral health professionals from harmful blood and chemicals including the bloodborne pathogens standard (BBP),3 hazard communication standard,4 and respiratory protection standard.5 The OSHA respiratory standard 1910.134 protects workers from respiratory hazards.5 The employer must provide a written worksite-specific protocol that outlines procedures for assessment of respiratory hazards and protective measures, and must select and provide appropriate respirators based on those exposure hazards. Common respiratory exposure hazards in dentistry include aerosol generating procedures (AGPs) such as the use of high-speed handpieces, ultrasonic scalers, air powder polishers, and air-water syringes.6,7 The OSHA risk pyramid considers AGPs as “very high risk” because sprays from these procedures can aerosolize microorganisms and blood.7,8 Visible spray from AGPs contain large particle droplets that travel quickly and settle on surfaces, whereas smaller microorganism containing aerosols < 10 µm can remain airborne for long periods, which can then be inhaled.6,9 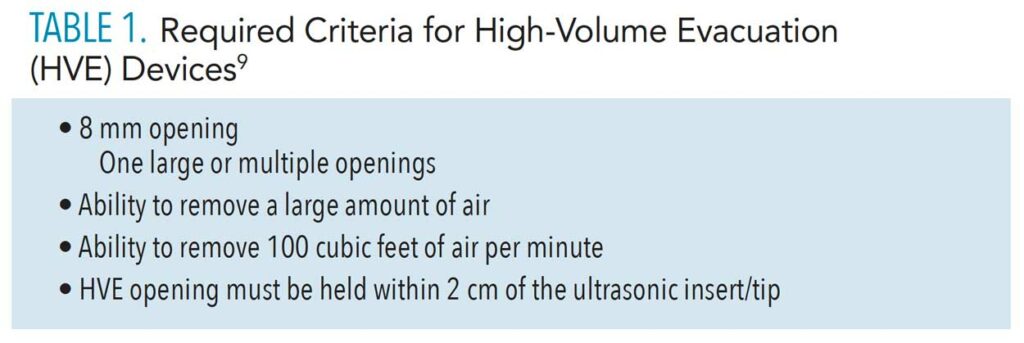
Aerosols
Potentially contaminated patient body fluids can become airborne during dental procedures in the form of spatter or aerosols. Spatter is large droplet spray larger than 50 micrometers known as microns (µm) that follows a forceful trajectory until it contacts a surface or settles on the floor, not staying airborne for very long.6 Aerosol is also measured in microns generally 0.5 µm to 10 µm in diameter, which can remain airborne for an extended time.6 These smaller particles can penetrate the filters of surgical masks and enter the respiratory tract.9
Several aerosol mitigation strategies are available for use with AGPs including rubber dams; HVE; preprocedural mouthrinses; proper PPE (respirators, goggles, face shield, gown, gloves); staggering of patients; air purification devices; positive pressure ventilation (if feasible); and possibly fallow time (time the operatory is remains empty to allow the clearance/settling of aerosols).1,2 Positive pressure ventilation built into the heating, ventilation, and air conditioning system eliminates small aerosols by continuous fresh air intake and venting air to the outside.10 HVE is recommended, however, four-handed dentistry is necessary as a dental assistant uses the HVE while procedures are performed by the dentist or dental hygienist. Unfortunately, dental hygienists generally work without the help of a dental assistant, so the use of HVE has been slow to become routine practice.
Ultrasonic instrumentation is considered an AGP that requires HVE.2,6 Aerosol spatter from ultrasonic scalers can be emitted up to 18 inches from the tip.11 Many dental hygienists use saliva ejectors to control fluids, which do not provide enough adequate protection from aerosols.12 Also, most dental hygiene procedures do not lend themselves to the use of a rubber dam, so reliance on HVE and proper PPE is necessary.
Many new HVE devices are available. The clinician must determine which product suits his or her needs. Suction devices must meet specified criteria to be considered HVE, so clinicians should keep this in mind when selecting HVE devices.

Criteria for High-Volume Evacuation
Several research studies indicate HVE significantly reduces aerosols by up to 90%.9,11,12 An HVE device must have a large opening of at least 8 mm, must quickly remove a large amount of air, and must remove up to 100 cubic feet of air per minute (Table 1).9 Typical HVE devices have either a large opening greater than 8 mm or multiple bore holes equivalent to 8 mm (Figure 1).9 Any device with an opening less than 8 mm is considered low-volume evacuation (LVE), which is adequate for fluid control, but not for aerosol control as the diameter of the opening is too small (Figure 2).9 Saliva ejectors are LVE devices.9
It is best to capture aerosols in the mouth before they get a chance to become airborne. Harrel11 states this can be achieved by holding the HVE within 2 cm of the ultrasonic tip, which can be difficult as a solo operator. It is imperative to keep the HVE within the 2 cm distance to provide optimal aerosol reduction whether employing a dental assistant or working solo.11
Several studies indicate HVE remains the gold standard for use with AGPs and is in alignment with prior and current CDC guidance.1,6,9,11–17 A recent study by Ehtezazi et al14 tested fallow time after six AGPs were performed in vitro on mannequin heads with a combination of HVE devices. They found that all of the HVE types significantly reduced aerosols, but did not completely eliminate them, so proper PPE along with HVE continue to be the best strategy. Shahad et al15 also suggested HVE as a primary aerosol mitigation strategy. Another study by Li et al16 found that HVE reduced aerosols by 60% as compared to LVE. Suprono et al17 noted significant aerosol reduction with ultrasonic scaling when HVE was used.

Types of Devices
Several types of HVE devices exist. Important factors to consider include the assessment of ergonomics, efficiency, effectiveness, and design. For proper ergonomics, HVE devices must be lightweight and easily managed by a solo clinician. Long, heavy, or coiled hoses cause tension on the wrist and arm, which can lead to musculoskeletal issues.18 Gupta et al18 recommend devices that swivel with flexible hoses for better ergonomics.
A variety of ergonomically sound HVE devices is available. One type attaches to the finger of the nondominant hand and provides a lightweight variable tip—with an 11-mm bore opening—that rotates 360°, making it easy to achieve the 2 cm distance.19 This fingertip device allows the operator to maintain a neutral wrist position.
A second type is a combined mouth mirror and HVE that either has a large 10 mm opening or several bore holes alongside the mirror back and sides that total 8 mm or more. This mirror-suction device allows for retraction, vision, fluid control, and aerosol control (Figure 3).
The third type of HVE device serves as a mouth prop or bite block combined with HVE. These bite block devices, also known as “dry field devices,” provide excellent fluid and aerosol control with bore openings greater than 8 mm in addition to helping patients keep their mouths open.20 Bite block devices help with efficiency because an entire side of the mouth can be completed without stopping or readjusting the bite block. The bite block is placed on the left side while the operator instruments the entire right side (maxillary and mandible), then it is readjusted to the right side while the operator instruments the left side. Bite block HVE devices are convenient, but may not be compatible for all patients as they can be large and they cover the oropharynx. This could be problematic for patients who gag, have difficulty breathing through the nose, have a small mouth, need to feel a sense of control, or need to swallow frequently.
A final device category is a flexible autoclavable suction tube that attaches to an ultrasonic scaler with a small clamp, capturing aerosols near the source of the tip and freeing up the nondominant hand for mirror use. This device was shown to reduce aerosols by 93%.21
Shortened or curved HVE tips can be used alone by the dental hygienist or with an assistant. When these devices are used, the tip should be angled to avoid suctioning the lips, buccal mucosa, or tongue.22
Large extraoral suction units called extraoral local extractors (ELE) utilize an arm with a cone or cup shape that is placed near the patient’s mouth to capture aerosols, but these are quite costly.23 Noordien et al23 found a 53% reduction in aerosols when ELE was used in conjunction with both an HVE and LVE as compared to an LVE alone. The ELE device could be a useful hands-free adjunct to HVE, but needs further study.24

Future Research Questions
Much of the literature suggests HVE is the primary mitigation method in aerosol management. However, three general themes arise for future research consideration:
1. Black and white categorization of procedures into either AGP or non-AGP is overly simplistic due to micron size and causes ambiguity.25,26 A range of procedures may or may not fall directly into one of these categories and needs further definition and investigation.26 Future research in this area should consider stratifying risk based on procedure types.26
2. The issue around the infectivity and transmission of viruses, like SARS-CoV-2, through dental aerosols.25–28 So far, there have been no documented cases of SARS-CoV-2 transmission related to AGPs in dentistry.28 This phenomenon is new and requires further study.24,26
Most studies of AGP use settle plates to detect droplets that have fallen.25,29 We know that droplets settle quickly while aerosols persist for longer periods, so settle plates may not be capturing the needed information.25,29 Settle plate methods are also problematic in that most microbiological studies measure bacterial colony forming units (CFU) with low sensitivity rather than measuring the transmissibility of viruses.25,27,29 Bacterial CFU are much larger than aerosols which are measured in microns.
Conclusion
No one device works for everyone. Clinicians must use their best judgement based on sound evidence, HVE criteria, personal preference, and ergonomics. Harrel and Molinari9 discuss a layered approach to safety with aerosols including use of proper PPE, pre-procedural mouth rinses, HVE, and operatory HEPA air filtration all of which remains consistent with current infection control guidance.
References
- United States Centers for Disease Control and Prevention. Guidance for Dental Settings. Interim Infection Prevention Control Guidance for Dental Settings During the Coronavirus Disease 2019 (COVID 19) Pandemic. Available at: cdc/g/v/coronavirus/떓-ncov/hcp/dental-settings.html. Accessed February 22, 2022.
- American Dental Hygienists’ Association. ADHA Interim Guidance on Returning to Work. Available at: adha.org/resources-docs/_D_A_TaskForceReport_著_C.pdf. Accessed February 22, 2022.
- Occupational Safety and Health Administration. Bloodborne Pathogens Standard 1910.1030. Available at: osha.gov/laws-regs/regulations/standardnumber/딦/딦.1030. Accessed February 22, 2022.
- Occupational Safety and Health Administration. Hazard Communication Standard 1910.1200. Available at: osha.gov/laws-regs/regulations/standardnumber/딦/딦.1200. Accessed February 22, 2022.
- Occupational Safety and Health Administration. Respiratory Protection Standard 1910.134. Available at: osha.gov/laws-regs/regulations/standardnumber/딦/딦.134. Accessed February 22, 2022.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for Infection Control in Dental Health-Care Settings 2003. MMWR Morb Mortal Wkly Rep. 2003;52(RR-17):1–61.
- Occupational Safety and Health Administration. COVID-19 Control and Prevention. Dentistry Workers and Employers. Available at: osha.gov/coronavirus/control-prevention/dentistry. Accessed February 22, 2022.
- Occupational Safety and Health Administration. COVID-19 Hazard Recognition. Available at: osha.gov/coronavirus/hazards. Accessed February 22, 2022.
- Harrel SK, Molinari J. Aerosols and splatter in dentistry. A brief review of the literature and infection control implicationsJ J Am Dent Assoc. 2004;135:429–37.
- Sprau M, Evans S. Dental design concepts for infection prevention & air quality. J Dent Infect Control & Safety. 2021;3:28953.
- Harrel SK. Clinical insights: proceed with caution. Dimensions of Dental Hygiene. 2020;18(7):16–21.
- Harrel SK. Clinical insights: what we know and don’t know about dental aerosols. Dimensions of Dental Hygiene. 2020;18(5):16–18.
- Jacks M. Protecting Yourself. Dimensions of Dental Hygiene. 2011;9(8):26–29.
- Ehtezazi T, Evans DG, Jenkinson ID, et tal SARS-CoV-2: characterisation and mitigation of risks associated with aerosol generating procedures in dental practices. Br Dent J. 202;7:1–7.
- Shahdad S, Hindocha A, Patel T, et al. Fallow time determination in dentistry using aerosol measurement in mechanically and non-mechanically ventilated environments. Br Dent J. 2021;24:1–8.
- Li X, Mak CM, Ma KW, Wong HM. How the high-volume evacuation alters the flow-field and particle removal characteristics in the mock-up dental clinic. Build Environ. 2021;205:108225.
- Suprono MS, Won J, Savignano R, et al. A clinical investigation of dental evacuation systems in reducing aerosols. J Am Dent Assoc. 2021;152:455–462.
- Gupta A, Bhat M, Mohammed T, Bansal N, Gupta G. Ergonomics in dentistry. Int J Clin Pediatr Dent. 2014;7:30–34.
- Dimensions of Dental Hygiene. Improve Your Ergonomics and Aerosol Control. Available at: dimensionsofdentalhygiene.com/article/improve-your-ergonomics-aerosol-control/. Accessed February 22, 2022.
- Holloman JL, Mauriello SM, Pimenta L, Arnold RR. Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. J Am Dent Assoc. 2015;146:27–33.
- Harrel SK, Barnes JB, Rivera-Hidalgo F. Reduction of aerosols produced by ultrasonic scalers. J Periodontol. 1996;67:28–32.
- Emmons L, Wu C, Shutter T. High-volume evacuation: Aerosols-it’s what you can’t see that can hurt you. Available at: rdhmag.com/patient-care/article/ླ/highvolume-evacuation-aerosolsits-what-you-cant-see-that-can-hurt-you. Accessed February 22, 2022.
- Noordien N, Mulder-van Staden S, Mulder R. In Vivo study of aerosol, droplets and splatter reduction in dentistry. Viruses. 2021;13:1928.
- Ou Q, Grazzini R, Danielson J, et al. Characterization and mitigation of aerosols and spatters from ultrasonic scalers. J Am Dent Assoc. 2021;152:981–990.
- Innes N, Johnson IG, Al-Yaseen W, et al. A systematic review of droplet and aerosol generation in dentistry. J Dent. 2021;105:103556.
- Virdi MK, Durman K, Deacon S. The debate: what are aerosol-generating procedures in dentistry? A rapid review. JDR Clin Trans Res. 2021;6:115–127.
- Johnson IG, Jones RJ, Gallagher JE, et al. Dental periodontal procedures: a systematic review of contamination (splatter, droplets and aerosol) in relation to COVID-19. BDJ Open. 2021;7:15.
- Geisinger MI, Iaonnidou E. Up in the air? Future research strategies to assess aerosols in dentistry. JDR Clin Trans Res. 2021;6:128–131.
- Ionescu AC, Cagetti MG, Ferracane JL, Garcia-Godoy F, Brambilla E. Topographic aspects of airborne contamination caused by the use of dental handpieces in the operative environment. J Am Dent Assoc. 2020;151:660–667. A Safe
From Dimensions of Dental Hygiene. March 2022;8(3):16-18.

