A Diagnostic Challenge
While a large radiopaque mass of the maxilla could represent a variety of oral health problems, a differential diagnosis is the key to pinpointing the cause.
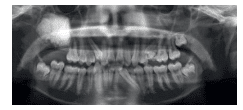
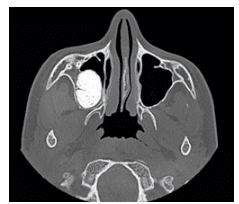
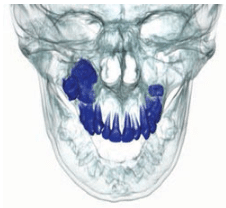
This case report is of a 15-year-old boy who presented for orthodontic treatment at a military base dental clinic. Upon radiographic examination, a large radiopaque mass was noted in the patient’s right maxilla (Figure 1).Computed tomography scans revealed that the mass was encroaching upon the posterior wall of the maxillary sinus (Figure 2 to Figure 4). The maxillary right second and third molars were impacted and associated with the lesion (Figure 5). The patient was asymptomatic. He had no sensation of fullness, history of swelling, or visual disturbance. Previous radiographs were unavailable for review. Several diagnoses are possible for a large radiopaque mass of the maxilla, including ameloblastic fibro-odontoma (AFO), compound odontoma, complex odontoma, ossifying fibroma, and cementoblastoma. A differential diagnosis is necessary to determine the correct cause of this lesion.
COMPOUND AND COMPLEX ODONTOMAS
Odontomas are the most common type of odontogenic tumors;1 however, the vast majority represent hamartomas or developmental anomalies—not true neoplasms.2 Odontomas consist of enamel, dentin, cementum, and pulp. In some instances, proliferating odontogenic epithelium and ectomesenchyme in the form of dental papilla can be observed.
Based on their gross appearance and radiographic and microscopic features, odontomas are classified as either compound or complex.3 Compound odontomas resemble misshapen teeth and have a predilection for the anterior maxillary region. In general, compound odontomas occur more frequently than complex odontomas. Complex odontomas are amorphous masses of calcified tissue. Grossly, complex odontomas do not morphologically resemble teeth and they have a predilection for the posterior segments of the jaws.
Odontomas are typically slow growing and are usually detected in the second decade of life.2 Most odontomas are asymptomatic and typically discovered during routine radiographic evaluation. Many are identified after a radiograph is prescribed due to the failure of a permanent tooth to erupt. Odontomas can be associated with impaction, delayed eruption, and malposition of adjacent teeth. Cyst formation and resorption of neighboring roots are also observed.2,4
The cause of odontomas is unknown. Several theories have been proposed, including local trauma or infection.5 An underlying genetic association has been observed with Gardner’s syndrome, which is a genetic disorder caused by a mutation of the adenomatous polyposis coli located in chromosome 5q21.6 The most important feature of this syndrome is the presence of premalignant intestinal polyps. Prophylactic colectomy is typically recommended in order to prevent the development of gastro-intestinal malignancy. Numerous dental anomalies are associated with Gardner’s syndrome, including multiple supernumerary teeth, osteomas, and odontomas.6 Odontomas are most often surgically removed with excellent prognosis.
AMELOBLASTIC FIBROMA–ODONTOMA
AFO is a true neoplasm, exhibiting both neoplastic epithelial and mesenchymal elements.1 Inductive changes that lead to the formation of enamel and dentin are observed. While some AFOs may be indistinguishable from large complex odontomas, radiographically AFOs exhibit a significant radiolucent component rather than the thin radiolucent halo observed in this patient. AFOs are relatively rare, representing only 1% of all odontogenic tumors.7 They favor a younger age group, with most cases reported in the first 20 years of life. About 70% of all cases of AFOs are diagnosed in the posterior mandible.1 Because AFOs are not locally invasive, the preferred treatment is surgical removal of the lesion.8
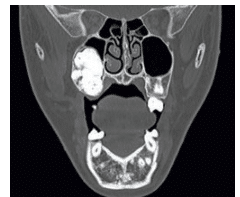 FIGURE 3. A coronal computed tomography scan illustrating a radiopaque mass involving the right maxilla and encroaching upon the maxillary sinus.
FIGURE 3. A coronal computed tomography scan illustrating a radiopaque mass involving the right maxilla and encroaching upon the maxillary sinus.
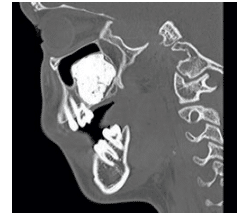 FIGURE 4. A sagittal computed tomography scan demonstrates a radiopaque lesion of the maxilla elevating the sinus.
FIGURE 4. A sagittal computed tomography scan demonstrates a radiopaque lesion of the maxilla elevating the sinus.
OSSIFIYING FIBROMA
Ossifying fibroma is a rare benign fibro-osseous neoplasm of the jaw. This lesion appears as a well-demarcated mass and has significant growth potential. The lesion replaces normal bone with a newly formed fibrous tissue with varying amounts of mineralized product.9 This mineralized product is similar to bone or cementum. Ossifying fibromas occur in patients in their 20s to 40s and are slightly more common in women. The mandible is involved more frequently than the maxilla. Early lesions can be radiolucent, but as lesions mature they become more sclerotic. The nature of the radiopacity is a bit more mottled than in odontomas and is typically not as radiopaque.
CEMENTOBLASTOMA
Cementoblastoma is a neoplasm of cementoblasts. It is a rare odontogenic neoplasm characterized by the formation of cementum or cementum-like tissue that is attached to the root(s) of a tooth. The lesion has also been referred to as a “true cementoma.”9 Cementoblastomas are distinctive in that they are always fused to the roots of the associated teeth. Although they produce radicular resorption, the tooth remains vital.10
The tumor mostly arises in the permanent dentition,11 and more than 50% of the cases involve the mandibular first molar.12 Some cases have been reported involving the premolars and rare reports exist in which cementoblastomas were found affecting the primary dentition.11 These tumors primarily affect young adults in their 30s and 40s, with approximately half occurring in those younger than 20.12 Cementoblastomas typically present with pain and swelling due to bony expansion of the buccal and lingual aspects of the alveolar ridges.11–13
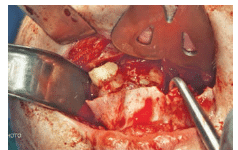 FIGURE 6. The lesion is surgically excised.
FIGURE 6. The lesion is surgically excised.
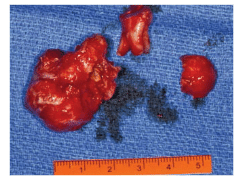 FIGURE 7. The lesion after it has been surgically removed.
FIGURE 7. The lesion after it has been surgically removed.
DIAGNOSIS REACHED
To determine the correct diagnosis, an incisional biopsy of the mass was performed and the excised tissue was submitted for histopathologic evaluation. Microscopic sections showed an amorphous mass of mineralized tissue consistent with dentin and enamel matrix. Focal areas revealed fragments of odontogenic epithelium. An area of dental papilla was observed. These data supported complex odontoma as the final diagnosis.

After the diagnosis was reached, a final surgical procedure was accomplished under general anesthesia that included a lefort osteotomy with a partial down fracture through the maxilla (Figure 6). The lesion was removed in its entirety with enucleation and curettage (Figure 7 and Figure 8). In addition, teeth numbers 1, 5, 12, 16, 17, 21, 28, and 32 were extracted for orthodontic purposes. At the 2-month follow-up appointment, the patient reported some residual numbness of the palate. Adequate healing of the surgical site was documented.
Determining the correct diagnosis can be challenging in oral pathology, where there can be several possible etiologies for a problem. Dental professionals must be prepared to perform a differential diagnosis to ensure that the correct cause is determined so the appropriate course of treatment can begin. Dental hygienists play key roles in noting abnormalities in the oral cavity and ensuring patients maintain their oral health.
REFERENCES
- Reichart PA, Philipsen HP. [Revision of the 1992 edition of the WHO histological typing of odontogenic tumors. A suggestion]. Mund Kiefer und Gesichtschirurgie. 2003;7:88–93.
- Budnick SD. Compound and complex odontomas. Oral Surg Oral Med Oral Pathol. 1976;42:501–506.
- Kaneko M, Fukuda M, Sano T, Ohnishi T, Hosokawa Y. Microradiographic and microscopic investigation of a rare case of complex odontoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.1998;86:131–134.
- Astekar M, Manjunatha BS, Kaur P, Singh J. Histopathological insight of complex odontoma associated with a dentigerous cyst. BMJ Case Rep. 2014 January 31.
- Kodali RM, Venkat Suresh B, Ramanjaneya Raju P, Vora SK. An unusual complex odontoma. J Maxillofac Oral Surg. 2010;9:314–317.
- Fonseca LC, Kodama NK, Nunes FC, et al. Radiographic assessment of Gardner’s syndrome. Dentomaxillofac Radiol. 2007;36:121–124.
- Cavalcante AS, Anbinder AL, Costa NC, Lima JR, Carvalho YR. Ameloblastic fibro-odontoma: a case report. Med Oral Patol Oral Cir Bucal. 2009;14:e650–653.
- Reis SR, de Freitas CE, do Espírito Santo AR. Management of ameloblastic fibro-odontoma in a 6-year-old girl preserving the associated impacted permanent tooth. J Oral Sci. 2007;49:331–335.
- Kramer IR, Pindborg JJ, Shear M. The World Health Organization histological typing of odontogenic tumours. Introducing the second edition. Eur J Cancer B Oral Oncol, 1993;29B:169–171.
- Pynn BR, Sands TD, Bradley G. Benign cementoblastoma: a case report. J Can Dent Assoc. 2001;67:260–262.
- Vieira AP, Meneses JM, Maia RL. Cementoblastoma related to a primary tooth: a case report. J Oral Pathol Med. 2007;36:117–119.
- Ulmansky M, Hjørting-Hansen E, Praetorius F, Haque MF. Benign cementoblastoma. A review and five new cases. Oral Surg Oral Med Oral Pathol. 1994;77:48–55.
- Ackermann GL, Altini M. The cementomas–a clinicopathological re-appraisal. J Dent Assoc S Afr. 1992;47:187–194.
From Dimensions of Dental Hygiene. September 2014;12(9):54–56.

