Cultural Competency
How to incorporate different cultural beliefs and practices into the dental hygiene process of care.
This course was published in the April 2012 issue and expires April 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain why cultural competency is important to the provision of oral health care.
- List the five components of cultural competence.
- Identify strategies for implementing cultural competency into the process of care.
- Discuss the use of the ETHNIC mnemonic.
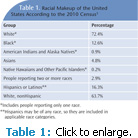
Over the past 10 years, the demographics of the United States have changed dramatically—creating a more diverse patient population.1,2 According to the United States Census Bureau, more than half of the population growth observed between the 2000 and 2010 census was due to an increase in the number of Hispanic residents, although the Asian population experienced the greatest growth as a group—increasing by 43%. During the same decade, the number of white, nonHispanics grew at the slowest rate. The Black population also experienced slow growth, increasing by 12% between 2000 and 2010.3 Table 1 provides additional population demographics.3 While the American population has become more diverse, the number of minorities working in the nation’s health care professions is not reflective of these new demographics.
Many initiatives are ongoing to encourage greater diversity in the health care professions.4 With this greater diversity comes the need for improved cultural sensitivity, especially among health care workers. Insensitivity to cultural differences can impede the ability of patients to access and effectively receive health care.5 All aspects of health care—including dental care—must adapt to improve cultural competency. While cultural initiatives are common in education, social services, law, and medicine, related educational resources in dentistry and dental hygiene are limited.2
The Institute of Medicine’s 2011 “Advancing Oral Health in America” report acknowledges the importance of improving cultural competence of the dental workforce.1 Combining culturally-sensitive assessment strategies with the dental hygiene process of care allows clinicians to integrate a culture-specific competency into the traditional care plan. The failure to develop these skills may compromise the quality of and access to care, limit patient resources, threaten patient safety, and perpetuate oral health disparities.6,7
The Process
Culture is a specific set of social, educational, religious, and professional behaviors, practices, or values that individuals learn and adhere to daily,8 including communication styles, customs, dress, cultural beliefs, and societal rules.9,10 Cultural competency is the ability to effectively communicate with people of diverse backgrounds.2,11,12 In health care, cultural competency also relates to the provider’s ability to acknowledge cultural influences on patients’ health-related beliefs and behaviors, and to understand how these influences affect the provision of care.2,11–13
The process of cultural competence includes five components: cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desire. Cultural awareness is based on understanding the provider’s own cultural background and becoming aware of others’ values, beliefs, and practices.11–13 Through this process, personal biases, prejudices, and assumptions about patients of diverse backgrounds may be identified and addressed.11
Cultural knowledge is rooted in learning about the world views of diverse groups,11–13 which includes understanding how to define culture and describe cultural beliefs, values, and behaviors of different populations. Cultural knowledge also includes engaging in collaborative discussions with patients about their cultural influences.11,12
Cultural skill is the ability to collect relevant cultural data regarding patients’ health problems and perform a culturally-based, physical and interview assessment.9,11–13 A cultural assessment investigates the beliefs, values, and practices of individuals, groups, and communities, in order to ascertain particular needs and treatment strategies.12
Experiencing cultural encounters is an important component of cultural competency.
Dental hygienists will better understand culture groups on a personal level through participation in multicultural activities. Exposure to cultural experiences may also encourage dental professionals to participate in public health events.11,13,14 Lastly, cultural desire involves caring for all patients equally, regardless of their cultural values and beliefs, and the motivation to develop cultural awareness, knowledge, and skills.11,13,14 Cultural competence is a process—a culturally competent dental hygienist strives to recognize and incorporate different cultural beliefs and practices into the dental hygiene process of care.6
IMPLEMENTATION INTO DENTAL HYGIENE PRACTICE
Individuals are most likely to cling to cultural values/beliefs during times of pain and anxiety.8,15 Culturally-based health beliefs influence medical decision making, and all forms of communication (verbal and nonverbal) are relative. Language barriers can limit patients’ abilities to communicate and understand health information.16 Dental hygienists can use interpreters, visual aids, and language-specific educational tools to maximize preparedness for cultural encounters.9,17 A translator educated in medical/dental terminology is preferred to explain treatment procedures effectively.
The young children of patients should not be used to interpret treatment plans or procedures.9,10,17,18 They may not understand the terminology or the importance of relaying all information. Also, adults may not be comfortable sharing certain details in front of their children. Visual aids may be helpful when verbal communication is limited. Use patient education aids with pictures or translate them into the patient’s first language. Dental hygienists can also enroll in language classes to overcome verbal communication barriers most prevalent in their communities.9 Documentation of language barriers, the need for an interpreter at subsequent visits, and use of language-specific materials should be included in patient records. Nonverbal communication includes culturally
acceptable gestures, etiquette, eye contact, physical contact, and methods of listening.9,11,16,17 Dental hygienists should
remain aware of eye contact, maintain a professional physical proximity, and avoid unnecessary bodily touching.9 Different cultures place varying levels of
value on punctuality.10 Addressing appointment time expectations with patients is necessary to avoid missed or rescheduling of appointments. Holidays and religious observance periods of patient populations most commonly seen in a practice should be noted in order to improve scheduling. Also, not all patients wear timepieces, thus medication instructions should be provided based on how patients gauge time change to ensure compliance.
APPLYIMG ETHNIC MNEMONIC
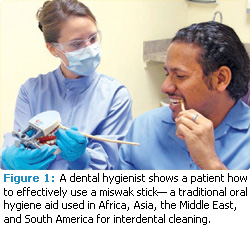
The ETHNIC (explanation, treatment, healers, negotiate, intervention, collaboration) mnemonic (tool to improve memory) helps clinicians provide culturally competent clinical care by increasing communication while the medical history and physical examination are completed (Table 2).9,19,20 The mnemonic prompts questions about health, healing, religion, and symptoms.9 Dental hygienists should inquire about the treatments a patient is currently using, and investigate the safety of any all-natural products, home remedies, and dietary changes the patient has implemented.7 Any patient preferences that are not harmful to oral health should not be targeted for change. The focus should remain on educating patients about harmful habits and promoting healthy behaviors.11 For example, a miswak stick has been used for centuries in parts of Africa, Asia, the Middle East, and South America as an oral hygiene aid and for religious and social purposes.21 As it turns out, the fluoride-impregnated miswak stick is an effective oral hygiene aid with antiplaque and antigingivitis properties (Figure 1).
Dental hygienists can support a patient’s use of the miswak stick while also introducing other oral hygiene aids, eg, the use of floss can be recommended to clean interproximal spaces and for subgingival plaque removal where the miswak stick cannot reach.21,22 Inform the patient of any adverse effects or limitations, and recommend supplement choices.
Patients from other countries visiting or living in the US may choose to use practices taught in their native countries.9,19,20 Healing techniques may not be viewed as a primary approach to curing or illuminating oral health disease, however the patients’ choice to use these therapies should be acknowledged and documented in the patient’s dental record. The ETHNIC mnemonic also supports the negotiation of mutually acceptable treatment options and self-care regimens, as well as the need to agree on appropriate disease interventions. Dental hygienists should incorporate co-therapy strategies and a patient-centered approach to treatment planning.9,19,20
Lastly, the ETHNIC mnemonic emphasizes collaboration, and recognizes a patient’s need for “nurturers”—family members or friends who influence health beliefs, attitudes, and actions—to be involved in the traditional provider-patient dynamic. Patients may decide to include other support persons to help make dental health decisions and to ensure proper treatment is rendered at home.
CONCLUSION
While it is difficult to garner in-depth knowledge of all health-affecting beliefs and practices of every ethnic or cultural group, dental hygienists should be open-minded to culture-specific patient opinions and health beliefs, and acknowledge how the illness affects dental and medical decision making in everyday life.23–25 Patients will then be more comfortable sharing overall health and vital medical history information. Dental hygienists can incorporate helpful tools like ETHNIC to increase communication and elicit responses, including culture-specific information useful for diagnosis and treatment planning.9,19,20 The overall goal of cultural competency is to improve communication, recognize differences that may impact oral health, and develop skills to provide high-quality dental hygiene care to all patients.11,25,26
REFERENCES
- Institute of Medicine of the National Academies. Advancing Oral Health in America Report 2011. Available at: www.iom.edu/Reports/2011/Advancing-Oral-Health-in-America.aspx. Accessed March 16, 2012.
- Rowland ML, Bean CY, Casamassimo PS. A snapshot of cultural competency education in US dental schools. J Dent Educ. 2006;70:982–990.
- US Census Bureau. Overview of Race and Hispanic Origin. Available at: www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed March 16, 2012.
- Institute of Medicine. In the Nation’s Compelling Interest: Ensuring Diversity in the Health-Care Workforce. Washington, DC: The National Academies Press; 2004:25.
- Berlin EA, Fowkes WC Jr. A teaching framework for cross-cultural health care. Application in family practice. West J Med. 1983;139:934–938.
- Tavoc T, Newsom R, DeWald JP. Cross-cultural adaptability of Texas dental hygienists and dental hygiene students: a preliminary study. J Dent Educ. 2009;73:563–570.
- Crosson JC, Deng W, Brazeau C, Boyd L, Soto-Greene M. Evaluating the effect of cultural competency training on medical student attitudes. Fam Med. 2004;36:199–203.
- Winkelman M. Glossary. In: Culture and Health: Applying Medical Anthropology. San Francisco: Jossey-Bass; 2009:430.
- Darby ML, Walsh, MM. Dental Hygiene Theory and Practice. St. Louis: Saunders Elsevier; 2010:56–72.
- Taylor RB. Taylor’s Diagnostic and Therapeutic Challenges: A Handbook. New York: Springer Science and Business Media Inc; 2005:1–15.
- Perez M, Luquis R. Cultural Competence in Health Education and Health Promotion. San Francisco: Jossey-Bass; 2008:2,27–34,112–115.
- Betancourt JR, Green AR, Carrillo JE, Ananeh- Firempong O 2nd. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302.
- Culhane-Pera KA, Reif C, Egli E, Baker NJ, Kassekert R. A curriculum for multicultural education in family medicine. Fam Med. 1997;29:719–723.
- Campinha-Bacote J. The process of cultural competence in the delivery of health care services: a model of care. J Transcult Nurs. 2002;13:181–184.
- Borkowski N. Organizational Behavior in Health Care. Sudbury, Mass: Jones and Bartlett Publishers; 2011.
- Quesada GM. Language and communication barriers for health delivery to a minority group. Soc Sci Med. 1976;10:323–327.
- Ferguson WJ, Candib LM. Culture, language, and the doctor-patient relationship. Fam Med. 2002;34:353–361.
- Kreps G, Kunimoto E. Effective Communication in Multicultural Health Care Settings. Thousand Oaks, Calif: Sage Publications Inc; 1994.
- Dobbie AE, Medrano M, Tysinger J, Olney C. The BELIEF Instrument: a preclinical teaching tool to elicit patients’ health beliefs. Fam Med. 2003;35:316–319.
- Levin SJ, Like RC, Gottlieb JE. ETHNIC: a framework for culturally competent clinical practice. In: Appendix: Useful clinical interviewing mnemonics. Patient Care. 2000;34(9):188–189.
- Baeshen H, Birkhed D. Release of fluoride from fresh and old NaF-impregnated chewing sticks (Miswaks) in vitro and oral retention in vivo. Oral Health Prev Dent. 2010;8:93–99.
- Al-Otaibi M, Al-Harthy M, Gustafsson A, Johansson A, Claesson R, Angmar-Månsson B. Subgingival plaque microbiota in Saudi Arabians after use of miswak chewing stick and toothbrush. J Clin Periodontol. 2004;31:1048–1053.
- US Department of Health and Human Services. National Call to Action to Promote Oral Health. Available at:www.surgeongeneral.gov/topics/oralhealth/nationalcalltoaction.html. Accessed March 16, 2012.
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J, Task Force on Community Preventive Services. Culturally competent health care systems. A systematic review. Am J Prev Med. 2003;24:68–79.
- Commission on Dental Accreditation. Accreditation Standards for Dental Hygiene Education Programs 2007. Available at: www.ada.org/sections/educationAndCareers/pdfs/proposed_dh.pdf. Accessed March 16, 2012.
- Holder-Ballard CB. Cross cultural adaptability of dental hygiene students and faculty. J Dent Hyg. 2006;1:20–21.
From Dimensions of Dental Hygiene. April 2012; 10(4): 58-61.