Treating Children with Spina Bifida
Follow these strategies to provide effective oral health care to pediatric patients with this complex birth defect.
This course was published in the April 2012 issue and expires April 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the different types of spina bifida.
- Describe the guidelines for antibiotic prophylaxis.
- Discuss the need for latex allergy precautions in the dental office.
- List appropriate dental care modifications for patients with spina bifida.
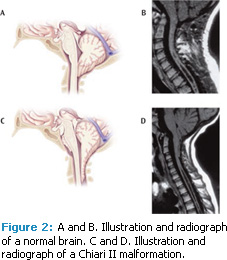
Spina bifida is a neural tube defect that impedes the complete development of the brain, spinal cord, and/or their protective coverings. It is caused by the failure of the fetus’s spine to close properly during the first month of pregnancy (Figure 1).1
The most common birth defect affecting the central nervous system, approximately eight babies are born each day in the United States with some form of spina bifida.2 The causes of this birth defect are unknown, but its risk can be reduced by 70% through adequate supplemental intake of folic acid. All women capable of becoming pregnant should take 0.4 mg of folic acid every day. For mothers who have had previous infants with neural tube defects, a prescription of 4 mg folic acid per day beginning 1 month before conception and continuing through the first trimester of pregnancy is recommended.3
Spina bifida affects people in different ways. Common side effects include hydrocephalus (fluid on the brain), full or partial paralysis, bladder and bowel control problems, learning disorders, depression, latex allergy, and social/sexual difficulties.4 With more than 160,000 people currently living with spina bifida in the US, dental professionals need to be knowledgeable about the special needs created by this birth defect so they can effectively provide oral health care services to this population.4 With advances in treatment, more than 90% of children with spina bifida today will live beyond the third decade of life, and with supportive, comprehensive health care, they can live normal, productive lives.5
Myelomeningocele Spina Bifida
There are four types of spina bifida: occulta, closed neural tube defects, meningocele, and myelomeningocele (Table 1). Myelomeningocele is the most common type and is commonly associated with Chiari II malformation (Figure 2), which consists of the downward displacement of the cerebellar vermis through the foramen magnum; changes in the fourth ventricle; downward displacement of the brainstem with potential for altered pressures on the lower cranial nerves; a smaller, tighter posterior fossa; and a somewhat larger foramen magnum.1,6 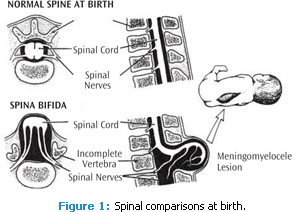
Chiari II malformation presents in one out of three children with myelomeningocele spina bifida. The development of symptoms vary in complexity and may be related to the individual’s age at presentation and the severity of the malformation. These symptoms include difficulty swallowing that leads to poor feeding, weak and poor cry, inspiratory stridor (noise on breathing in) frequently exacerbated by crying, arching of the head, and possible facial weakness in newborns and young infants. The child and adolescent may develop stiffness or spasticity of the arms or hands, which may lead to loss of sensation in the involved extremities. In the younger child, balance control and coordination of movement may be hindered.7
Approximately 70% to 90% of children with myelomeningocele also have hydrocephalus,8 which requires the permanent insertion of a shunt to drain excess fluid from the head to another place where the body can remove it naturally.9 Pediatric neurosurgeons disagree on which shunt is preferred, but the most commonly used is the ventriculoperitoneal (VP) shunt. Table 2 summarizes the various shunt options.9
Updated Guidelines on Antibiotic Prophylaxis
Patients at risk of bacteremia (blood infection), may require antibiotic prophylaxis (AP) before dental treatment. Patients with spina bifida who have ventriculoatrial, ventriculocardiac, or ventriculovenus shunts for hydrocephalus are at risk of bacteremia due to their vascular access. In contrast, VP shunts do not involve any vascular structures and do not require AP. Several factors should be considered before AP is recommended. In consultation with the American Heart Association, the American Academy of Pediatric Dentistry (AAPD) recommends the conservative and judicious use of AP in order to minimize the risk of resistant organism development.10 Table 3 summarizes the AAPD’s statement on AP for dental procedures.10 When treating a patient with a vascular shunt, consulting his or her physician is prudent.10 AP is typically recommended for all dental procedures that involve manipulation of gingival tissue, the periapical region of teeth, or perforation of the oral mucosa. Procedures, such as routine anesthetic injections through noninfected tissue, dental radiographs, placement of removable prosthodontics or orthodontic appliances, adjustment of orthodontic appliances, placement of orthodontic brackets, shedding of deciduous teeth, and bleeding from trauma to the lips or oral mucosa, no longer require AP.10
Risk Management for Latex Allergy
Children with spina bifida are at increased risk of latex allergy, with more than 70% exhibiting symptoms of this potentially dangerous allergy. Why people with spina bifida are predisposed to latex allergy is unknown, although, it is surmised that the more contact a person has with latex, the greater the risk of allergy, as is the case with health care personnel. It may be that because patients with spina bifida often have shunts, other allergies, and need frequent health care, they are at greater risk. Additionally, children with a strong or confirmed allergy to bananas are most likely allergic to latex as well.11 The dental office contains many sources of latex, such as gloves, rubber dams, suction tips, air or water syringes, impression materials, mixing bowls, blood pressure cuffs, gutta-percha, orthodontic rubber bands, and nitrous oxide reservoirs.12 When treating patients with spina bifida in the dental office, a latex-free environment must be maintained. If latex-safe rooms are not available, elective patients should be scheduled for treatment in the morning in order to minimize exposure to airborne latex.11 The use of latex-free equipment and all precautionary measures taken during patient contact should be documented. Signs of an allergic reaction may include: irritated eyes, sneezing and coughing, rash, wheezing, difficulty breathing, and drop in blood pressure. Latex allergy can be fatal so injectable epinephrine should be available and the practice should be well prepared for an emergency.
Oral Care Considerations
Treating children with spina bifida can be challenging, but through modifications in care, dental professionals can provide adequate, efficient, and effective care to this patient population. Prior to the appointment, if the parent or guardian of the patient is concerned about dental anxiety, an antianxiety agent, such as diazepam or lorazepam, can be prescribed. These medications can help the child remain calm during the dental appointment.
During the appointment, a soft beanbag can be placed on the dental chair to help prevent pressure wounds as well as redistribute the pressure on the sensitive vertebrae and areas of insensate skin. Performing an extraoral/intraoral exam can help assess the integrity of the patient’s skin. The six most common risk factors for skin breakdown include reduced mobility, nutritional status, fecal and urinary incontinence, medications that cause a change in sensation or mobility, decreased tissue oxygenation or reduced oxygenated blood, and age.13 Children with spina bifida are at higher risk of wound development and, therefore, should be assessed for skin breakdown at each appointment with results documented in the patient record. Patients with spina bifida who have gastrointestinal and/or tracheostomy tubes need special consideration in order to maintain the airway. They should be placed as upright as possible in the dental chair, and the use of water should be minimized because people with spina bifida often have dysphagia, in addition to a highly sensitive gag reflex. Also, when working with children, regardless of the presence of special needs, a positive atmosphere should be maintained in the clinic and child-friendly language should be used.
Summary
The dental treatment of children with spina bifida involves a team-based multidisciplinary approach to help them achieve optimal health. Due to the complexity of this birth defect, children may hesitate to become more autonomous in daily tasks as they grow and mature. In 2009, Friedman et al found that children with spina bifida tended to be more passive, more dependent on adults for guidance, less likely to make independent decisions, and displayed less intrinsic motivation in school.14 This dependency can be tough on family members who may feel overwhelmed by frequent physician visits and hospitalizations. As a result, oral health care may become less important in relationship to the other health problems exhibited. Oral health professionals must emphasize the importance of performing adequate selfcare and receiving consistent professional dental care, as well as providing support and encouragement to families.
Acknowledgment
The authors would like to thank Elaine Ekmark, RN, MS, spina bifida nurse practitioner at Texas Scottish Rite Hospital for Children, for her assistance with this manuscript.
References
- National Institute of Neurological Disorders and Stroke. What is spina bifida? Available at: www.ninds.nih.gov/disorders/spina_bifida/spina_bifida.htm. Accessed March 16, 2012.
- Fletcher JM, Brei TJ. Introduction: Spina bifida–a multidisciplinary perspective. Dev Disabil Res Rev. 2010;16:1–5.
- Folic acid for the prevention of neural tube defects. American Academy of Pediatrics. Committee on Genetics. Pediatrics. 1999;104:325–327.
- Spina Bifida Association. About spina bifida. Available at: www.spinabifidaassociation.org/site/c.liKWL7PLLrF/b.2642323/k.8E10/Spina_Bifida.htm. Accessed March 22, 2012.
- SpinaBifidaInfo.com. Spina bifida life expectancy. Available at: http://spinabifidainfo.com/life-expectancy. Accessed March 22, 2012.
- Adams RC. Spina bifida: life span management. In: Orthopedic Intervenentions for Pediatric Patients. La Crosse, Wis: American Physical Therapy Association Orthopedic Section; 2000.
- Spina bifida Association. Folic acid. Available at: www.spinabifidaassociation.org/site/c.liKWL7PLLrF/b.2642343/k.8D2D/Fact_Sheets.htm. Accessed March 16, 2012.
- Liptak GS. Spotlight on spina bifida. Available at: www.spinabifidaassociation.org/site/c.liKWL7PLLrF/b.2642343/k.8D2D/Fact_Sheets.htm. Accessed March 16, 2012.
- Dias MS. Hydrocephalus and shunts in the person with spina bifida. Available at: www.spinabifidaassociation.org/site/c.liKWL7PLLrF/b.2642343/k.8D2D/Fact_Sheets.htm. Accessed March 16, 2012.
- American Academy of Pediatric Dentistry. Guideline on antibiotic prophylaxis for dental patients at risk for infection. Available at: www.aapd.org/media/Policies_Guidelines/G_AntibioticProphylaxis.pdf. Accessed March 16, 2012.
- American Latex Allergy Association. AANA latex protocol. Available at: www.latexallergyresources.org/articles-and-brochures. Accessed March 16, 2012.
- Kean T, McNally M. Latex hypersensitivity: A closer look at considerations for dentistry. J Can Dent Assoc. 2009;75:279–282.
- Ekmark EM. Risky business: preventing skin breakdown in children with spina bifida. J Pediatr Rehabil Med. 2009;2:37–50.
- Friedman D, Holmbeck GN, DeLucia C, Jandasek B, Zebracki K. Trajectories of autonomy development across the adolescent transition in children with spina bifida. Rehabil Psychol. 2009;54:16–27.
From Dimensions of Dental Hygiene. April 2012; 10(4): 52, 55-57.