Risk of Ultrasonic Aerosols
Ultrasonic scalers and high-speed handpieces produce more airborne contamination than any other instrument in dentistry.
Ultrasonic scalers and high-speed handpieces produce more airborne contamination than any other instrument in dentistry. Inhalation of airborne particles and aerosols produced during dental procedures may cause adverse respiratory health effects and bidirectional disease transmission. While there are recommended mechanisms that minimize the risk of transmission, many may not be routinely practiced. Oral health professionals need to be aware of the invisible dangers in the operatory and reduce the risk of disease transmission before, during, and after patient care.
Photo Credit: klerik78 / iStock / Getty Images Plus
Bacteria Galore
The oral cavity is inhabited by more than 700 bacterial species. It harbors fungi and viruses from the respiratory tract. Temperature, pH, nutrients, host defenses, and host genetics contribute to microbial growth. Many normal inhabitants of the oral cavity include species of Streptococcus, Actinomyces, Neisseria, Campylobacter, Porphyromonas, Prevotella, Capnocytophaga, and Fusobacteria. The oral microenvironment can be altered by factors such as age, tooth eruption or loss, oral disease status, pregnancy, and drug use. Several of these changes can alter the virulence and pathogenicity of microorganisms.
Photo Credit: blueringmedia / iStock / Getty Images Plus

411 on Aerosols
Potential routes of infection in dental settings are direct and indirect contact, inhalation, and injections/punctures. These routes can be bidirectional where transmission may occur from patient-to-patient, patient-to-clinician, or clinician-to-patient. Inhalation of bioaerosols is considered a moderate risk for disease transmission. Dental patients and personnel are exposed to tens of thousands of bacteria per cubic meter, and the potential to breathe infective material that is aerosolized during routine dental procedures is highly likely. Due to the size, composition, and ability to linger, airborne particles pose an increased health risk.
Photo Credit: draganab / iStock / Getty Images Plus
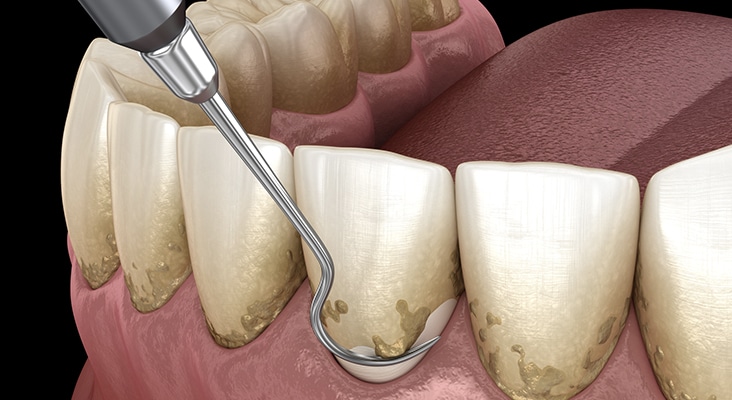
Biofilm Removal
Oral biofilm is resistant to antibiotics, antimicrobial agents, and the body’s immune system; therefore, removal of bacteria in dental biofilms is best achieved by physical disruption, contributing to aerosol production. Aerosols, both visible and invisible, are created during the performance of surgical and nonsurgical dental therapies, which may include extractions, crown preparations, caries restorations, periodontal therapies, prophylaxes, and endodontic therapies. Aerosols consist of water, saliva, blood, debris, and microorganisms (bacteria, fungi, viruses, protozoa) and their metabolites, such as lipopolysaccharides/endotoxins and other toxins.
Photo Credit: alex-mit / iStock / Getty Images Plus
Safety Precautions
Many safety procedures should be incorporated into daily practice to minimize aerosol production, prevent contamination from emitted particles, and reduce transmission of infectious diseases. Minimizing dissemination of aerosols can be accomplished through the use of high velocity air evacuation and preprocedural antimicrobial mouthrinses, flushing waterlines at the beginning of the work day and between each patient, wearing personal protective equipment (PPE), and employing air purifications systems.
Photo Credit: Vectorios2016 / DigitalVision Vectors

High-Volume Evacuation
The high-volume evacuator (HVE) has a large diameter (> 8 mm), which allows for removal of high volumes of air in a short time and reduces the amount of bioaerosols by as much as 90%. The HVE can be challenging to maneuver simultaneously with instrumentation; therefore, most dental hygienists find the saliva ejector easier to use, making it the preferred device for removing excess fluids from the oral cavity. From a practice and safety standpoint, it’s important to note that the opening size of the saliva ejector makes it inadequate for reducing aerosols compared with the HVE or an isolation and evacuation device.
Photo Credit: santypan / iStock / Getty Images Plus

Personal Protective Equipment
Standard precautions involve the use of personal protective equipment (PPE). Primary PPE includes donning proper fitting gloves and surgical masks, protective eyewear with solid side shields or face shield, and protective clothing/disposable gowns. PPE should be worn whenever there is a potential to encounter spray or spatter during patient care and while disinfecting the treatment area, as bioaerosols remain suspended for 30 minutes to 2 hours post treatment. Masks and gloves should be changed between every patient; moreover, all PPE should be changed if torn, wet, or visibly soiled. If providing care for patients with a known infectious disease, the National Institute for Occupational Safety and Health (NIOSH) requires the wearing of a NIOSH-certified particulate-filter respirator. To reduce disease transmission, all PPE must be removed prior to exiting the treatment area.
Photo Credit: Roman Babakin / iStock / Getty Images Plus
Clean Air
Air cleaning systems—such as high efficiency particulate air (HEPA) filters, gas filter cartridges, and electrostatic filters—assist in purifying the air in and outside of dental operatories. The HEPA filter systems direct air through a series of prefilters, which help to continuously catch airborne microorganisms and retain particles as small as 0.3 µm. The four-cylinder gas filter cartridge systems aid in reducing gases and vapors, including mercury, formaldehyde, and glutaraldehyde. The electrostatically charged post-filters/ion emitters aid in purification by reducing dust, particulates, and vapors. Studies show that all three systems have been successful in significantly reducing bioaerosols created during dental procedures, most notably during cavity preparations, tooth extractions, and ultrasonic use.

