
The Blended Approach to Instrumentation
The best patient outcomes are achieved through the tandem use of ultrasonic and hand instrumentation.
This course was published in the November 2016 issue and expires November 30, 2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the blended approach.
- Identify the strengths and weaknesses of ultrasonic and hand instrumentation.
- List the advances in hand instruments designed to improve clinical use and patient outcomes.
- Discuss the clinical applications of the blended approach.
Introduction
Since 1908, Hu-Friedy has been putting the highest quality, most innovative dental products in the hands of dental professionals worldwide. And today, as one of the world’s leading dental instrument companies, we continue our commitment to advancing dental performance by supporting these products with world-class service, support, education, and peer communities. At Hu-Friedy, we have proudly collaborated with private practitioners, dental schools, and leading educators to develop new technologies and quality products that are synonymous with value and performance. At the core is our commitment to helping our customers perform at their best and to improve lives through better dentistry.
This article reviews a clinically optimized approach to improve patient outcomes. It expands clinician understanding of the benefits and restrictions of each technique and explains how to combine them for optimal patient care. By using a balanced approach with both hand and power instrumentation, improved clinical results can be achieved.
Dental hygienists can achieve successful treatment outcomes in nonsurgical periodontal therapy through the combined use of hand and power instrumentation, or the blended approach. Newly engineered designs in both modalities make them more valuable and effective than ever. Today’s dental hygienists have the advantage of providing optimal periodontal patient care through the blended approach to increase clinical success, improve outcomes, and, ultimately, help patients achieve good oral and overall health.
The dental endoscope and dental videoscope, with their subgingival vision, have shown that even after hand and power instrumentation, calculus goes undetected by the explorer and is therefore overlooked.1,2 Research in biofilm, enhanced by the dental endoscope, has established a new paradigm for periodontal therapy, revealing a need for more meticulous and thorough debridement. Studies demonstrate that the presence of inflammation after nonsurgical periodontal therapy usually reveals residual deposits.3,4 Depending on the host response to inflammation, disease will often continue to progress in unresolved areas. In order to reduce chronic gingival inflammation following nonsurgical periodontal treatment, instrumentation must include complete biofilm and calculus removal.5
The American Dental Association sets the standards for procedures with current dental terminology (CDT) codes to achieve uniformity, consistency, and specificity in accurately documenting dental treatment. Initial therapy is typically coded as CDT-D4341 or D4342. The codes D4341 (four or more teeth in a quadrant needing treatment) and D4342 (three or fewer teeth in a quadrant) are designated for therapeutic periodontal scaling and root planing (SRP).6 These codes identify root planing as a definitive procedure to remove rough cementum permeated with calculus or contaminated with microorganisms. SRP is therapeutic, not preventive, and should only be used for patients diagnosed with active periodontitis. Code D4910, or the periodontal maintenance code, includes the removal of supra- and subgingival biofilm and calculus, in addition to site-specific root planing where indicated. Code D1110 defines prophylaxis, a purely preventive procedure, as the removal of plaque, calculus, and stain from the tooth structures.
No matter what code is used, irritants must be removed for tissue resolution. The dental profession regards SRP as the gold standard in the nonsurgical treatment of periodontitis.7–9 One significant question remains: how is this task best accomplished—via ultrasonics, hand instrumentation, or a combination of the two known as the blended approach?
ULTRASONICS
Ultrasonic scalers, when used effectively, can provide many benefits to dental hygienists and patients. Ultrasonic units are available in magnetostrictive or piezoelectric technology. Power instrumentation excels in the removal of biofilm and heavy ledges of supra- and subgingival calculus, leading to decreased bacterial counts and improved tissue health. To achieve the best clinical outcomes when using ultrasonic instrumentation, dental hygienists must meticulously instrument the complete root surface.10,11 This creates a challenge, as the effective use of this modality depends on the dental hygienist’s skill level. Adopting the “fast and easy” mentality using haphazard strokes could potentially result in partial scaling or burnished calculus, leaving biofilm or calculus behind as a reservoir of pathogens. In areas where the ultrasonic insert/tip (UIT) does not touch or strokes are insufficient, the root surface could still harbor embedded calculus and biofilm.10 Some clinicians hold to the misconception that an ultrasonic device used on low power and waved around inside the pocket will deplaque the root surface. While the lavage provides some benefits, it does not dislodge all layers of the biofilm unless the UIT covers every square millimeter of root surface.12 Although ultrasonic instrumentation may seem effortless, its effectiveness depends heavily on proper technique and sufficient time investment. Improper grasp, power level, pressure, adaptation, speed, and stroke can alter the efficacy of the instrument and possibly damage the tooth structure.13 Proper activation and adaptation are fundamental to success. Unlike hand instruments, which are used from an apical to coronal direction, ultrasonic instrumentation is accomplished from the crown to the apex. Effective power scaling requires adapting the terminal 2 mm to 3 mm portion of the UIT to the root surface and using continuous, overlapping strokes at a moderate to slow pace. Using methodical patterns activated in strokes across each surface will assist in attaining complete root coverage.14
For thorough debridement, dental hygienists must spend an adequate amount of time and use a variety of UITs. Research has shown that thorough coverage using ultrasonic instrumentation requires no less time investment than hand instrumentation.15 A combination of horizontal and vertical UIT orientations will provide the best periodontal debridement. The dental endoscope reveals that thorough removal of deposits requires repeated strokes over the same surface because calculus is removed layer by layer.11 If calculus or biofilm persists after therapy, the biofilm recolonizes quickly, within hours, causing inflammation.16,17
It is a myth that ultrasonic scaling sterilizes calculus. Ultrasonic instrumentation disrupts biofilm and flushes out bacteria, but acoustic microstreaming—the flow of water that occurs around the tip of the instrument—does not kill bacteria and periodontal pathogens. Ultrasonic instrumentation adequately applied will not completely eliminate bacteria and pathogens but will reduce their numbers.18
During the 1990s, power scaling became an accepted modality for SRP due to innovations in the shape and diameter of UITs. Advances in the technology behind thin and ultra-thin UIT design changed the dental hygienist’s approach to providing SRP and periodontal maintenance. Today, wide assortments of UITs are available.19
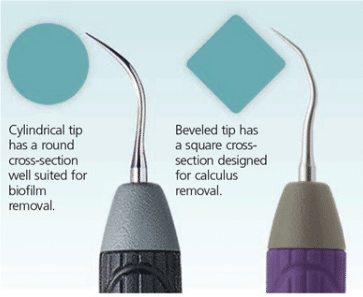
While the majority of UITs are cylindrical in cross section, new additions are square with beveled edges and triple bends that enhance removal of heavy stain and calculus (Figure 1). Due to the surge of an energy wave along the edge, UITs that are triangular, square, or diamond in cross-section are more efficient at removing heavy stain and hard deposits. Adapting the energized edge to the deposit creates microfractures in the calculus, resulting in more efficient removal of hardened deposits.20 Dental hygienists can safely use the new ultra-thin and beveled edge UITs on high power. Without adequate power, the procedure might polish over the outer surface of mineralized deposits because additional energy is required to dislodge mature, tenacious calculus without burnishing.20,21 Cylindrical UITs are more effective for biofilm removal, while UITs with angular shapes or edges are ideal for tenacious calculus and stain (Figure 1). UITs are designed for specific purposes and accessibility; therefore, selection is based on UIT geometry, type, and location of calculus, as well as patient health status and root anatomy.13 This information provides guidance on proper UIT selection in order to complete the job with the least difficulty and most efficiency. The efficacy of ultrasonic instrumentation is based on the meticulous removal of biofilm from the tooth surface and is linked to the skill level of the clinician.22 Extraoral fulcrums assist in providing increased access and adaptation in deep pockets.
ROLE OF HAND INSTRUMENTATION
Hand instruments can be divided into two categories: assessment and treatment.23 Instruments for data collection and tissue assessment include a variety of explorers and probes and are indispensable to the diagnosis and classification of periodontal diseases. Effective treatment requires proper assessment of the contours of the tooth and quantity, quality, and location of calculus, pocket depth, soft tissue, and bone levels. Because subgingival calculus usually forms in rings around the root or in ledges, vertical or oblique exploring strokes with light pressure are best for assessing calculus and cementum through the corresponding vibrational bumps, jumps, and clicks.
Treatment instruments include a wide variety of scalers, such as sickles and curets. Sickles have a cross-sectional shape of a triangle and can be curved or straight. Curets have a cross section of a half-circle, and can be universal or area-specific. The cross section and the internal angulation are important considerations in instrument selection. Other scaling instruments include chisels, files, diamond-coated files, and hoes. For example, Hirschfeld files can be used to break up sheets of residual or burnished calculus especially when applying vertical or oblique strokes. The file has multiple small cutting edges that initially fracture the surface of and then break up burnished calculus that is difficult to remove with other types of bladed instruments.24 Understanding the specific instrument design and the relationship of instrument design to tooth/root anatomy for periodontal debridement will help clinicians achieve successful outcomes.
Many improvements have been made in instrument design. Advances include extended and angled terminal shanks for better access, while others offer shanks with varying degrees of flexibility and rigidity to aid in the debridement of heavy calculus, as well as biofilm removal. Some instruments have unpaired working ends—such as a thin, short sickle for use on lower anterior teeth paired with a rounded disc or hoe, which is useful for extrinsic stain removal. New sickle scalers and area-specific curets feature thin working ends with short, curved blades. Unpaired sickle and curet combinations are also available.23,25
Instrument handles come in a variety of diameters, shapes, padding, weights, and materials. Using hand instruments with different diameter handles can reduce hand stress and repetitive motion injuries. Research suggests that the optimal handle diameter should be at least 10 mm and the optimal weight should be 15 g or less.26 Clinician comfort is the primary consideration. Instruments manufactured with a textured grip surface or surfaces made with materials that increase friction between gloved fingers and the instrument decrease pinch forces.27 Instrument handles come in resin or stainless steel with choices of etched design patterns to prevent slipping and ensure a secure grasp.
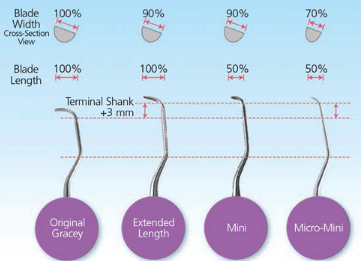
Area-specific (Gracey) curets are available in regular, extended shank, extended shank mini, and micro minis. Extended shanks provide an additional 3 mm in the shank for deep pockets of 5 mm or greater, along with 10% thinner blades for easier insertion. Mini-bladed instruments feature blades that are 10% thinner and 50% shorter than a regular Gracey blade. Rigid mini-bladed Gracey curets with hard, sharp blades are available to aid in scaling tenacious or burnished calculus and do not flex when applying lateral pressure. Mini-bladed Gracey curets provide access to difficult-to-reach areas during nonsurgical periodontal therapy. The small blade enhances subgingival access and helps to prevent unintentional trauma to the epithelial attachment.
When scaling in furcations, narrow pockets, line angles, and buccal or lingual root surfaces, the miniature blades of mini curets provide improved adaptation and tactile sensitivity. For this reason, they are SRP following either ultrasonic or traditional hand scaling. Micro-mini Gracey curets feature blades 50% shorter than standard Graceys, but extra-thin with a 20% thinner blade than the minis. This decrease in bulk allows the micro-mini Gracey curets even greater access to tight, narrow periodontal pockets and complex furcations, line angles, narrow anterior pockets, and root concavities (Figure 2). The shank design is similar to the rigid shank of traditional Gracey curets and is beneficial in removing burnished, tenacious deposits. Basic principles include ensuring the blade extends apically to the calculus deposit in a deep pocket and placing the terminal shank parallel to the surface being instrumented.
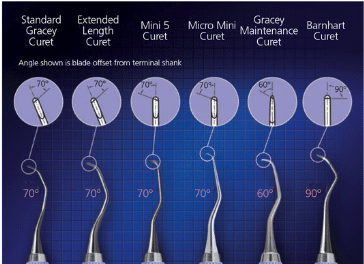
A new area-specific curet, honed at a 60° angle, rather than the traditional 70° Gracey angle, has been developed for periodontal maintenance but can be applied to other applications. These new instruments have shorter, thinner blades than the standard Graceys and they are longer than the mini Gracey curet. They also feature a modified rigid shank 2 mm longer than the standard Gracey (Figure 3). These instruments are designed to provide easy access and insertion under tight tissue in areas with attachment loss. Periodontal maintenance curets may be used to remove biofilm or soft calculus on teeth with tight tissue, recession, or residual pocket depths.
Improved formulations of stainless or carbon steel alloys enable the blades of hand instruments to stay sharp longer. The use of sharp curets is necessary for sensory vibrations to be effectively transmitted from the shank to the finger tips. The advantages of working with sharp instruments also include more efficient working time, less fatigue on the patient and clinician, less discomfort for the patient, reduced pressure or force on the fulcrum, and decreased risk of burnishing deposits.
TANDEM USE OF POWER AND HAND INSTRUMENTATION
The blended approach to instrumentation uses both hand and ultrasonic instruments for effective SRP and debridement procedures during periodontal maintenance.28,29 Biofilm and calculus removal remains the fundamental approach for the resolution of inflammatory periodontal diseases and can be best accomplished with the blended approach. Both types of instrumentation offer unique benefits and both have strengths and weaknesses. For instance, some patients cannot tolerate the temperature or volume of water produced during ultrasonic scaling, while others may have metal sensitivities that preclude the use of hand instruments. The skill of the clinician rather than the type of instrumentation determines efficacy.
The combined use of both modalities enables each method’s strengths to be used.30,31 For example, not all hand instruments easily access the base of deep, narrow pockets. On the other hand, the appropriate UIT can reach the base of deep, narrow pockets more easily. For both hand and power scaling, the correct techniques and appropriate instrument selections to maneuver anatomical concavities and convexities drive optimal patient outcomes.32–34
Both methods require correct patient-operator seating positions. Moving on the stool from the front, side, and back positions of the patient help to maintain neutral body posture. Alternative seating positions and fulcrums, as well as the correct use of the dental light also provide improved ergonomics. Lighted loupes and double-sided mirrors can enhance visual guidance. When choosing hand instruments, clinicians should consider the overall handle size, shape, weight, and maneuverability of the particular instrument in order to reduce force exertion while maintaining neutral wrist positioning. Some ultrasonic UITs and hand pieces offer a swivel feature allowing clinicians to change direction of the tip with greater ease and without interruption.35
CLINICAL APPLICATIONS
When treating plaque-induced gingivitis, clinicians may begin with ultrasonic or hand instrumentation.36 Standard-sized UITs work best when used on heavy deposits, while thin to ultra-thin UITs work better on moderate to light deposits. After power instrumentation is complete, a hand scaler can effectively remove residual calculus or stain. New choices for stain removal include hand instruments paired with sickles and discs. Additionally, there are many choices for posterior interproximal scaling such as the 204 series or a jacquette. Clinicians should then evaluate the tooth surfaces with an 11/12 explorer, followed by polishing and fluoride application, if indicated.19
Treating patients with chronic periodontitis first requires assessment for pain management, followed by removal of supragingival deposits using ultrasonics with standard UITs. Subgingival deposits should then be removed with thin UITs and power levels appropriate to the deposit being removed. Ultrasonic instrumentation requires sufficient power to remove the bulk of the deposit.19 Following the use of thin UITs, the root surfaces should be evaluated with an explorer and debridement continued with hand instruments using universal, then area-specific curets to completely cover root contours.32 For example, the Gracey 17/18, counterpart of the Gracey 13/14, was designed with a deep bend on the lower shank for accessing far distal posteriors while clearing crown interference. The 17/18 Gracey enables clinicians to lower the handle so the patient does not have to open as wide and allows the use of an extraoral fulcrum for the maxillary arch to ensure the terminal shank of the instrument is parallel to the long axis of the tooth. The rounded back minimizes tissue trauma and allows easy insertion to the base of the pocket.
The Gracey 15/16 is the contemporary version of the 11/12, a mesial posterior instrument. When the original 1/2, 3/4, 5/6, 7/8, 9/10, 11/12, and 13/14 area-specific curets were introduced in the 1940s, dentistry was exclusively a stand-up profession. The angle of the mouth accessed by dental hygienists changed with the advent of sit-down dentistry. In response, instrument manufacturers modified posterior curets and developed the 15/16 for mesial posterior surfaces and the 17/18 for distal posterior surfaces. Both modifications allow increased instrument access with a low handle for arch clearance. The design of the shank helps clinicians maintain a neutral position of the hand, wrist, and forearm by decreasing wrist flexion.
The anatomy of the periodontal pocket determines which curet to select. Use extended length curets in deep, wide pockets and use mini and micro-mini curets in narrow pockets. Apply firm lateral pressure for calculus removal and moderate lateral pressure for smoothing the root surface. Controlling pressure is a balance between the instrument grasp and force against the fulcrum and tooth.19,32 Following deposit removal with hand instruments, use UITs on a low setting for final smoothing to remove any smear layer from the root surface. Dental hygienists should avoid over-instrumenting with power and hand scaling and polishing in order to reduce the risk of dentinal hypersensitivity.
SRP should be performed by quadrant or sextant over a number of visits, depending on the severity. Because cases widely vary, establishing specific instrumentation time guidelines is difficult. Timing depends on several variables, including differences in root anatomy that hinder access, tenacity of the deposits, inflammation level, and presence of overhanging margins. Dental hygienists must continue the instrumentation process until all deposits are removed. Even then, case-specific variables, such as patient discomfort, visibility, time allotment, and skill level impact the final result.19 If calculus remains after treatment, biofilm quickly recolonizes on residual deposits, keeping the area inflamed.22 When bleeding on probing is evident at the 4-week to 6-week tissue re-evaluation, dental endoscope studies show residual calculus likely remains, thus preventing the pocket from resolving.3,4
CONCLUSION
New technologies, such as the dental endoscope and dental videoscope, have revealed that a high standard of care is needed to provide acceptable treatment outcomes.37 The best results are achieved by using ultrasonic and hand instruments in tandem. Both require clinical skill and adequate time for the procedure. Thin and ultra-thin UITs, as well as mini and micro-mini curet blades enable access into concavities and convexities as never before. The blended approach to instrumentation joins the advantages of both techniques to best serve clinicians, as well as patients.
REFERENCES
- Osborn JB, Lenton PA, Lunos SA, Blue CM. Endoscopic vs. tactile evaluation of subgingivalcalculus. J Dent Hyg. 2014;88:229–236.
- Blue CM, Osborn J, Lenton P, Lunos S, Poppe K. A pilot study comparing the outcome ofscaling/ root planing with and without Perioscope™ technology. J Dent Hyg. 2013;87:152–157.
- Checchi L, Montevecchi M, Checchi V, Zappulla F. The relationship between bleeding onprobing and subgingival deposits. An endoscopical evaluation. Open Dent J. 2009;28:154–160.
- Wilson TG, Harrel SK, Nunn ME, Francis B, Webb K. The relationship between the presenceof tooth-borne subgingival deposits and inflammation found with a dental endoscope. J Periodontol. 2008;79:2029–2035.
- Osborn JB. The role of the dental endoscope in calculus detection. Dimensions of DentalHygiene.2016;14(2):40–44.
- American Dental Association. Code on Dental Procedures and Nomenclature (CDT Code).Available at: ada.org/en/publications/cdt. Accessed October 13, 2016.
- Drisko CL Periodontal debridement: Still the treatment of choice. J Evid Base Dent Pract. 2014;14S:33–41.
- Sanz I, Alonso B, Carasol M, Herrera D, Sanz M. Nonsurgical treatment of periodontitis. J Evid Base Dent Pract. 2012;12(3 Supp;):76–86.
- Hung HC, Douglass CW. Meta-analysis of the effect of scaling and root planing, surgicaltreatment and antibiotic therapies on periodontal probing depth and attachment loss. J ClinPeriodontol. 2002;29:975–986.
- Matsuda S. The importance of complete root surface coverage. Dimensions of DentalHygiene.2015;13(10):36–39.
- Kiehl N. The keys to effective power instrumentation. Dimensions of Dental Hygiene. 2012;10(7):42,44–48.
- Pattison AM. Ultrasonics unveiled. Dimensions of Dental Hygiene. 2010;8(4):36–45.
- Cox, R. Getting the most out of ultrasonic scaling: A guide to maximizing efficacy. Availableat: dentsply.com/content/dam/dentsply/master/document/ G/ Getting the Most outof UltrasonicScaling-ocdv1gm-en-1509.pdf. Accessed October 13, 2016.
- Matsuda S. Instrumentation of biofilm. Dimensions of Dental Hygiene. 2003;1(1):26–30.
- Pattison A. The right stuff. Dimensions of Dental Hygiene. 2015;13(1):31–37.
- Tan B, Gillam DG, Mordan NJ, Galgut PN. A preliminary investigation into theultrastructure of dental calculus and associated bacteria. J Clin Periodontol. 2004;31:364.
- Haffajee AD, Patel M, Socransky SS. Microbiological changes associated with four differentperiodontal therapies for the treatment of chronic periodontitis. Oral Microbiol Immunol. 2008;23:148–157.
- Fleming TF. Ultrasonics and periodontal pathogens. Dimensions of Dental Hygiene.2007;5(10):14–18.
- Shaklee, R. Modern approach to periodontal debridement. Dimensions of DentalHygiene.2006;4(10):24–27.
- Miller N. How tip geometry impacts performance. In: Ultrasonic Insights. 10th ed.Chicago: Hu-Friedy Manufacturing Co; 2015.
- Matsuda SA. The pathway to synergy. Dimensions of Dental Hygiene. 2008;6(7):24–26.
- Fleming TF. Biofilm removal is the key. Dimensions of Dental Hygiene. 2012;10(4):40-43.
- Bennett B. All about hand instruments. Dimensions of Dental Hygiene. 2007;5(11):20-23.
- Nguyen M. Pattison A. Master the method. Dimensions of Dental Hygiene. 2013;11(11):36,38–40.
- Marcil S. Instrumentation for periodontal care. Journal of Practical Hygiene. 2007;16(4):6-8.
- Simmer-Beck M, Branson B. An evidenced based review of ergonomic features of dentalhygiene instruments. Work. 2010;35:477–485.
- Moravec LJ. Habits for healthy practice. Dimensions of Dental Hygiene. 2012;10(11):42–44.
- Sweeting LA, Davis K, Cobb CH. Periodontal treatment protocol (PTP) for the generaldental practice. J Dent Hyg. 2008;83(Suppl 6):16–25.
- Schaudinn C, Gorur A, Keller D, Sedghizadeh PP, Costerton JW. Periodontitis: anarchetypical biofilm disease. J Am Dent Assoc. 2009;140:978–986.
- Matsuda S. Strategies for success. Dimensions of Dental Hygiene. 2016;14(1):24–26.
- Khosravi M, Bahrami ZS, Atabaki MSJ, Shokrgozar MA, Shokri F. Comparative effectivenessof hand and ultrasonic instrumentations in root surface planing in vitro. J Clin Periodontol.2004;31:160–165.
- Boyd LD, Wilkins EM. Nonsurgical periodontal therapy. In: Clinical Practice of theDental Hygienist. 12th ed. Wilkins EM, ed. Philadelphia: Lippincott Williams and Wilkins;2017:699–737.
- Nguyen M. A closer look at the Gracey 13/14 curet. Dimensions of Dental Hygiene. 2015;13(9):24–30.
- Violante TL, Maddi A. Battling biofilm. Dimensions of Dental Hygiene.2015;13(11):44–49.
- McNitt-Gray JL, Mathiyakom W. Reducing the mechanical demand. Dimensions ofDental Hygiene. 2006;4(3):18–21
- Singh S. Gingival diseases. In: Comprehensive Periodontics for the Dental Hygienist.4th ed. Weinberg MA, Westphal-Theile CM, Froum SJ, Segelnick, SL, eds. Upper Saddle River,New Jersey: Pearson; 2015:102–116.
- Sternberg VM. Call to the dental profession: saving the art of scaling and root planing inperiodontal treatment. Available at: perioimplantadvisory.com/articles/2016/02/call-to-thedental-profession-saving-the-art-of-scaling-and-root-planing-in-periodontal-therapy.html.Accessed October 13, 2016.
From Dimensions of Dental Hygiene. November 2016;14(11):45–50.



