 MKARCO/ ISTOCK/ THINKSTOCK
MKARCO/ ISTOCK/ THINKSTOCK
The Role of Occlusion In the Progression of Periodontal Diseases
Current data suggest that occlusal discrepancies and certain types of occlusal contacts negatively impact periodontal health.
This course was published in the November 2016 issue and expires November 30, 2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the controversial history of the relationship between occlusal contacts and their influence on periodontal disease progression.
- Identify which occlusal contacts contribute to the progression of periodontal diseases.
- Explain the potential problems and benefits associated with the treatment of occlusal discrepancies as part of periodontal therapy.
In the mid-20th century, many studies of cadaver material attempted to show whether occlusion played a role in the progression of periodontal diseases. Glickman and Smulow3 felt that heavy occlusal contacts (occlusal trauma) in the presence of gingival inflammation were a co-destructive force that resulted in deep pockets and more bone loss, while Waerhaug4 argued that all periodontal destruction was associated only with the advancing subgingival plaque front. Extensive animal studies were also performed to try to correlate various forms of occlusal trauma to the progression of periodontal diseases.5,6 The anatomical differences between animals and humans and the types of trauma that were applied to the animals, however, make it difficult to correlate the results of these animal studies to human periodontal disease progression.
The 1996 World Workshop in Periodontics summed up the occlusion research of the 20th century by concluding there was no proof that occlusion played a role in the progression of periodontal diseases and that, with the exception of the treatment of mobility and the presence of parafunctional habits, there was no proof that occlusal treatment was beneficial for the control or treatment of periodontal diseases.7 The World Workshop in Periodontics also recognized that developing an ethical research protocol to determine a definitive answer to the role of occlusion in human periodontal disease progression was impossible. A controlled clinical trial would involve diagnosing periodontal diseases and occlusal discrepancies and then withholding treatment from a portion of the study population.
OCCLUSAL INTERFERENCES
Given the unequivocal statement of the World Workshop on Periodontics that a controlled clinical trial evaluating the role of occlusion in periodontal disease progression in humans was unethical, an effort was made to retrospectively determine the effect of occlusion on the progression and treatment of periodontal diseases. Patient records from a private practice were evaluated to determine if occlusal discrepancies were a risk factor for the progression of periodontal diseases.8,9 These studies were based on assessments of patients who had received periodontal evaluations, including thorough occlusal assessments. Patients then chose whether they wanted to receive complete periodontal treatment or only undergo a portion of the recommended periodontal treatment. The patients voluntarily returned 12 months later for another periodontal and occlusal examination. Some patients diagnosed with periodontal diseases decided not to complete the recommended periodontal treatment. When they returned 12 months later, the progression of the periodontal disease on teeth with occlusal discrepancies was compared with the progression of periodontal disease on teeth that did not have occlusal discrepancies. This allowed for the ethical evaluation of the effects of occlusal discrepancies on the progression of untreated periodontal diseases and, in the cases in which the patients had some treatment performed before dropping out of active therapy, the effect of performing occlusal adjustment on teeth with discrepancies could be evaluated.
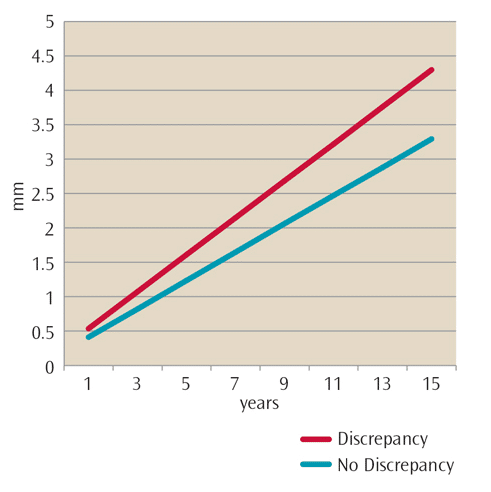
In patients who had no periodontal treatment for 12 months or longer, pocket probing depths continued deepening over time for both teeth that did and did not have occlusal discrepancies (Figure 1). This is expected, as it is well established that untreated periodontal diseases worsen over time. However, the rate of increase in pocket probing depths for those teeth with occlusal discrepancies was statistically significantly higher than the increase in pocket probing depths of those teeth without occlusal discrepancies. This portion of the study gives clear evidence that the presence of an occlusal discrepancy resulted in a more rapid increase in pocket probing depth and that the presence of an occlusal discrepancy negatively influenced periodontal health.8,9
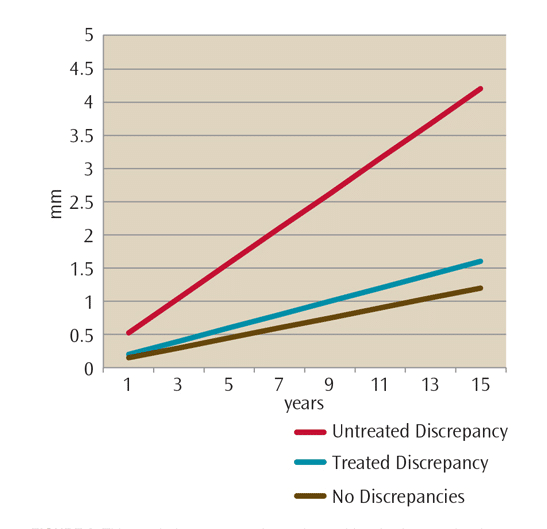
In cases where a portion of the recommended periodontal treatment was performed, patients underwent subgingival root planing with local anesthesia but did not follow through with surgical recommendations. Some patients had also undergone occlusal adjustment. Others had dropped out of treatment before occlusal adjustments were performed. In this partially treated group, all teeth continued to exhibit increasing pocket probing depths (Figure 2) indicating that root planing was inadequate to halt the progression of periodontal diseases in this cohort.10 While the rate of disease progression was slowed in all groups receiving treatment compared to the group that received no treatment, the teeth with untreated occlusal discrepancies had more rapidly increasing pocket probing depths compared with teeth without an occlusal discrepancy or teeth where the occlusal discrepancy had been eliminated by occlusal adjustment. The fact that occlusal adjustment significantly slowed the increase in pocket probing depths indicated that the removal of an occlusal discrepancy yielded a significant treatment benefit for the patient.
In a later study, the effect of occlusal discrepancies on the progression of gingival recession was evaluated.11 While it is a commonly held belief that heavy occlusal contacts result in the loss of gingiva and exposure of the root surface, no correlation between occlusal discrepancies and recession was detected. While some gingival recession was noted at the initial examination, there was no correlation between the existing gingival recession and the occlusal contact on the tooth. Additionally, no increased recession noted over time was related to an occlusal discrepancy. The conclusion of this study was that occlusal discrepancies do not contribute to gingival recession.11
Four studies evaluated teeth that had an occlusal discrepancy vs teeth that did not. For these studies, an occlusal discrepancy was defined as a centric prematurity and/or a nonworking interference. This relatively broad definition was used due to the capabilities of the statistical programs that were available at the time of publication. Due to improvements in statistical programs, it was decided to reevaluate the data that looked at individual occlusal contacts.12 In this study, the effects of premature contacts in centric relation, working contacts, nonworking contacts, combined working and nonworking contacts, and protrusive contacts were evaluated individually (Table 1). Deeper pocket probing depths were noted on teeth that had a centric prematurity, a nonworking contact, a combined working and nonworking contact, or a protrusive contact on a posterior tooth. A working contact without a balancing contact and a protrusive contact on an anterior tooth were not associated with deep pocket probing depths. The pocket probing depths on teeth with a centric prematurity or a nonworking contact experienced a mean increase in pocket probing depth of 1 mm or greater compared with a similar tooth without these contacts. The pocket probing depths associated with the damaging contacts were compared to the known risk factors for periodontal diseases: smoking and poor oral hygiene. In all cases, the mean pocket probing depths associated with the damaging occlusal contacts were statistically deeper than those associated with the known risk factors.
The outcomes of these studies indicate that occlusal discrepancies are a significant risk factor for the progression of periodontal diseases. Also, the studies on the partially treated group indicated that the treatment of occlusal discrepancies was associated with slowing of periodontal disease progression. While these results are not definitive because the studies were not prospective, controlled clinical trials (which would have been unethical to perform), they provide the best data available to date. The results indicate that occlusal relationships should be evaluated in all patients with periodontal diseases and that occlusal therapy should be an integral portion of definitive periodontal therapy.
CLINICAL IMPLICATIONS
The research referenced in the previous section was based on a study of patients with established periodontal diseases. Therefore, the trends and results can only be applied to patients with periodontal diseases. These studies do not necessarily demonstrate the need to adjust occlusal discrepancies among patients with no or mild periodontal diseases. However, if the patient’s periodontal disease does not respond over time to nonsurgical periodontal therapy, occlusal therapy and surgery should be considered.
The most definitive form of occlusal therapy is to permanently change the relationship between the teeth in a manner that eliminates the damaging occlusal contact. This may be accomplished through orthodontic therapy or multiple full-coverage restorations. In patients with advanced periodontal diseases, however, these therapies are usually contraindicated because the long-term prognosis of the teeth cannot be established until the periodontal disease is controlled. During active periodontal therapy, removable devices, such as a biteguard/occlusal stint or definitive occlusal adjustment, can be performed by reshaping the contours of the natural teeth. There are concerns with both of these approaches.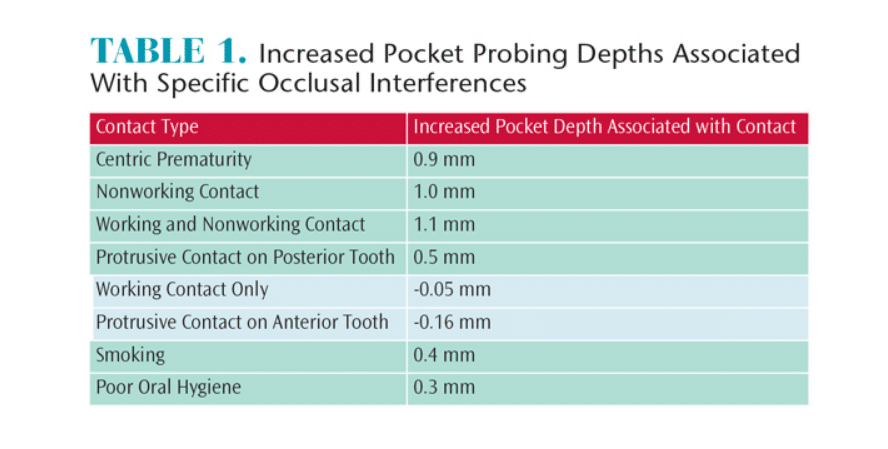
The use of a bite appliance is the least invasive approach to prevent potential damage from occlusal forces. It is completely reversible so that no permanent changes are made to the teeth. If there is a problem with patient acceptance, the appliance can be removed and the patient’s occlusal pattern remains the same as pretreatment. The problem with a removable appliance is that most patients will not wear the appliance during the day and compliance while sleeping varies. If the patient only wears the appliance during sleep at least 50% of the time, the teeth will undergo potentially damaging loading. If the patient bruxes during sleep, then a large portion of the damaging loading may be occurring during sleep. Therefore, the harm from the occlusal pressures caused by parafunctional habits may be avoided by the use of a night guard.
A definitive occlusal adjustment of all teeth is the most predictable approach to relieving damage from occlusal contacts. It permanently removes the occlusal discrepancy and takes pressure off the tooth. Also, this benefit is not dependent on patient compliance. However, performing the extensive tooth reshaping necessary to effectively eliminate damaging contacts from all teeth is a technically difficult procedure that should be approached with caution. While holding high potential benefit for patients, an occlusal adjustment done incorrectly has the potential for serious harm both to the teeth and the periodontium. Additionally, the permanent reshaping of the occlusal surface of the teeth cannot be reversed without extensive prosthetic intervention. Permanent occlusal adjustment of the teeth should be approached with caution and specific training in the adjustment technique is necessary. If the treating dentist is not comfortable with performing a complete occlusal adjustment, the patient should be referred to a specialist.
ROLE OF THE DENTAL HYGIENIST
Dental hygienists are well-positioned to evaluate and record evidence of occlusal stress on the teeth of patients with periodontal diseases. Occlusal stress is illustrated by parafunctional habits such as grinding/clenching, and they may occur as a result of either skeletal or positional misalignment of the teeth. Each patient should be evaluated for signs of occlusal stress, and the findings should be recorded.
The prominent clinical feature of parafunctional habits (grinding/clenching) is the presence of wear on the teeth. The presence of flat spots or wear facets on the teeth is an indication of parafunctional habits that have occurred in the past and that may be ongoing. Obvious wear facets with a shiny surface usually indicate the patient is presently grinding his or her teeth. Wear facets with a dull surface may suggest the patient has been a bruxer in the past but is not currently, or it may mean the patient is an intermittent bruxer. In either case, the findings should be recorded and the possibility of clenching/grinding should be discussed with the patient. Many patients who routinely clench their teeth are not aware of the habit. The first step in educating patients is to show them the wear patterns on their teeth.
If patients are unsure or deny they are bruxers, a series of signs that will help them self-diagnose their parafunctional habit should be given. These include: waking in the middle of the night or in the morning with their teeth clamped together; waking in the morning with the muscles of the face and jaws feeling tired; having “tired teeth” in the morning as if they have been chewing gum all night; or waking up with tenderness or pain in front of the ear. Any of these signs is an indication the patient is grinding/clenching his or her teeth during sleep and that intervention is indicated.
SUMMARY
The role of occlusion in the progression of periodontal diseases remains controversial.13,14 While not definitive due to the inability to perform an ethical controlled clinical trial, current data seem to indicate that occlusal discrepancies and certain types of occlusal contacts contribute to the progression of periodontal disease and that the treatment of occlusal discrepancies has a beneficial therapeutic effect. Thus, occlusal evaluation and treatment, if indicated, should be an integral part of periodontal therapy.
REFERENCES
- Karolyi M, Beobachtungen über pyorrhea alveolaris. Öst. Ung. Vierteeljschr Zahnheilk. 1901;17:279.
- Stillman PR. The management of pyorrhea. Dent Cosmos. 1917;59:405–414.
- Glickman I, Smulow J. The combined effects of inflammation and trauma from occlusion in periodontitis. Int Dent J. 1969;39:101–105.
- Waerhaug J. The angular bone defect and its relationship to trauma from occlusion and downgrowth of subgingival plaque. J Clin Periodontol. 1979;6:61–82.
- Polson A, Zander H. Effects of periodontal trauma on intrabony pockets. J Periodontol. 1983;54:586–591.
- Ericsson I, Lindhe J. Effect of longstanding jiggling on experimental marginal periodontitis in the beagle dog. J Clin Periodontol. 1982;9:497–503.
- Gher M. Non-surgical pocket therapy: Dental occlusion. Ann Periodontol. 1996;1:567–580.
- Nunn M, Harrel SK. The effect of occlusal discrepancies on treated and untreated periodontitis: I. Relationship of initial occlusal discrepancies to initial clinical parameters. J Periodontol. 2001;72:485–494.
- Harrel SK, Nunn M. The effect of occlusal discrepancies on treated and untreated periodontitis II. Relationship of occlusal treatment to the progression of periodontal disease J Periodontol. 2001;72:495–505.
- Harrel S, Nunn M. Longitudinal comparison of the periodontal status of patients with moderate to severe periodontal disease receiving no treatment, non-surgical treatment, and surgical treatment utilizing individual sites for analysis. J Periodontol. 2001;72:1509–1519.
- Harrel SK, Nunn ME. The effect of occlusal discrepancies on gingival width. J Periodontol. 2004;75:98–105.
- Harrel SK, Nunn ME. The association of occlusal contacts with the presence of increased periodontal probing depth. J Clin Periodontol. 2009;36:1035–1042.
- Harrel SK, Nunn ME, Hallmon WW. Is there an association between occlusion and periodontal destruction?: Yes—occlusal forces can contribute to periodontal destruction. J Am Dent Assoc. 2006;137:1380–1384.
- Deas DE, Mealey BL. Is there an association between occlusion and periodontal destruction?: Only in limited circumstances does occlusal force contribute to periodontal disease progression. J Am Dent Assoc. 2006:137:1381–1389.
From Dimensions of Dental Hygiene. November 2016;14(11):41–43.



