Tips for Successful Implant Maintenance
Oral reconstruction and rehabilitation using dental implants in patients with partial and complete edentulism has become extremely common in clinical practice.

Oral reconstruction and rehabilitation using dental implants in patients with partial and complete edentulism has become extremely common in clinical practice. At the same time, patient expectations about the outcomes of implant therapy have also risen. Deeb et al report that 49% of patients who had a consultation expected dental implants to last more than 20 years. While high implant success and survival rates have been reported, the prevalence of peri-implantitis was reported to range from 1% to 47%. In addition, the progression of peri-implantitis follows a nonlinear, accelerating pattern, and the onset of bone loss was usually within 3 years of function among the affected implants. Accordingly, clinicians need to realize there is a wide gap between patient expectations and epidemiologic data. In light of the fact that more than 50% of patients say a dentist is their most significant source of information on implants, clinicians need to present realistic outcomes of implant-supported restorative therapy. Therefore, recognizing risk factors, developing a proper treatment plan, and providing adequate maintenance care at general dental offices are necessary to minimize complications and improve outcomes. Toward this goal, this article will review the risks of implant complications and how oral heath professionals can prevent adverse events..
Photo Credit: CreVis2 / iStock / Getty Images Plus
Determining the Problem
Because most implant complications are multifactorial, it is difficult to identify one specific factor in the clinical setting that can lead to implant failure. Thus, the treatment plan for dental implants must be comprehensive and include a multidisciplinary approach. Each clinician must obtain a complete medical history, followed by extraoral and intraoral examinations—including the assessment of the periodontal and periapical status of existing teeth. Risk of implant failure can be classified into two main groups: systemic conditions and local factors. The diagnosis phase helps clinicians and patients identify many preexisting determinants that could negatively affect the outcome. If any potential causative factors affecting long-term implant success are recognized at this phase, further investigation and discussion of each risk factor is needed..
Photo Credit: peterschreiber.media / iStock / Getty Images Plus

Implant Treatment
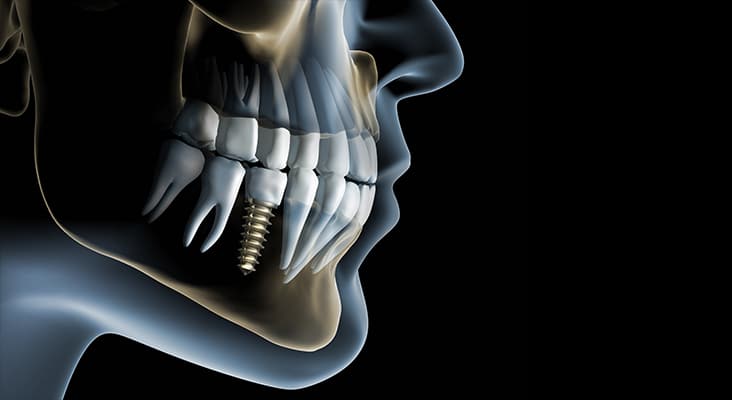
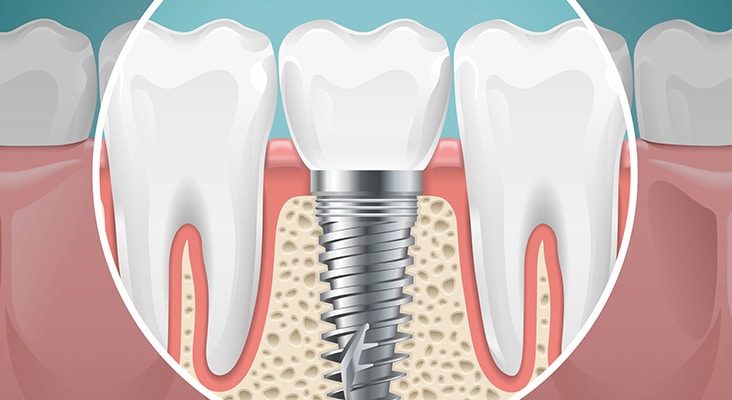
Prior to implant placement, all presenting intraoral pathologic conditions should be treated. These include the treatment of periodontal diseases, endodontic lesions, and caries. Patient compliance with plaque control should be monitored during the initial phase before moving to implant therapy. Once any inflammatory disease has been addressed, an individualized restorative treatment plan should be developed. Three-dimensional (3D) radiographic evaluation using cone-beam computed tomography with a radiographic marker, along with a diagnostic wax-up, are essential steps in this process. These 3D images allow clinicians to assess vital anatomical structures, such as the inferior alveolar nerve, mental foramen, lingual concavity of the posterior mandible, incisive canal, shape and pathological changes of the maxillary sinus, and the endodontic status of adjacent teeth. Implant simulation software is used to evaluate the local anatomical structures and improve clinicians’ understanding of possible future implant positions..
Photo Credit: AlessandroPhoto / iStock / Getty Images Plus
Prosthetic Retention
Both screw- and cement-retained prostheses are acceptable treatment options for single and multiple fixed implant restorations. However, there is debate over which is the better option in the long term. A cement-retained prosthesis has several advantages over a screw-retained prosthesis in terms of cost, ease of fabrication, lack of an access hole (advantageous for a narrow-diameter implant with limited restorative space), and ability to change the angulation of the implant axis by utilizing angled abutments. A systematic review by Wittneben et al compared cement- and screw-retained implant-supported restorations. The 5-year cumulative survival rate of cement-retained reconstruction was 96.03%, while it was 95.55% for screw-retained prostheses. There was no statistically significant difference between the two groups. However, this study revealed that screw-retained fixed prostheses exhibited a slightly lower biological complication rate, such as the presence of fistula/suppuration rates. In addition, the major negative aspect of cement retention is the presence of residual cement following delivery of the prosthesis that can lead to peri-implant mucositis and peri-implantitis. A clinical trial has shown that approximately 80% of the cement-retained implant prostheses with radiological and clinical signs of peri-implant disease had subgingival residual cement. Thus, it was concluded that residual cement might play an important role as a bacterial reservoir, leading to soft tissue irritation that contributes to peri-implant tissue breakdown..
Photo Credit: ONYXprj / iStock / Getty Images Plus

Keys to Implant Maintenance
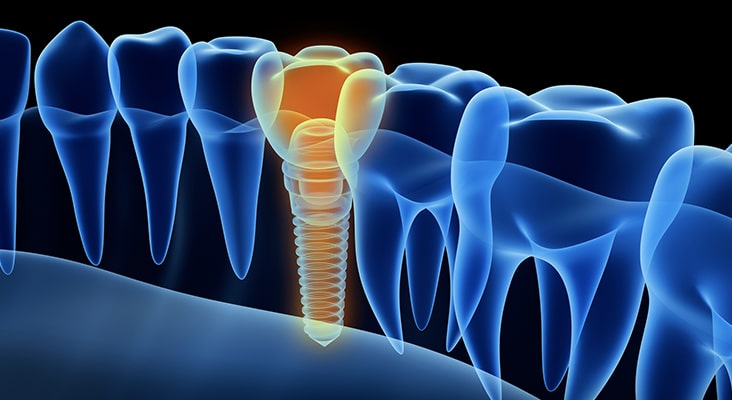
Peri-implant mucositis and peri-implantitis are often associated with an inflammatory reaction to bacterial invasion within the peri-implant tissue. The first signs of peri-implant mucositis include bleeding on probing and/or suppuration, increased probing depth, redness, and swelling. These signs are recognizable upon careful clinical examination. The main purpose of the maintenance protocol for patients with implant-supported restorations is to prevent the onset of inflammatory disease, and, if applicable, halt the progression from peri-implant mucositis to peri-implantitis. This is key, as there are no predictable and reliable methods to treat peri-implantitis. Costa el al showed that subjects who lacked monitoring of the peri-implant tissues and preventive maintenance were associated with a higher prevalence of peri-implantitis than patients who underwent maintenance therapy..
Photo Credit: SeventyFour / iStock / Getty Images Plus
Maintenance Intervals
Because there is no consensus regarding a definitive frequency for maintenance visits, maintenance treatment should be individualized according to each patient’s systemic and local risk factors. For patients with history of periodontitis with acceptable self-care, a 3-month recare interval is usually adequate. On the other hand, when there are no systemic or local risk factors, recare visits might be scheduled every 6 months. If patients still maintain some natural teeth, alternating maintenance therapy between a general dentist’s office and specialist’s office may be beneficial for patients. Careful attention to the presence of inflammation and peri-implant tissue health can help sustain the long-term success of implant-supported restorative treatment..

