Tips to Manage Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) affects approximately 26% of adults between the ages of 30 and 70 in the United States. It occurs when an apnea or hypopnea causes the anatomical structures in the back of the throat (tongue, soft palate, and uvula) to collapse during sleep.

Obstructive sleep apnea (OSA) affects approximately 26% of adults between the ages of 30 and 70 in the United States. It occurs when an apnea or hypopnea causes the anatomical structures in the back of the throat (tongue, soft palate, and uvula) to collapse during sleep. An apnea is a full obstruction of the airway, causing the cessation of breathing for at least 10 seconds. Hypopnea is a partial obstruction of breathing, where the airflow to the lungs is reduced. Due to the obstruction and lack of airflow, the body responds by increasing respiratory effort. The severity of OSA is based on the apnea-hypopnea index (AHI) and/or the respiratory disturbance index (RDI). The AHI is the combined average of apneas and hypopneas occurring in 1 hour. The RDI is the number of apneas, hypopneas, and respiratory-related arousals occurring in 1 hour. Mild RDI/AHI is five arousals to 15 arousals per hour; moderate is 15 arousals to 30 arousals per hour; and severe is more than 30 arousals per hour.
Photo Credit: cherrybeans / iStock / Getty Images Plus

Risk Factors
Adults with a high BMI (≥30 kg/m2) and large neck circumference (>17 inches for men, >16 inches for women) is one of the greatest predictors of OSA. OSA can be present, however, in patients with any BMI and/or neck circumferences. Age is another risk factor for OSA. Men are at increased risk of OSA compared with women. Sleep position also plays a role in OSA prevalence. Research shows that adults with positional OSA had double the number of obstructive events when sleeping in the supine position than when sleeping in the lateral position. Consuming alcohol can raise OSA risk. Patients with hypertension are 30% to 40% more likely to develop OSA than those without hypertension.
Photo Credit: South_agency / E+
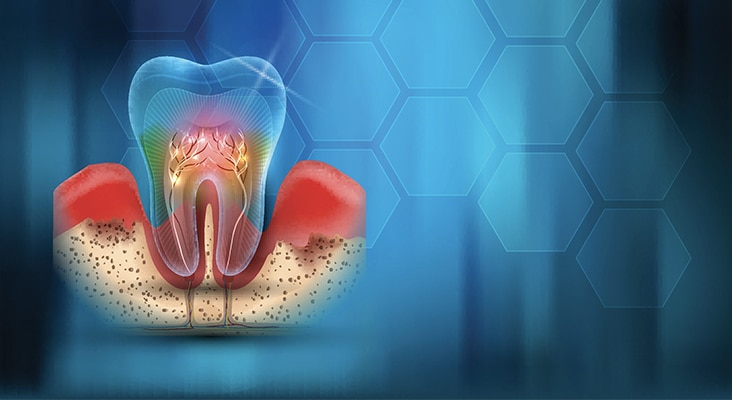
Oral Health Connection
Oral health problems are more common among patients with OSA. While it is a new area of investigation, increasing evidence demonstrates an association between chronic periodontitis and OSA. Adults with moderate and severe chronic periodontitis are four times more likely to develop OSA than adults with mild chronic periodontitis and gingivitis. Adults at high risk for OSA were 73% more likely to develop first-onset temporomandibular joint disorder (TMJ) than individuals at low risk of OSA. A study also showed that 52% of individuals with mild to moderate OSA presented with signs and symptoms of TMD. Sleep bruxism is another oral health problem related to OSA that may serve as a compensating behavior through the pushing of the mandible forward in an attempt to open the airway. Approximately 25% of patients with OSA exhibit sleep bruxism, compared with 5% to 8% in the general population.
Photo Credit: TefiM / iStock / Getty Images Plus

Characteristics
Characteristics commonly associated with OSA include snoring, witnessed cessation of breathing by a bed partner, and excessive daytime sleepiness. Large tonsils, long uvulas, large tongues, and a crowded pharyngeal space are associated with OSA. Large tonsils create a small airway, which is more easily obstructed. A large tongue rests on top of or above the mandibular teeth, causing airflow obstruction when it falls back into the throat during sleep. A thick, broad, and scalloped tongue may be a sign of OSA. A crowded pharyngeal space limits the amount of airflow. Additional signs of OSA are dry mouth, narrow palate, anterior attrition, and retrognathia.
Photo Credit: PobladuraFCG / iStock / Getty Images Plus
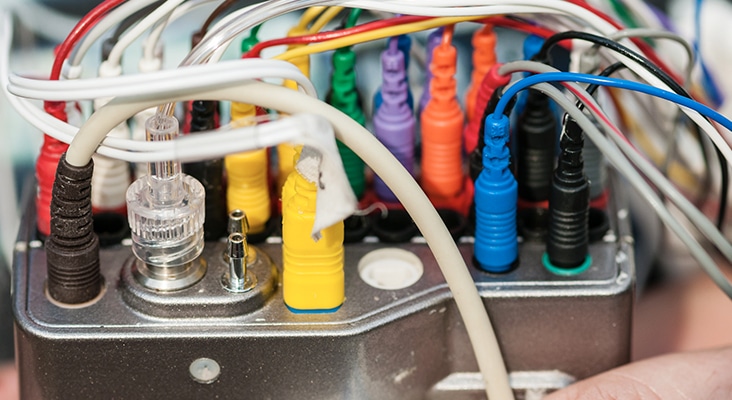
Diagnosis
The definitive diagnosis of OSA is made through polysomnography, an overnight sleep study. A polysomnography is monitored by a sleep technician throughout the night and interpreted by a sleep physician once the study is completed. It monitors a patient’s blood oxygen level, heart rate, brain waves, breathing, and eye and leg movements during sleep. Once the sleep physician interprets the results, he or she determines the diagnosis and severity of the sleep disorder.
Photo Credit: Stephen Barnes / iStock / Getty Images Plus

Positive Airway Pressure
Positive airway pressure (PAP) is the first treatment of choice for patients with OSA. It is a long-term treatment that keeps the airway open via air pressure while sleeping. It can be delivered through continuous positive airway pressure (CPAP), bilevel positive airway pressure (BPAP or BiPAP), or automatic, self-adjusting airway pressure (APAP). A PAP machine uses a mask that either fits over the nose or nose and mouth, a tube that connects the mask to the machine’s motor, and a motor that blows air into the tube to boost airway flow. Today’s PAP machines are lightweight, fairly quiet, and have a success rate of 80% to 95%. Common challenges are mask leaks, loud noise (although this has improved over the years), nasal congestion, xerostomia, claustrophobia, irritation from the mask and straps, and too much air pressure. These challenges can lead to noncompliance and cessation of treatment.
Photo Credit: yokaew / iStock / Getty Images Plus

Oral Appliance
If a patient cannot tolerate PAP, or snores, the physician may refer the patient to an oral health professional who is certified to fabricate and adjust an oral appliance. Once referred, the oral health professional will evaluate the patient’s oral cavity. The patient must receive dental treatment if active disease is present before an oral appliance is made. Oral appliance options consist of mandibular advancement splints (MAS) and tongue-retaining devices (TRD). A MAS engages the mandible and the tongue (indirectly), repositioning the mandible in a forward position. It is made of two acrylic resin pieces covering the maxillary and mandibular arches. An additional part connects two pieces to hold the mandible forward. Appliances can either be titratable or nontitratable. Titratable appliances allow for adjustments to the degree of mandibular protrusion during use, while nontitratable appliances keep the mandible in a fixed state of protrusion. Side effects that occur within the first few days or weeks of MAS therapy are typically minor and may include masticatory muscle or temporomandibular joint discomfort. Side effects occurring 6 months or later after the start of therapy typically result in cessation of the treatment and may include changes in tooth position and occlusion. An aligner should be fabricated in order to avoid these changes in tooth position and occlusion.

