 watanyou / iStock / Getty Images Plus
watanyou / iStock / Getty Images Plus
The Propensity for Gingival Recession
Preventive and maintenance practices are critical to preventing and managing this common periodontal problem.
A lack of attached, keratinized tissue and gingival recession are the most common soft tissue conditions encountered by the dental team. In fact, 50% to 80% of adults present with at least one site of recession.1 Exposed root surfaces compromise esthetics and function, leading to an unfortunate sequela of dentinal hypersensitivity, caries, noncarious cervical lesions, and/or impaired plaque control.
If these defects are not treated aptly, they can worsen and complicate future surgical, restorative, or orthodontic treatment.2 The surgical approach is unique to each patient and differs by etiology of the condition, oral hygiene compliance, and other risk factors. Understanding preventive and maintenance practices is key to preventing and managing gingival recession.
WHAT IS GINGIVAL RECESSION?
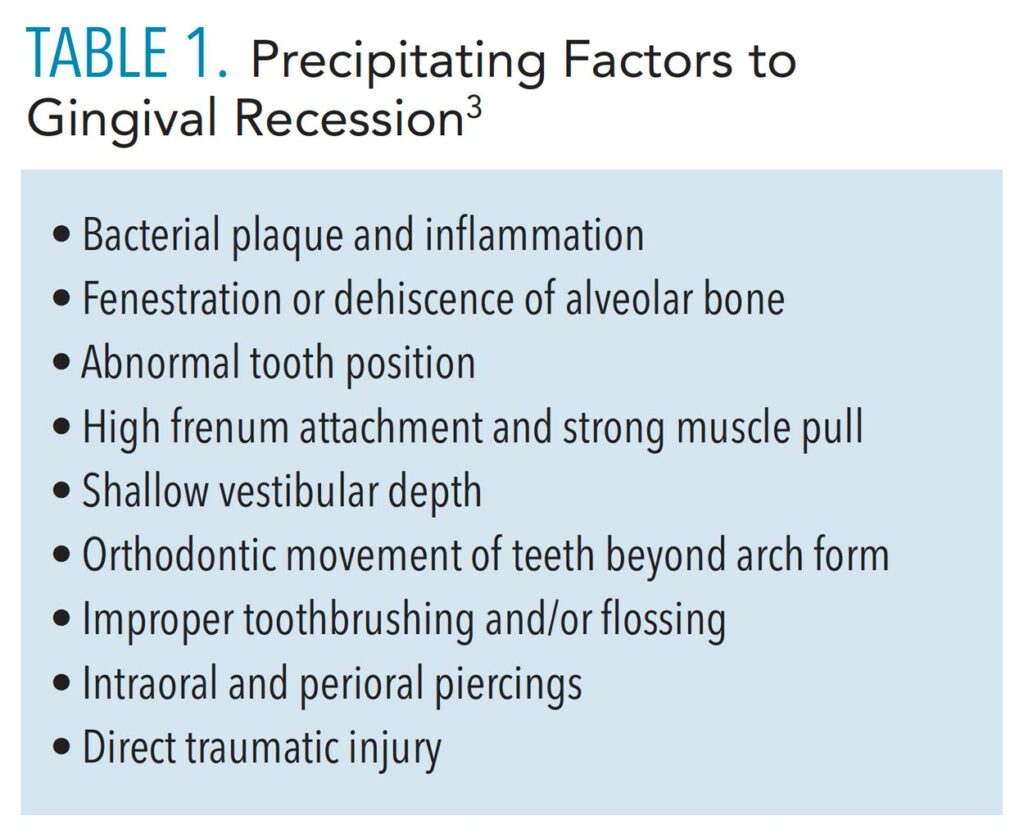
Gingival recession is the apical shift of the gingival margin from the cementoenamel junction.3 Recession can result from bacterial, anatomical, chemical, or mechanical trauma, but the presence of inflammation and bone loss are what truly drive this process. A combination of these factors worsens recession over time (Table 1).3 These factors do not cause recession by themselves, but rather predispose patients to its development.
 The influences of a patient’s phenotype, which considers hard and soft tissue thickness, are also considered. Dehiscence and recession more frequently occur in patients with thin phenotypes, especially after orthodontic treatment.4 If a probe is visualized through the facial gingival sulcus, it is classified as thin.5 This should be documented as part of the initial workup, as it may complicate treatment.
The influences of a patient’s phenotype, which considers hard and soft tissue thickness, are also considered. Dehiscence and recession more frequently occur in patients with thin phenotypes, especially after orthodontic treatment.4 If a probe is visualized through the facial gingival sulcus, it is classified as thin.5 This should be documented as part of the initial workup, as it may complicate treatment.
MINIMIZE RECESSION
Today, a variety of materials and techniques are used to minimize recession. A systematic review of 48 randomized clinical trials with short- and long-term follow-ups found that connective tissue grafts combined with coronally advanced flaps best managed single and multiple recession-type defects with the most significant gain in attachment, keratinized tissue width, and complete root coverage.6 This is often considered the gold standard of root coverage procedures. In this same study, chemical root modification and the type of mechanical debridement did not affect therapeutic outcomes.6
Different chemical agents, including ethylenediaminetetraacetic acid, can be used to decontaminate the root surface, remove the smear layer, and expose the dentin tubules for improved connective tissue re-attachment.7 They can, however, be cytotoxic to wound healing cells at specific concentrations, and should be applied in the appropriate indications.7
REFERENCES
- Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134:220–225.
- Imber JC, KasaJ A. Treatment of gingival recession: When and how? Int Dent J. 2021;71:178–187.
- Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S204– S213.
- Kao RT, Curtis DA, Kim DM, et al. American Academy of Periodontology best evidence consensus statement on modifying periodontal phenotype in preparation for orthodontic and restorative treatment. J Periodontol. 2020;91:289–298.
- De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009;36:428–433.
- Chambrone L, Salinas Ortega MA, Sukekava F, et al. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev. 2018;10:CD007161.
- Blomlöf JP, Blomlöf LB, Lindskog SF. Smear layer formed by different root planing modalities and its removal by an ethylenediaminetetraacetic acid gel preparation. Int J Periodontics Restorative Dent. 1997;17:242–249.
This information originally appeared in Saltz AE, Sirois V. The dental hygienist’s role in treating gingival recession. Dimensions of Dental Hygiene. May 2022; 20(5)32-35.

