A Nonsurgical Approach to Periodontitis
Nonsurgical therapy is considered the gold standard for the initial treatment of inflammatory periodontal disease.
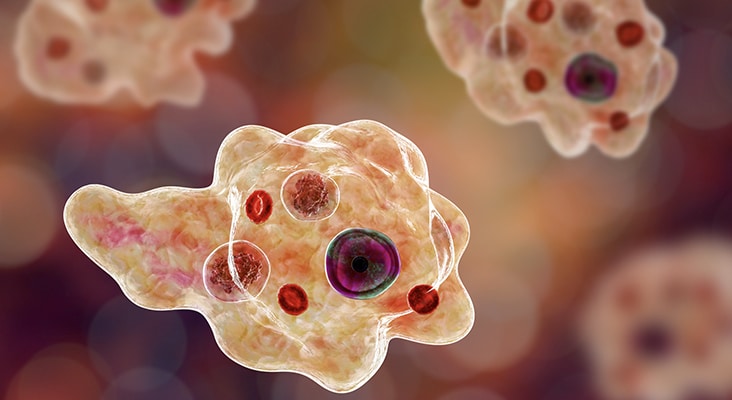
Nonsurgical therapy is considered the gold standard for the initial treatment of inflammatory periodontal disease. Indeed, nonsurgical treatment involving meticulous scaling and root planing has been extensively documented and has been shown to be a highly predictable and successful therapy. The main goals of nonsurgical periodontal therapy (NSPT) are to remove and control supra- and subgingival microbial biofilms, eliminate and control inflammation, and eliminate and control systemic and local risk factors that contribute to disease development and progression. Depending on the degree of bony involvement, effective NSPT may minimize or eliminate the need for surgical intervention.
Photo Credit: Dr_Microbe / iStock / Getty Images Plus

Risk Factors
Several risk factors have well established associations with both periodontal and systemic diseases, such as diabetes, smoking, stress, immunodeficiency, medications, obesity, hormones, and nutrition. For optimal treatment results, systemic risk factors must be modified or eliminated. Some are under the patient’s control, and may, therefore, require lifestyle changes to achieve significant modification. Other more subtle systemic and environmental issues may also need to be addressed to achieve optimal results.
Photo Credit: MangoStar_Studio / iStock / Getty Images Plus

Connection Between Diabetes and Periodontitis
A bidirectional relationship between diabetes and periodontitis has been confirmed repeatedly by other investigators. For a patient with diabetes or a patient suspected of prediabetes, it is imperative to know the individual’s glycosylated hemoglobin level (HbA1c) prior to initiating periodontal treatment. Patients with diabetes and HbA1c values less than 7% are considered well controlled and can be treated in similar fashion to the general population; however, even in these patients, the possibility of delayed healing and infection should be discussed prior to treatment. Patients with diabetes that is poorly controlled should be referred to a medical provider for better metabolic control prior to initiating periodontal therapy. Mutual management of both chronic diseases is vital to attaining stable periodontal health, as well as optimal metabolic control.
Photo Credit: adrian825 / iStock / Getty Images Plus

Smoking
Smokers have a twofold to fourfold greater risk of developing periodontitis. In clinical studies, patients are generally stratified based on the number of cigarettes smoked per day; for example, light (< 10 cigarettes/day), moderate (10 to 19 cigarettes/day), or heavy smokers (≥ 20 cigarettes/day). The risk of developing periodontitis is positively correlated to the number of cigarettes smoked. Prior to initiating nonsurgical periodontal therapy, patients who smoke should be educated about the effects of smoking and encouraged to quit. Studies have reported that smokers exhibit less reduction in subgingival microbial loads and probing depths during NSPT than nonsmoking patients.
Photo Credit: Eva-Katalin / E+

Medication Usage
Roughly 6% to 15% of patients taking a calcium channel blocker, 25% to 30% receiving immunosuppressants, and 50% being treated with antiepileptic drugs will exhibit some degree of drug-induced gingival enlargement. Clinical symptoms of gingival overgrowth are generally seen 1 month to 3 months after initiating drug therapy. For these patients, the medical provider should be consulted to explore the possibility of changing to a different drug category to minimize gingival enlargement. In addition, thorough oral hygiene instruction and appropriate periodontal maintenance intervals need to be established.
Photo Credit: okskaz / iStock / Getty Images Plus

Role of Obesity
The World Health Organization defines obesity as having a body mass index (BMI) ≥ 30 kg/m2. Obesity and BMI are positively correlated to an increased incidence of periodontitis. Further, it appears that obesity can adversely impact periodontal treatment outcomes. Gorman et al reported that as BMI increases by one unit, the rate of alveolar bone loss increases by 5%. Consequently, periodontal patients should be encouraged to adapt a healthy lifestyle to maintain an ideal BMI of < 25kg/m2. Calculation and recording of BMI needs to be incorporated in the comprehensive initial evaluation.
Photo Credit: vadimguzhva / iStock / Getty Images Plus

Importance of Diet
The role of nutrition is well documented in management of chronic systemic illnesses and should be extended to include periodontitis. A diet plan should include high fiber, low carbohydrate, high protein, Omega-3 fatty acids, micronutrients (such as vitamins D, C and B12), and antioxidants (eg, vitamin A, folic acid, and beta-carotene) to optimize periodontal health. Chapple et al demonstrated a statistically significant relationship between the prevalence of periodontal disease and low serum vitamin C levels. Levine et al reported that 200 mg of vitamin C per day could help maintain periodontal health. Compared to a control group, in a study of patients in a periodontal maintenance program, subjects taking ≥ 1,000 mg of calcium and ≥ 400 IU of vitamin D had more shallow probing depths and less gingival inflammation.
Photo Credit: Olga Peshkova / iStock / Getty Images Plus

Eliminating Local Risk Factors
A variety of tooth-related local risk factors can predispose a patient to developing an inflammatory periodontal lesion. These can be grouped into three general categories: anatomical, tooth position, and iatrogenic. While local risk factors are not considered to be a direct cause of periodontitis, they contribute to biofilm development, increased biofilm pathogenicity, and calculus retention. Local risk factors can be modified and/or eliminated—and, in fact, periodontal therapy should not be considered complete until all local risk factors have been addressed.
Photo Credit: SARINYAPINNGAM / iStock / Getty Images Plus

Behavior Modification
Effective plaque control is a requirement in nonsurgical and surgical periodontal therapy. Assessment, motivation, and reinforcement of oral hygiene should be performed at each appointment. Recent research evaluating the association between oral hygiene and periodontitis showed that the risk of periodontitis increased by twofold to fivefold in patients with poor oral hygiene. Self-care instructions need to be personalized and should be recommended based on the severity of the patient’s periodontal status.
Photo Credit: Ridofranz / iStock / Getty Images Plus
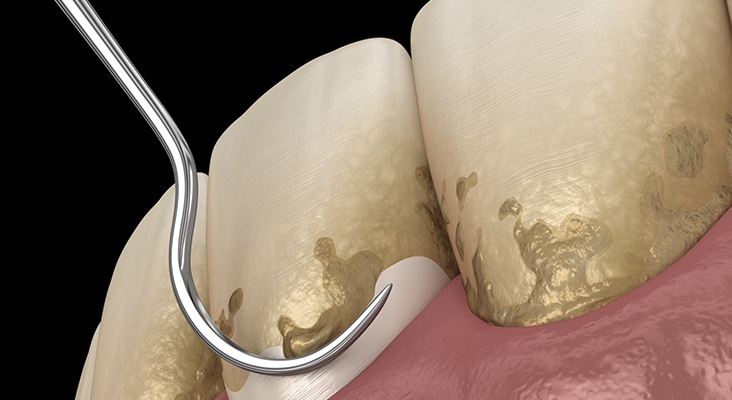
Scaling and Root Planing
Meticulous scaling and root planing is the most critical component of initial periodontal therapy. The primary goals of scaling and root planing are to significantly reduce or eliminate subgingival microbial loads, remove subgingival calculus, remove soft and diseased cementum, and smooth roughened root surfaces. A systematic review reported that average improvement in probing depth following scaling and root planing was 1.29 mm in pockets that had an initial probing depths of 4 mm to 6 mm, and 2.16 mm in pockets of ≥ 7 mm. Gains in clinical attachment levels (CAL) averaged 0.55 mm and 1.19 mm for initial probing depths of 4 mm to 6 mm and ≥ 7 mm, respectively. In most forms of periodontitis, scaling and root planing is highly effective in controlling the signs of periodontal inflammation. However, surgical intervention may be required to definitively treat the bony defects often associated with the moderate and severe stages of periodontitis.
Photo Credit: alex-mit / iStock / Getty Images Plus

Reevaluation
Clinicians are advised that reevaluation is not the end-point of active periodontal therapy—it is part of a decision matrix. Periodontal status should be thoroughly reassessed at 4 weeks to 6 weeks following the nonsurgical phase of treatment, as the greater part of healing is completed by 6 weeks, but collagen maturation might continue for up to 9 months. Post-therapy reevaluation is a critical step in determining the status of gingival inflammation, oral hygiene and healing. Ideal end points for nonsurgical therapy include a decreasing plaque index ≤ 10%, bleeding on probing ≤ 20%, probing depths ≤ 4 mm, mean gain and stability of CAL, maintenance of alveolar bone height, and preservation of form and function of dentition.
Photo Credit: Aja Koska / E+

Periodontal Maintenance
Achieving long-term periodontal stability requires an effective periodontal maintenance program and patient compliance. Maintenance generally includes a reevaluation to determine the patient’s periodontal status, evaluation of systemic and local risk factors, supragingival scaling and polishing, scaling and root planing of residual probing depths—particularly those that exhibit bleeding on probing. The interval between periodontal maintenance appointments should be customized for each patient, based on local and systemic risk factors, severity and extent of periodontal disease, rate of disease progression, and patient compliance. The standard of care for patients who have received definitive treatment for chronic or aggressive periodontitis is a 3-month maintenance interval; however, stable patients can be appointed for longer intervals.

