Managing Periodontal Diseases
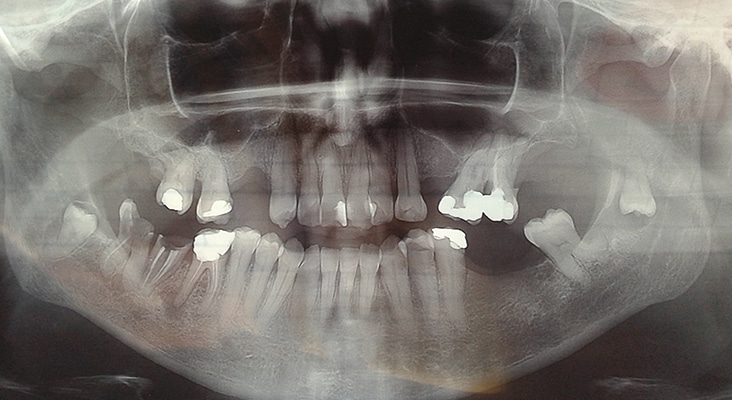
The standard clinical periodontal examination begins with the evaluation of clinical and radiographic signs and symptoms—after taking a medical and dental history—to determine the extent and severity of gingival and periodontal tissue damage.

Standard of Care
The standard clinical periodontal examination begins with the evaluation of clinical and radiographic signs and symptoms—after taking a medical and dental history—to determine the extent and severity of gingival and periodontal tissue damage. With this, the clinical presentation of periodontal disease, or clinical phenotype, follows clinical features of inflammation, redness, edema, and bleeding on probing, and loss of periodontal attachment, as evidenced by probing depth, attachment level, gingival recession, and alveolar bone loss. These recognized techniques alone are insufficient, as they often result in a diagnosis that is inconsistently reproduced or cannot be replicated, as well as an unreliable treatment outcome prognosis. The limited success of prognosis in periodontal disease progression in some patients is due to the clinical appearance not reflecting the biology at the biofilm–gingival interface. Periodontitis is multifactorial, and disease phenotype is expressed due to complex interactions of the bacterial plaque biofilm with the host immune-inflammatory response, resulting in changes in homeostasis of osseous and gingival tissues.
Photo Credit: zlikovec / iStock / Getty Images Plus
Role of Inflammation
Recent evidence-based concepts reveal inflammation is critical in diseases like cardiovascular disease and Alzheimer’s disease, which previously have not been considered inflammatory. Today, inflammatory mechanisms are recognized as integral to the development and progression of most chronic diseases of aging. Environmental and genetic variations interact and account for differences in inflammation among individuals. While inflammation in the body is actively resolved by protective mechanisms that help to restore homeostasis, there are ways to support these processes. Although genes do not change, gene expression in specific tissues can evolve significantly throughout life by factors such as diet, stress, and bacterial accumulations. Abdominal and visceral fat accumulations increase the inflammatory burden on the body, and overexpression of inflammation may be one of the key aspects of aging that influences and links various diseases in individuals.
Photo Credit: Bibica / iStock / Getty Images Plus
Disease Prevention
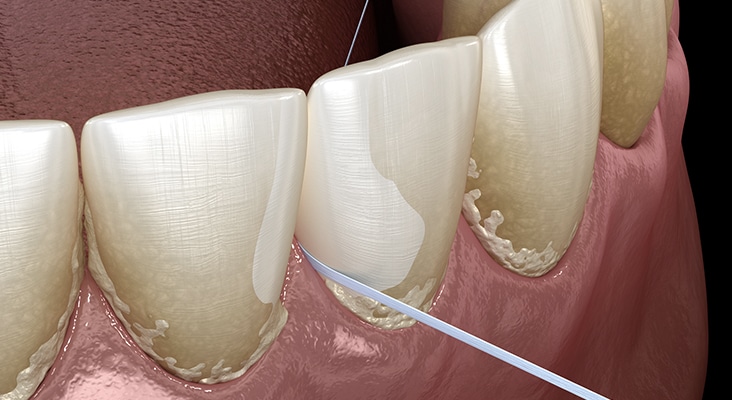
In more than half a century of worldwide translational research and clinical studies, it has been firmly established that effective and persistent removal of dental plaque is conditional to achievement and maintenance of oral health. According to the nonspecific plaque hypothesis, any reduction of the noxious load of plaque and its bacterial byproducts adjacent to gingiva will reduce gingivitis. Gingivitis is the precursor of periodontal disease. As supragingival plaque matures and progresses to subgingival plaque, any decrease in bacterial deposits will prevent gingivitis. The maintenance of noninflamed gingiva will help prevent chronic periodontitis. As the dental biofilm accumulates, oral hygiene helps to control the amount of bacterial deposits on the dental structures and their apical migration. This constitutes primary gingivitis prevention.
Photo Credit: alex-mit / iStock / Getty Images Plus

Oral Hygiene Tools
While patients may have an interdental aid preference, factors such as gingival biotype; anatomy of the embrasure between teeth; tooth location in the dental arch and alignment; and patient’s dexterity, motivation, and compliance should be considered when giving interproximal oral hygiene instructions. Most studies show improvement of plaque scores when comparing patients using interproximal brushes with the use of floss. Two of three studies showed that the regular use of interdental brushes reduced pocket depth more than the use of floss in patients with periodontitis. One study compared interdental brushes with wood sticks and found the interproximal brushes to be more effective in plaque removal. The most effective cleaning is achieved when the biggest brush size that fits into the embrasure is used. As such, patients need to have different brush sizes available to use for anterior teeth and posterior areas. In areas of dental crowding and in young patients where the papillae fill out the embrasures, dental floss is suitable for interdental oral hygiene.
Photo Credit: FotoDuets / iStock / Getty Images Plus

Importance of Patient Education
The research asserts that one single oral hygiene instruction by a dental professional can positively affect the prognosis of periodontitis in a patient for about 6 months afterward. This is in congruence with the 3-month to 6-month recare interval. This confirms the importance of patient education by oral health professionals in the prevention of periodontal disease.

