
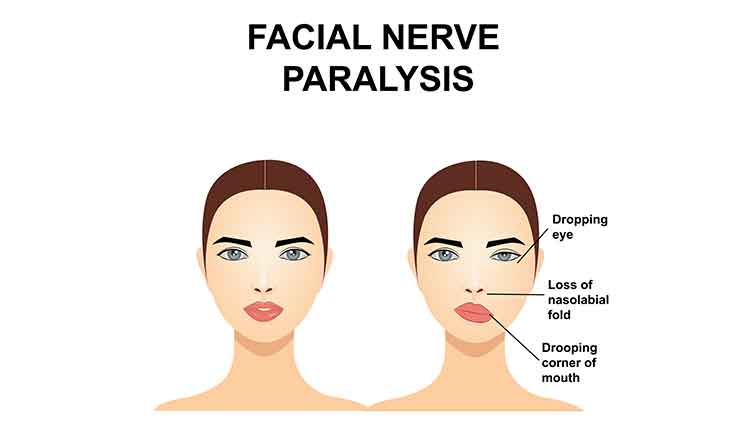
Oral health professionals are likely to see patients who have, or have experienced, facial paralysis, so it is important for clinicians to be aware of its potential causes. While the most common etiologies are Bell’s palsy and trauma, Ramsay Hunt syndrome (RHS) should be included in the differential diagnosis. Caused by reactivation of latent varicella-zoster virus (herpes zoster/shingles) in the geniculate ganglion, RHS presents as facial nerve palsy accompanied by an erythematous vesicular rash on the ear, or in the ear canal or mouth. The rash, which is a cluster of herpetic blisters, can present before, concomitant to, or even after the onset of paralysis. The condition is named after neurologist James Ramsay Hunt, MD, who also described a neuralgia that accompanied the paralysis, located deep in the face or periauricular area. Not surprisingly, RHS can be quite uncomfortable, as it represents a unique presentation of shingles, which is notoriously painful.
Photo Credit: Doucefleur / iStock / Getty Images Plus
Treatment Protocol
The standard-of-care treatment for Bell’s palsy and RHS is combination therapy of a steroid and antiviral medications. Treatment must begin immediately to improve the overall prognosis of the damaged nerves. A common tool to determine the severity of facial nerve damage is the House-Brackmann facial nerve grading scale. Patients are graded according to function of the facial nerve: grade I (100%), II (80%), III (60%), IV (40%), V (20%), and VI (0%). With severe facial palsy, an electroneurography (ENoG) evaluation is recommended to assess the integrity and conductivity of the facial nerve. If the ENoG reports a degeneration of 90% or greater within 14 days, it should be followed by an electromyographic (EMG) confirmation of the muscle cells’ electrical potential.
Photo Credit: Albina Lavrentyeva / iStock / Getty Images Plus

Most Common Modality
One of the accepted treatment modalities is surgical intervention via facial nerve decompression (FND). Gantz et al reported that patients who undergo middle fossa FND for Bell’s palsy can experience significant improvement of normal to near normal return of facial function.
Photo Credit: sframephoto / iStock / Getty Images Plus
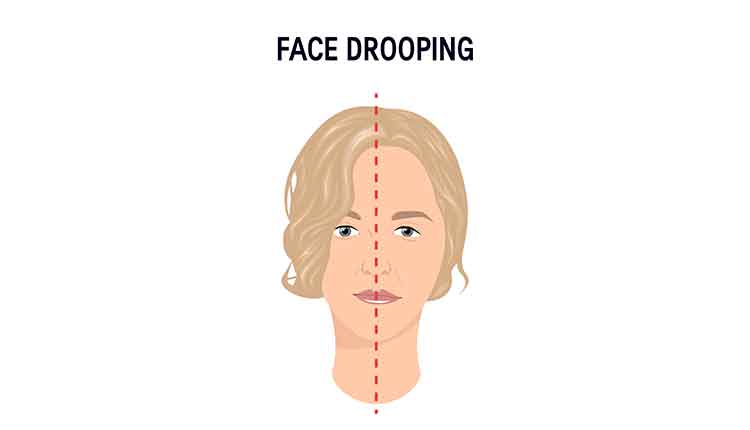
Permanent Damage
As an aggressive disease process that causes facial nerve paralysis, inner ear dysfunction, periauricular pain, and herpetiform vesicles in or around the ear, face, tongue, or palate, RHS can lead to permanent damage to the facial nerve, permanent hearing loss, or continual inner ear issues. Although it presents much like Bell’s palsy, the paralysis can be more severe and patients are less likely to recover completely. The major difference in clinical presentation between RHS and Bell’s palsy is the presence of pain, herpes-type vesicles, and severity of paralysis.
Photo Credit: marina_ua / iStock / Getty Images Plus

Surgical Option
Timing is critical when performing FND surgery, which involves the surgical removal of the bone that is constricting the inflamed, damaged, or diseased nerve. Many times, as in this case study, the nerve is accessed by way of middle fossa craniotomy. Ideally patients with > 90% nerve degeneration and no voluntary EMG motor unit potentials who elect surgery should have the decompression on or before day 14 from onset. A study from the University of Iowa found a greater than 93% probability of achieving a House-Brackmann grade of I (normal) or II (mild dysfunction) if surgery is performed by day 12. If the surgery is completed by day 14, these drop to 82%. Some FND surgeries have been done with some success up until day 21, but the outcome is far less predictable.
Photo Credit: Motortion / iStock / Getty Images Plus

Importance of the Dental Team
Dental teams are frequently the first point of contact for patients with chief complaints involving the tongue, face, or even the ear. It is therefore important for clinicians to be aware of common symptoms—such as facial paralysis and/or ear vesicles—of palsies such as RHS or Bell’s palsy, because the key to successful treatment is timing. Diagnosis and necessary referrals must take place as soon as possible after onset of symptoms. After onset of symptoms, the degree of treatment success, as measured by the level of permanent deformation and/or lack of function of the facial nerve, directly depends on the promptness of treatment.

