Calculus Detection With the Dental Endoscope
The dental endoscope is a subgingival viewing system that includes a fiber optic lens for relaying images, a water irrigation source, imaging electronics, and a monitor.

The Dental Endoscope Defined
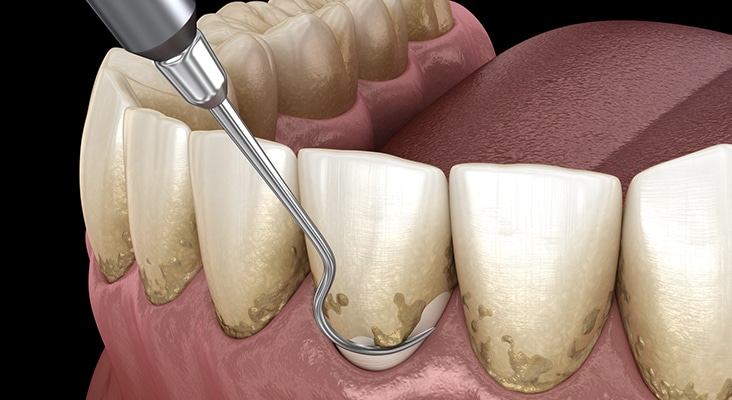
The dental endoscope is a subgingival viewing system that includes a fiber optic lens for relaying images, a water irrigation source, imaging electronics, and a monitor. The fiber optic lens used for capturing and transmitting images is 1 mm in diameter and covered by a single-use sterile sheath for clinical application on each patient. Images are displayed on the monitor for real-time viewing and are magnified 24 times to 48 times, with magnification depending on the proximity of the lens to the imaged tissue. Water flows consistently during use to aid in viewing pocket contents such as sulcular tissues, root surfaces, caries, and deposits. Hand-held metal handles control the position of the fiber optic tip and sheath so the endoscope can be inserted into the sulcus. These handles have multiple shank designs that facilitate access into different sites, much like #11/12 and #13/14 hand curets are designed to access specific areas.
Photo Credit: Ocskaymark / iStock / Getty Images Plus

Technique Approach
In terms of clinical technique, there are two basic approaches to deposit removal when using the dental endoscope: two-handed perioscopy and what Pattison calls the “view, instrument, view” process. While two-handed perioscopy is theoretically more efficient, it requires more experience with the endoscope to achieve mastery. Pattison notes difficulty with this approach because of the tightly restricted spaces that remain when the endoscope and deposit-removal instruments are positioned in the subgingival site. Interpretation of the images also takes training and practice, as they continually change with illumination and magnification. In the “view, instrument, view” technique, the camera is removed from the pocket and the scaling instrument is inserted. This technique precludes visualization while instrumenting the tooth surface, but the ability to see the area post-instrumentation enables thorough calculus removal.
Photo Credit: Lighthaunter / iStock / Getty Images Plus

Evidence Base
Several studies have evaluated the use of the dental endoscope during and after scaling and root planing to add subgingival visual evaluations of calculus removal. Geisinger et al performed scaling and root planing on periodontally involved single-rooted teeth. One of each matched pair was visually examined with a periodontal endoscope for calculus removal and the other was tactilely examined with a hand explorer before extraction. A statistically significant decrease in residual calculus was found when the endoscope was used, especially in deep pockets. A similar study was conducted on multirooted teeth comparing the endoscope with tactile methods of calculus detection before extraction. Use of the endoscope facilitated calculus detection at interproximal sites, but not on facial/lingual surfaces, in furcations, or in deep pockets. In a nonextraction clinical study of periodontally involved teeth, my colleagues and l compared the endoscope with tactile evaluation of calculus immediately post-scaling and root planing and at two subsequent re-evaluation visits 6 weeks to 8 weeks apart. The outcomes indicated that the dental endoscope, while significantly improving calculus detection at all visits, was most beneficial when used during the re-evaluation phase of periodontal therapy.
Photo Credit: wakila / iStock / Getty Images Plus

Role of Inflammation
Patients’ gingival responses after periodontal treatment can provide indirect evidence of how the endoscope performs clinically, while illustrating the role that residual calculus plays in continuing periodontal inflammation. Several studies have examined tissue inflammation, bleeding on probing, and improvement in periodontal tissues. These studies have used the typical parameters of periodontal assessment: pocket depth, attachment level, bleeding on probing, gingival index, plaque index, and calculus index. However, additional indices have been developed for purposes of delineating subgingival findings when using an endoscope, such as endoscopic biofilm index, endoscopic calculus index, and endoscopic gingival index.
Photo Credit: metamorworks / iStock / Getty Images Plus
Thorough Removal
The previous extraction and clinical studies using the dental endoscope highlight the value of subgingival vision during scaling and root planing. Overall, the literature has reported favorable results (compared with blind scaling and root planing) when a dental endoscope is used. Not only is subgingival calculus more thoroughly removed when using an endoscope, but a general improvement in periodontal tissues can be expected. Unfortunately, improved outcomes seem less likely when treating the furcal aspects of multirooted teeth.
Photo Credit: alex-mit / iStock / Getty Images Plus

Practice Makes Perfect
In studies where endoscope use had failed to show improvements compared with control therapies, authors agreed that limitations such as clinician training, experience, and calibration may have contributed to these outcomes. This technology requires hours of practice to achieve competency. Stambaugh estimated that rudimentary skill development for imaging and instrumentation would take approximately 2 months of using an endoscope for 2 hours to 3 hours per week. Overall, there is convincing evidence for using an endoscope as an additional means of ensuring success in periodontal treatment and creating a healthy subgingival environment. Using available technology to provide for more predictable treatment outcomes is a positive step toward advancing the profession, as well as patient care.

