Zooming in on Magnification
A close up look at the use of magnification in dentistry and dental hygiene.
The use of magnification to improve the performance of dental procedures dates back to the late 1800s.1 Over the past decade, magnification in dentistry/dental hygiene has experienced enormous growth. A number of simple and complex magnification systems are now available to dentists and dental hygienists, ranging from simple loupes to the operating microscope.
Improvement in visual acuity has resulted in refinement of techniques in endodontics, periodontics, and restorative dentistry. Ruddle described improved predictability of nonsurgical endodontics in 19942 and Shanelec published numerous innovations in periodontal surgery in the 1990s3-5 using the operating microscope. Leknius and Geissberger at the University of the Pacific School of Dentistry studied the effect of magnification in laboratory and clinical procedures in 1995 and concluded that magnifiers should be required for all dental students due to the dramatic improvement in clinical performance.6
Magnification was originally intended to improve precision in dental procedures but ergonomic benefits are also achieved with magnification. In 2002, Chang discussed the prevention and elimination of chronic neck and back pain in clinicians using appropriate magnification and lighting.7
LOUPES VS MAGNIFICATION
Both loupes and operating microscopes improve visual acuity, enhance postural ergonomics, and decrease eye strain. The operating microscope has the advantages of built in coaxial lighting and variable magnification with the potential for higher magnification than loupes. Loupes have the advantages of being initially easier to use, are less cumbersome, and are far less expensive to purchase than operating microscopes. As a result, loupes really are the modality of choice for dental hygienists.
Dental loupes are the most common magnification system used in dentistry. All loupes have convergent lenses that form a magnified image but there are differences in the optical properties of loupes.
Simple loupes are the most primitive magnifiers with limitations in magnification, working distance, and depth of field, and are not recommended for dental applications. Compound loupes are more sophisticated in design, consisting of multiple lenses and increased refracting power that creates additional magnification, working distance, and depth of field without excessive increases in size and weight. Prism loupes or dental telescopes are the most optically advanced system consisting of low-power telescopes. Prism loupes produce increased magnification with larger fields of vision and greater depth of field than other types of loupes but are heavier and less stable when mounted on glasses at magnifications higher than 3x.
SELECTING AN APPROPRIATE PAIR OF LOUPES
Loupes should be comfortable to wear. Heavy telescopes are uncomfortable and may impede stability and performance. Adjustable loupes mounted on headbands are heavy and inconvenient to use. Lightweight frames with comfortable nose pads should be selected for dental hygiene procedures.
The working distance and the declination angle of the loupes should be adjusted to accommodate the most ergonomic position for the operator. Working distance is the distance from the operator’s eyes to the work site. The working range (or depth of field) of the loupes is the nearest and farthest points between which the site remains in sharp focus. The most favorable ergonomic operator position is such that the hips and forearms are parallel to the floor with the head and the back in comfortable positions.1 The working distance is then calculated by measuring the distance from the eyes to the work site with the operator in an ideal ergonomic position. The working distance and depth of field of the loupes should then be adjusted to match this distance.
The declination angle is the angle formed between the neutral eye position and the actual line of sight to the work site. To select the ideal declination angle, the operator should again assume the most favorable ergonomic position, and the lenses of the loupes should be inclined so that the head does not need to tilt to view the work site.
The magnification power of the loupes should be suited to the work being done. As magnification power is increased, the field of view and depth of field are decreased. Field of view and depth of field can be increased with dental telescopes at magnifications greater than 3x but most dental hygiene procedures can be performed with magnification of no greater than 2.5x, making compound loupes are adequate for dental hygiene.
 Loupes may be fixed to the lenses or adjustable. They may be mounted on the glasses or headband mounted. There are advantages and disadvantages with each configuration.
Loupes may be fixed to the lenses or adjustable. They may be mounted on the glasses or headband mounted. There are advantages and disadvantages with each configuration.
Fixed loupes are permanently mounted in the eyeglass lenses and the mounting should be based on interpupillary distance, working distance, and declination angles as previously discussed. Fixed loupes cannot be adjusted and vision correction must be built into the lenses. If vision changes occur, the loupes must be remade. Low magnification fixed compound loupes are lightweight and convenient to use.
Adjustable loupes give the operator the ability to change the horizontal viewing angle when the clinician changes working positions for various procedures (such as standing to work on patients who don’t want to be reclined). They can be lens mounted or headband mounted. Adjustable loupes are not as convenient as fixed loupes and headband mounted loupes are less comfortable for longer procedures.
Coaxial lighting systems can either be directly mounted to the loupes or to headbands. Lights directly mounted to the loupes keep the illumination parallel with optical axis (the clinician’s line of sight) and are more comfortable than headband mounted lights. Coaxial illumination helps minimize shadows and the need for overhead operatory lights but is somewhat inconvenient and cumbersome. Most dental hygiene procedures do not require the use of coaxial lighting.
When selecting loupes, the clinician should make sure that the proper working distance and declination angle can be integrated for the optimal ergonomic working position.
Compound loupes with the lenses fixed to the eyeglasses and with magnification of 2.5x are ideal for dental hygiene practice. They are comfortable, convenient to use, and less costly than dental telescopes.
DENTAL ENDOSCOPE
Instrumentation of subgingival root surfaces has been done blindly with the clinicians tactile sense the only indication of the presence or absence of root deposits.8 This method is ineffective.9-15 A dental endoscope has been described which gives the clinician direct, real-time visualization and magnification of the subgingival tooth root surface, aiding in the location of deposits on the tooth root.16-17 The inflammatory status of the subgingival soft tissue, including the gingival attachment, sulcus wall, and sulcus contents, can be assessed. Identification and location of subgingival caries, root fractures, tooth root deposits, post perforations, and open restoration margins with the dental endoscope can aid the clinician in diagnosis and therapy.17, 20
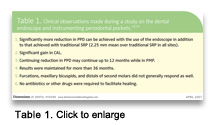 In a retrospective study of 12 patients who had periodontal surgery treatment planned, the efficacy of using the dental endoscope for better debridement of the subgingival root surface was demonstrated.18-19 These patients had 626 periodontal pockets, ranging from 5 mm to 10 mm in depth. These were instrumented with the aid of the dental endoscope. In this study, most periodontal pockets around single rooted teeth healed with significant reduction in probable pocket depth (PPD), an increase in calibrated attachment level (CAL), and the elimination of bleeding on probing.18 The pocket depths continue to be maintained in the 2 mm-3 mm range after more than 3 years of 3-month PMP alone.19 See Table 1 for the clinical observations.
In a retrospective study of 12 patients who had periodontal surgery treatment planned, the efficacy of using the dental endoscope for better debridement of the subgingival root surface was demonstrated.18-19 These patients had 626 periodontal pockets, ranging from 5 mm to 10 mm in depth. These were instrumented with the aid of the dental endoscope. In this study, most periodontal pockets around single rooted teeth healed with significant reduction in probable pocket depth (PPD), an increase in calibrated attachment level (CAL), and the elimination of bleeding on probing.18 The pocket depths continue to be maintained in the 2 mm-3 mm range after more than 3 years of 3-month PMP alone.19 See Table 1 for the clinical observations.
Most clinicians are effectively scaling subgingivally with the endoscope within a few weeks. Regardless of clinicians’ initial skill level and experience, once they begin to use the dental endoscope, their abilities in root instrumentation improve dramatically because clinicians can directly observe the effectiveness of instrumentation with visual confirmation of deposit removal.
The limitations of the dental endoscope are that it takes time and effort to achieve the skill set required to achieve the results reported in the literature.19,20 Also, once the clinician locates the root deposit, the endoscope most often has to be removed from the sulcus and set aside while the clinician instruments the area blindly. However, many sites can be instrumented using a two-handed technique where the endoscope is placed in the sulcus from one side of the pocket and the scaling instrument from the other.
Lasers could be adapted to the dental endoscope to allow removal of root deposits while the deposit is visualized. This would be a significant improvement over the traditional dental endoscope as it would allow immediate removal of the subgingival root deposit when it was discovered, would dramatically reduce the level of clinical skills required for subgingival instrumentation, and increase efficiency as the time required to discover the deposit and remove it would be sharply reduced. Interestingly, a dental endoscope with a laser has been developed for use on horses.21
Unfortunately, the dental endoscope is not currently available and there has been little interest in coupling the laser to a dental endoscope in dentistry. However, the ownership of the dental endoscope has recently changed hands and this may affect its availability in the future.
CONCLUSION
The most frequently used and perhaps the most practical magnification device available for use in dental hygiene clinical practice are dental loupes. Clinicians who use carefully selected and well adjusted dental loupes find them helpful in the practice of dental hygiene.
REFERENCES
- Michaelides P. Use of the operating microscope in dentistry. J Calif Dent Assoc.1996;24:45-50.
- Ruddle CJ. Endodontic perforation repair: using the surgical operating microscope. Dent. Today. 1994;13:49-53.
- Shanelec DA, Tibbetts LS. Periodontal microsurgery. Perio Insights. 1994;3:4-7.
- Tibbetts LS, Shanelec DA. An overview of periodontal microsurgery. Curr Opin Periodontol. 1994;2:187-193.
- Shanelec DA, Tibbetts LS. A perspective on the future of periodontal microsurgery. Periodontol 2000. 1996;11:58-64.
- Leknius C, Geissberger M. The effect of magnification on theperformance of fixed prosthodontic procedures. J Calif Dent Assocl. 1995;23:66-70.
- Chang B.J. Ergonomic benefits of surgical telescope systems: selection guidelines. J Calif Dent Assoc. 2002;30:161-169.
- Stambaugh RV. Perioscopy—the new paradigm. Dimensions of Dental Hygiene. 2003;1(2):12-15.
- Stambaugh RV, Dragoo M, Smith DM, Carasali L. The limits of subgingival scaling. Int J Periodontics Restorative Dent. 1981;1:31-41.
- Nagy RJ, Otomo-Corgel J, Stambaugh RV. The effectiveness of scaling and root planing with curets designed for deep pockets. J Periodontol. 1992;63:954-959.
- Kepic TJ, O’Leary TJ, Kafrawy AH. Total calculus removal: an attainable objective? J Periodontol. 1990;61:16-20.
- Stambaugh RV, McMullin KA. Effectiveness of long term, non-surgical maintenance in deep periodontal pockets. J Dent Res. 1988;67:272.
- Fleischer HC, Mellonig JT, Brayer WK, Gray JL, Barnett JD. Scaling and root planing efficacy in multirooted teeth. J Periodontol. 1989;60:402-409.
- Sherman PR, Hutchens LH Jr, Jewson LG, Moriarty JM, Greco GW, McFall WT Jr. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3-8.
- Buchannan SA, Robertson PB. Calculus removal by scaling/root planning with and without surgical access. J Periodontol. 1987;58:159-163.
- Stambaugh RV, Myers GC, Watanabe J, Lass, C, Stambaugh KA. Visualization of subgingival root surfaces with the dental endoscope. J Dent Res. 2000;79:3656.
- Stambaugh RV, Myers G, Ebling W, Beckman B, Stambaugh K. Endoscope visualization of the subgingival dental sulcus and tooth root surface. J Periodontol. 2002;73:374-382.
- Stambaugh RV, Myers GC, Watenabe J, Lass C, Stambaugh KA. Clinical response to scaling and root planing aided by the dental endoscope. J Dent Res. 2000;79:2762.
- Stambaugh RV. A clinician’s three year experience with perioscopy. Compend Contin Educ Dent. 2002;23:1061-1070.
- Pattison A, Pattison GL. Periodontal instrumentation transformed. Dimensions of Dental Hygiene. 2003;1(2):18-20, 22.
- Tremaine WH. Dental endoscopy in the horse. Clinical Techniques in Equine Practice. 2005;4(2):181-187.
From Dimensions of Dental Hygiene. April 2007;5(4): 16, 18, 20-21.

