Xerostomia from A to Z
Effective detection and treatment guidelines to improve your patients’ quality of life.

Proper salivary flow rate and composition provide lubrication, clearance and dilution of carbohydrates, buffering of acids, and supersaturation of calcium and phosphorus to resist the demineralization of teeth. The disease states associated with loss of salivary gland function demonstrate the crucial role of saliva in the maintenance of oral health.
Etiologies
There are many causes of reduced salivary flow (Table 1).2 More than 400 medications cause xerogenic effects, including antidepressants, antipsychotics, antihistamines, antihypertensives, respiratory inhalers, and sedatives.1,3,4 Medical conditions, such as diabetes, Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, cystic fibrosis, and hormonal imbalances, may also cause xerostomia. Depending on the dose and location, radiation therapy to the head and neck not only decreases salivary flow, but also alters the chemistry of saliva—reducing properties known to protect the oral hard and soft tissues.5 Thyroid malignancies treated with radioactive iodine can also damage the parotid glands.3
Dehydration due to heavy exertion or prolonged exercise is another risk factor. This can cause the loss of salivary buffers needed to protect the oral environment from highly cariogenic beverages, such as sport drinks.6 Similarly, alcoholic drinks are dehydrating, acidic, and may have long-term effects on both salivary function and gastric reflux.5 Alcoholics, bulimics who vomit regularly, and people with gastroesophageal reflux disease have increased oral intrinsic acid and a higher risk of xerostomia due to their altered blood-ion metabolism. Without normal salivary protection, these patients can experience dental erosion and increased caries.
Biologic Processes
Humans have two major salivary glands: the parotid and submandibular glands. The parotid and submandibular glands secrete the most saliva, while the sublingual glands and other glands produce the rest. Salivary secretion is regulated synergistically by both divisions of the autonomic nervous system. Water and electrolyte secretions are regulated by the parasympathetic system, while protein secretion is regulated by the sympathetic system. Hormones also play a minor role in the regulation of salivary glands.7
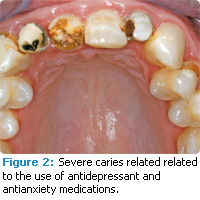
Low salivary pH contributes to an acidic environment in the mouth, and predisposes patients to dental erosion (Figure 1).5,8,9 Changes in the normal ecological balance—due to hyposalivation—promote the proliferation of acid-producing bacteria and rapid demineralization.10 Specifically, a pH below 5.5 increases the likelihood that enamel and dentin will demineralize.
Mucins from submandibular/sublingual saliva have viscoelastic properties that provide lubrication and prevent desiccation. Saliva from these glands also contains histidine-rich proteins that have potent anticandidal effects.2 Patients with diminished salivary function are at risk of denture discomfort and oral candidiasis. These patients often consume a liquid diet or a diet that requires less mastication, and may experience parotid gland atrophy.2 Oral mucosal surfaces become desiccated, which leads to denture sores, inadequate retention of prostheses, and speech difficulties.
Medications that cause xerostomia most frequently alter the neural pathways that stimulate salivary gland secretion.11 Complaints of xerostomia and decreased saliva flow directly correlate to the number of drugs taken. The submandibular gland is more susceptible to medications than the major salivary glands.12 This gland is the major contributor to resting salivary flow and lubrication of the oral cavity. Stimulated parotid saliva during mastication has a watery consistency that aids in mastication.
Symptoms
Salivary hypofunction and xerostomia can disrupt quality of life and result in permanent or temporary intraoral and extraoral disorders. Saliva plays an integral role in taste, digestion, and swallowing. Patients with low salivary flow experience difficulty during the chewing and swallowing of dry food—often requiring extra liquid to facilitate the process. As a result, many patients make poor nutritional food and drink selections in an attempt to mitigate the symptoms. Since saliva stimulates gustatory receptors located on the taste buds, reduced saliva flow inhibits the patient’s ability to identify and recognize several gustatory stimuli.13 Patients with Sjögren’s syndrome or who have undergone head and neck radiation treatment often report dysgeusia (abnormal taste).
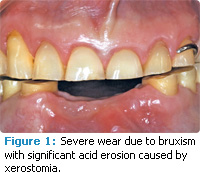
Dental caries is a common consequence of low salivary flow among older adults with restored teeth, gingival recession, and root exposure. Insufficient saliva to restore the baseline oral pH and regulate bacterial populations leads to primary and secondary carious lesions (Figure 2). Since the protective effect of a regular salivary flow is impaired, the mouth lacks calcium, phosphate, and fluoride needed to remineralize hard tissues and the necessary flushing effect to clear debris from the tissues in the oral cavity. All of these factors create the perfect environment for cariogenic bacterial overgrowth that can lead to rampant caries.9
Saliva protects the soft oral tissues from abrasion. In patients with reduced salivary production, traumatic lesions are prevalent. Improper lubrication of the oral mucosa increases the sensitivity of the tissues. Rough or defective restorations with broken margins or poorly fitting prostheses are cofactors in tissue trauma and discomfort of the mucosa. Hyposalivation and xerostomia for patients wearing dentures can impair retention due to the lack of an interface salivary film and reduction in surface tension. Stomatodyna (burning mouth and tongue) and oral ulcerations are common complaints.14,15 Patients with low salivary production are susceptible to candidiasis-associated infections of the mucosal tissue and commissures (angular cheilitis).13 Beyond the medical implications, patients with xerostomia often experience problems speaking and communicating.
Diagnosis and Treatment
Diagnosis of xerostomia can be difficult because patients may experience as much as a 60% reduction of saliva flow and still not complain of “dry mouth.” The best diagnostic aid may be a careful review of patients’ medical histories. The presence of risk factors including medication use (especially antidepressant or antianxiety drugs); systemic problems; or lifestyle issues, such as smoking, alcohol abuse, or dehydration from exercise, increases the likelihood of hyposalivation.
The use of caries management by risk assessment (CAMBRA) is an important tool for patients with xerostomia as they should be classified in the high-risk categories.16
One of the most critical steps for managing xerostomia is establishing the diagnosis, which involves a multidisciplinary team approach. For most patients with hyposalivation and xerostomia, quality of life and overall oral health can be improved with prevention and therapeutic treatments.1 Patients should be instructed about the etiology and possible negative effects of xerostomia and hyposalivation. Effective preventive therapy for dental and oral mucosal disease includes nutrition counseling to avoid a high-sugar diet, acidic foods, caffeine, sodas, and alcohol. Monitoring the patient’s condition every 4 months to 6 months with annual radiographs is imperative to prevent caries and oral mucosa disease.
Clinicians should recommend drinking fluids with food, oral moisturizers, artificial saliva, and the use of a humidifier while sleeping.17 Fluoride varnishes, dentifrices, and outhrinsescan be considered, as well as prescription strength topical fluoride. Standard oral candidiasis infections are treated with topical antifungal medications in different forms: oral rinses, pastilles, ointments, and troches. For immunocompromised patients and those with intractable disease, systemic antifungal treatment should be considered.
Patients wearing dentures should be reminded to remove dentures at night and clean daily with solutions containing benzoic acid, 0.12% chlorhexidine, or 1% sodium hypochlorite, and to apply topical antifungal ointment.17,18 Clinicians should also include alternative products to alleviate symptoms. Saliva substitutes and moisturizing products are available over-the-counter in oral rinses, gels, sprays, and toothpastes. Stimulation techniques are a great aid for patients with functioning salivary tissue. Increased salivary flow has been observed when using sugar-free chewing gum, candies, and mints. Patients should be cautioned about sugar-free candies that might irritate soft tissue such as cinnamon and mint, as well as lemon-flavored candies with citric acids, which may cause caries and dental erosion by lowering the pH of the oral environment.18
Another method of managing xerostomia or hyposalivation is the use of salivary gland stimulants (sialogogues). Two parasympathomimetics drugs—pilocarpine and cevimeline—have been approved by the United States Food and Drug Administration for treatment of xerostomia. Pilocarpine and cevimeline are parasympathomimetic and muscarinic agonists that augment saliva production and are effective in patients with sufficient exocrine tissue.
Pilocarpine is approved for xerostomia caused by Sjögren’s syndrome and radiation therapy, and cevimeline is used to treat Sjögren’s syndrome-related xerostomia.19,20 Prescribing medication for xerostomia will require communication and collaboration with patients’ primary care physicians. In order to mitigate side effects of the systemic medications, the dose or type of medication might need modification. In some cases, drug therapy cannot be adjusted or modified, and alternative options to systemic medications should be considered (Table 2).21
Xerostomia is an important, yet often undiagnosed problem with significant oral health ramifications. Dental hygienists are well poised to diagnose hyposalivation and xerostomia, and provide effective treatment.
References
- Wiener C, Wu B, Crout R, et al. Hyposalivation and xerostomia in dentate older adults. J Am Dent Assoc. 2010;141:279-284.
- Dodds MW, Johnson DA, Yeh CK. Health benefits of saliva: a review. J Dent. 2005;33:223-233.
- Wynn R, Meiller T. Drugs and dry mouth. Gen Dent. 2001;49:10-12,14
- R am S, Kumar S, Navazesh M. Management of xerostomia and salivary g land hypofunction. J Calif Dent Assoc. 2011;39:656-659.
- Young WG . The oral medicine of tooth wear. Aust Dent J. 2001;46:236-250.
- Noble WH, Donovan TE, Geissberger M. Sports drinks and dental erosion. J Am Dent Assoc. 2011;39:233-238.
- Ami S, Wolff A. Implant-supported electrostimulating device to treat xerostomia: a preliminary study. Clin Implant Dent Relat Res. 2010;12:62-71.
- Bartlett D. A new look at erosive tooth wear in elderl y people. J Am Dent Assoc. 2007;138(Suppl):21S-25S.
- Stooky GK. The effect of saliva on dental caries. J Am Dent Assoc. 2008;139(Suppl):11S-17S.
- Takahasi N, Nyvad B. Caries ecology revisited: microbial dynamics and the caries process. Caries Res. 2008;42:409-418.
- Villa A, Polimeni A, Strohmenger L, et al. Dental patients’ self-reports of xerostomia and associated risk factors . J Am Dent Assoc. 2011;142:811-816.
- Wolff A, Zuk-Paz L, Kaplan I. Major salivary gland output differs between users and non-users of specific medication categories. Gerodontology. 2008;25:210-216.
- Spielman A, Ship J. Taste and smell. In: Miles TS , Nauntofte B, Svensson P, eds. Clinical Oral Physiology. Copenhagen, Denmark: Quitessence; 2004:53-70.
- Turner M, Jahangiri L, Ship J. Hyposalivation, xerostomia and the complete denture: a systemic review. J Am Dent Assoc. 2008;139:146-150.
- Takahashi N, Nyvad B. Caries ecology revisited: microbial dynamics and the caries process. Caries Res. 2008;42:409-418.
- Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolf f M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35:703-713.
- Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007;138(Suppl):15S-20S.
- Ram S, Kumar S, Navazesh M. Management of xerostomia and salivary gland hypofunction. J Am Dent Assoc. 2011;39:656-659.
- Berk L. Systemic pilocarpine for treatment of xerostomia. Expert Opin Drug Metab Toxicol. 2008;4:1333-1340
- Chambers MS, Posner M, Jones CU, et al. Cevimeline for the treatment of post-irradiation xerostomia in patients with head and neck cancer. Int J Radiat Oncol Biol Phys. 2007;68:1102-1109.
- Ship JA. Diagnosing, managing, and preventive salivary gland disorders. Oral Dis. 2002;8:77-89.
From Dimensions of Dental Hygiene. January 2012; 10(1): 22, 24, 27-28.